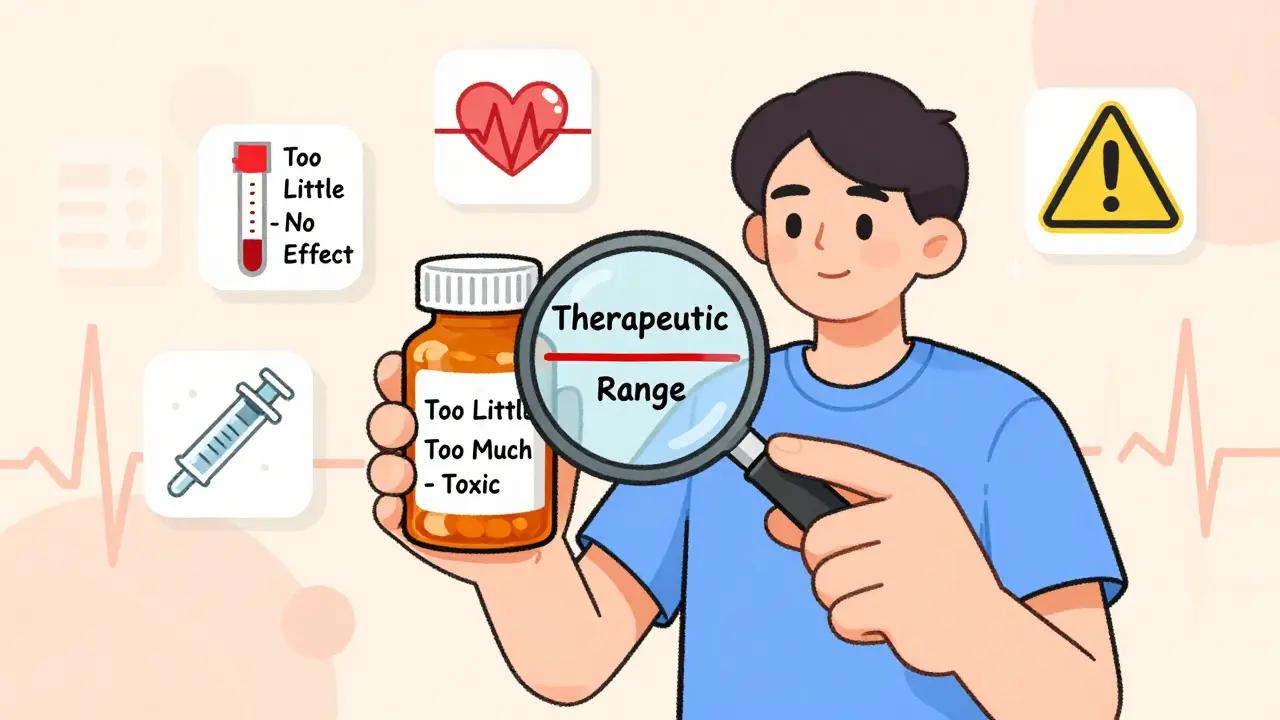
When you take a medication, you expect it to work - not too little, not too much. But for some drugs, that balance is razor-thin. Take narrow therapeutic index drugs (NTI drugs). These aren’t your average pills. A tiny change in dose - even 10% - can mean the difference between healing and harm. Too little, and the drug does nothing. Too much, and it can send you to the hospital. This isn’t theoretical. Real people have bled out from a generic switch. Others have had seizures because their lithium level crept up after a cold. If you’re on one of these drugs, understanding what they are - and how to stay safe - isn’t optional. It’s life-saving.
What Makes a Drug Have a Narrow Therapeutic Index?
Every drug has a sweet spot: the amount in your blood that treats your condition without hurting you. For most medications, that range is wide. You can miss a dose, take it with food, or switch brands, and nothing major happens. NTI drugs are different. Their sweet spot is a narrow band. The gap between the lowest dose that works and the lowest dose that causes harm is smaller than a twofold difference. That means if your blood level rises just 20%, you could cross from safe to toxic.
Think of it like driving a car with no room to steer. If your target speed is 60 mph, and you go 66, you’re speeding. But if you go 54, you’re too slow. With NTI drugs, there’s no 55 or 65 - just 60, plus or minus 3. The FDA defines these drugs as ones where small changes can cause life-threatening reactions or permanent disability. That’s why doctors don’t just prescribe them - they monitor them. Regularly.
Common NTI Drugs You Might Be Taking
You might not realize you’re on an NTI drug. Many are routine prescriptions. Here are the most common ones:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Your INR (a blood test) must stay between 2.0 and 3.0. Above 3.5? Risk of internal bleeding. Below 1.5? Clots can form. A single generic switch has sent people to the ER.
- Lithium (Lithobid): Used for bipolar disorder. Therapeutic level: 0.6-1.2 mmol/L. Above 1.5? Tremors, confusion, seizures. Many patients stabilize only after years of blood tests.
- Digoxin (Lanoxin): For heart failure and irregular heartbeat. Therapeutic range: 0.5-0.9 ng/mL. Over 2.0? Dangerous heart rhythms. Even small changes in kidney function can push levels too high.
- Levothyroxine (Synthroid): For hypothyroidism. TSH levels must be tightly controlled. Switching between generic brands has caused TSH to swing from 1.8 to 8.4 in weeks - leading to fatigue, weight gain, and depression.
- Tacrolimus (Prograf): Used after organ transplants. Too low? Organ rejection. Too high? Kidney failure. Levels are checked daily at first, then weekly.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): Seizure medications. Small changes can trigger seizures or cause dizziness, nausea, or even liver damage.
- Methotrexate (Trexall): Used for autoimmune diseases and some cancers. Toxicity can cause severe bone marrow suppression.
These aren’t rare. About 5-7% of all prescriptions are NTI drugs - but they cause nearly 15% of serious drug-related hospitalizations. That’s why pharmacists in states like North Carolina need your doctor’s approval before swapping generics.
Why Generic Switches Can Be Dangerous
You’ve probably heard that generics are cheaper and just as good. For most drugs, that’s true. But not for NTI drugs.
The FDA allows generics to vary by 80-125% in how much drug gets into your bloodstream compared to the brand. That’s a 45% swing. For NTI drugs, that’s too wide. A 15% difference in absorption could push your lithium level from 1.1 to 1.3 - still in range. But for someone with borderline kidney function, that same 15% could push them to 1.6 - into toxic territory.
Real stories prove this. One patient switched from brand Coumadin to a generic and saw her INR jump from 2.5 to 4.1 in a week. She bled internally and needed emergency treatment. Another patient on levothyroxine switched manufacturers and her TSH went from 1.8 to 8.4. She gained 15 pounds, felt exhausted, and couldn’t focus at work. She didn’t know the problem was her pill - until her doctor checked.
The European Medicines Agency (EMA) already requires stricter testing for NTI generics: 90-111% equivalence instead of 80-125%. The FDA is moving in that direction too. In 2023, they updated guidelines for 15 NTI drugs, including levothyroxine and digoxin, to require tighter bioequivalence standards. But until those rules are fully enforced, your pill could still change - even if your doctor doesn’t know.
What You Must Do to Stay Safe
Being on an NTI drug doesn’t mean you can’t live well. But it does mean you need to be active in your care. Here’s what works:
- Know your drug and its target level. Ask your doctor: “What’s my goal blood level or test number?” Write it down. For warfarin, it’s INR 2.0-3.0. For lithium, it’s 0.6-1.2.
- Stick to one brand or generic. If your pill looks different, ask your pharmacist: “Is this the same as before?” Don’t assume it is. If you’ve been stable on one, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription.
- Get your blood tested on schedule. Warfarin? INR every 1-4 weeks. Lithium? Every 3-6 months, or more if your dose changes. Tacrolimus? Often twice a week after transplant. Skipping tests is like driving blind.
- Track symptoms. Learn the signs of too little and too much. For warfarin: bruising, nosebleeds, dark urine = too much. Swelling, chest pain = too little. For lithium: hand tremors, slurred speech, confusion = too much. Low energy, weight gain = too little.
- Use a medication diary. Record your dose, date, symptoms, and lab results. Patients who do this have 32% fewer problems. Apps like Medisafe or MyThyroid can help - and some are FDA-cleared for NTI drug tracking.
- Watch for interactions. Grapefruit juice? Can raise tacrolimus. Vitamin K-rich foods (kale, spinach)? Can make warfarin less effective. Antibiotics? Can change how your body processes lithium. Always check with your pharmacist before taking anything new.

What’s Changing in 2025-2026
The system is catching up. In 2023, the FDA launched a new initiative to create a formal list of NTI drugs with clear criteria - something it’s never had before. By late 2024, you’ll know exactly which drugs are classified this way.
Also, pharmacogenetic testing is becoming standard. For warfarin, your genes (CYP2C9 and VKORC1) explain up to 60% of how much you need. In 2026, many clinics will test these before prescribing. That means your first dose could be personalized - not guessed.
Hospitals are also installing barcode scanners for 12 high-risk NTI drugs. Before you get a dose, the system checks: Is this the right drug? Right patient? Right dose? It’s like a safety net you don’t even see.
And the numbers are growing. The global market for blood monitoring of NTI drugs will hit $4.7 billion by 2027. Why? Because people are living longer, taking more meds, and we’re learning how dangerous small mistakes can be.
What If You’re Confused or Scared?
You’re not alone. Many patients feel overwhelmed. One Reddit user said: “I used to panic every time my pill looked different.” But after learning how to track her INR and asking for a consistent brand, she hasn’t had a single emergency in five years.
Start small. Ask your pharmacist: “Is this an NTI drug?” Call your doctor and say: “I want to make sure I’m on the right version.” Request your lab results - don’t wait for them to call. Keep a notebook. Use a reminder app. You don’t need to be an expert. You just need to be aware.
NTI drugs aren’t the enemy. They’re tools. And like any powerful tool, they need careful handling. With the right knowledge and habits, you can take them safely - and live well.
Are all generic versions of NTI drugs unsafe?
Not all generics are unsafe, but many are not tested tightly enough. The FDA’s standard allows up to a 45% variation in how much drug enters your bloodstream. For NTI drugs, even a 10-15% change can be dangerous. Some generics meet stricter standards, but you can’t tell by looking. The safest approach is to stay on the same brand or generic you started with - and never switch without talking to your doctor.
Can I switch from brand to generic if my doctor says it’s okay?
Even if your doctor says yes, proceed with caution. A doctor may not know the generic you’re switching to has different absorption rates. Always ask: “Is this the exact same formulation as before?” and request a blood test 2-4 weeks after the switch. Many patients feel fine at first - but their levels change slowly. That’s why monitoring is non-negotiable.
What should I do if I miss a dose of my NTI drug?
Don’t double up. Call your doctor or pharmacist immediately. For warfarin, missing a dose can lower your INR and increase clot risk. For lithium, missing doses can cause levels to drop, then spike if you take two pills later. Each drug has different rules. Your provider will tell you what to do based on your specific medication and health status.
Do I need blood tests forever?
Not forever - but for as long as you’re taking the drug. Once you’re stable, testing frequency may drop (e.g., from weekly to every 3 months). But if you get sick, start a new medication, or change your diet, your levels can shift. Think of it like checking your car’s oil - you don’t do it once and forget it. You check regularly because things change.
Can I use a pill organizer for NTI drugs?
Yes - but only if you use the same brand or generic every time. If you switch products, the pills may look identical but contain different amounts of active drug. A pill organizer is great for remembering doses, but it’s dangerous if you mix different versions. Always check with your pharmacist before putting NTI drugs into a multi-dose tray.
Simon Critchley
February 8, 2026 AT 07:02Bro, NTI drugs are the ultimate game of Russian roulette with your biochemistry. We’re talking about drugs where a 10% shift in absorption can turn your life into a medical drama. Warfarin? One generic switch and suddenly you’re leaking blood internally like a busted radiator. Lithium? Miss your lab by a week and boom - tremors, confusion, seizures. It’s not ‘medication management’ - it’s high-stakes pharmacology Jenga.
The FDA’s 80-125% bioequivalence standard is a joke. That’s a 45% swing! Imagine buying a car that might go 60 mph or 100 mph on the same gas pedal. And don’t get me started on how pharmacists just swap generics like it’s a damn lottery. I’ve seen patients stabilize for YEARS, then get a new bottle that looks identical… and suddenly they’re in the ER with a TSH of 8.4. It’s not negligence - it’s systemic malpractice wrapped in a white coat.
Meanwhile, the EMA’s 90-111% standard is the bare minimum we should’ve had since 1998. The FDA’s 2023 update? Too little, too late. And don’t even mention pill organizers - mixing NTI generics in a tray is like playing tetris with your own organs. If you’re on one of these, you’re not a patient. You’re a lab rat with a prescription.
PS: Use MyThyroid. Track everything. Write it down. Because if you don’t, someone else’s cost-cutting decision will bury you.
Tom Forwood
February 8, 2026 AT 14:40Y’all need to chill. I’ve been on lithium for 12 years, switched generics 3 times, and never had an issue. My doc checks my levels every 4 months, I take it with food, and I drink my water. It’s not magic, it’s medicine. Stop acting like every pill swap is a death sentence.
Also - grapefruit juice? Yeah, bad. But kale? Nah. Vitamin K doesn’t mess with lithium. That’s warfarin stuff. Don’t confuse the two. People panic over stuff they don’t understand. Stay informed, not terrified.
John McDonald
February 9, 2026 AT 21:34Tom’s right - panic doesn’t help. But I’ve also seen people get wrecked by generic switches. My uncle was on digoxin for AFib. Switched to a generic, didn’t get tested for 6 weeks. Ended up in the ICU with ventricular tachycardia. His levels were 2.8. Normal is 0.5–0.9. That’s not a coincidence - that’s a system failure.
Here’s the thing: if your doctor doesn’t know the difference between brand and generic for NTI drugs, they shouldn’t be prescribing them. We need better education. Not just for patients - for docs too. And pharmacists? They need to be forced to flag NTI swaps. No more ‘it’s the same.’ It’s not.
My advice? Always ask: ‘Is this the exact same formulation?’ If they hesitate? Walk out. Get a new pharmacy. Your life isn’t a cost-saving experiment.
Joshua Smith
February 10, 2026 AT 03:04I’ve been on levothyroxine since I was 18. I used to switch brands because my insurance changed. Then I started having panic attacks, weight gain, and brain fog. I didn’t connect it until I read this post. I switched back to Synthroid and asked my doc to write ‘Do Not Substitute.’
My TSH went from 8.1 to 1.9 in 6 weeks. I’m not exaggerating - I went from feeling like a zombie to running 5Ks again. If you’re on an NTI drug and you feel ‘off,’ don’t assume it’s stress. Don’t assume it’s aging. It might be your pill.
Also - yes, pill organizers are fine. Just use ONE brand. Label the tray. Write the name on the container. It’s that simple.
Elan Ricarte
February 10, 2026 AT 20:49Let’s cut through the BS. This isn’t about ‘patient safety’ - it’s about Big Pharma protecting their monopoly. Brand-name Synthroid? $50 a month. Generic? $4. The FDA lets generics slide because they’re too cozy with the manufacturers. Meanwhile, patients are the collateral damage.
That ‘15 NTI drugs updated in 2023’? Please. It’s a PR stunt. They still allow 80-125% variation for 90% of NTI drugs. And don’t tell me ‘monitoring fixes it.’ Who’s gonna pay for monthly blood draws? The uninsured? The underinsured? The elderly on fixed incomes?
Here’s the truth: if you’re rich, you can afford to stay on brand. If you’re poor? You get to gamble with your kidneys, your heart, your brain. This isn’t healthcare. It’s a class war wrapped in a lab coat.
And yes - I’ve seen people die because they couldn’t afford consistent meds. So don’t preach ‘stay informed.’ Tell the FDA to fix the damn system.
Camille Hall
February 11, 2026 AT 01:12Thank you for this. I’m a nurse, and I’ve had patients cry because their pharmacist switched their lithium without telling them. One woman said, ‘I thought I was getting better - then I started hallucinating.’
It breaks my heart. We need a national NTI drug registry. Pharmacies should be required to notify both patient and prescriber when a substitution happens. And insurance companies? They should be forced to cover the brand if the generic causes instability.
Also - if you’re on an NTI drug, ask for a copy of your lab results. Don’t wait for a call. You’re the only one who’s going to notice the shift before it’s too late.
You’re not paranoid. You’re proactive. And that’s everything.
Ritteka Goyal
February 11, 2026 AT 08:51OMG I had no idea! I am from India and here we use so many generics because they are cheap and everyone says they are same! I am on levothyroxine since 2020 and I change brand every time because my insurance changes and I never had any problem! But now I am scared! I think I should go to doctor and ask for Synthroid! My cousin died because of wrong medicine! I think this is very important! I will start tracking my TSH now! Thank you for this post! I am sharing this with my family!
Also - why USA have so many rules? In India we just take pill and go! No blood test! No doctor! Maybe that is why we have more problems? I think USA system is better! Even if it is complicated!
Monica Warnick
February 12, 2026 AT 05:20I’ve been on warfarin for 7 years. I’ve had 3 hemorrhages. I’ve been in the ER twice. I’ve had 11 INR tests in one month. I’ve cried in my car because my pharmacist switched my pills and I didn’t know until I started bleeding from my gums.
My doctor says ‘it’s fine.’ My insurance says ‘switch.’ My pharmacist says ‘it’s the same.’
But I know. I know when I feel different. I know when my skin is too pale. I know when my urine is too dark. I know when my legs feel heavy.
So I stopped trusting everyone. I only take one brand. I write everything down. I call my doctor every time I see a new pill. I don’t care if I look ‘neurotic.’ I’m alive.
And if you’re on an NTI drug and you’re not doing this? You’re playing with fire.
Ashlyn Ellison
February 13, 2026 AT 09:52I switched my levothyroxine brand last year. Didn’t feel anything. Got my TSH checked anyway - went from 2.1 to 6.8. I was asymptomatic. That’s the scary part. You don’t feel it until it’s too late.
Now I only take one brand. I use a reminder app. I keep a notebook. I ask my pharmacist every time. It’s not hard. It’s just… non-negotiable.
Chelsea Deflyss
February 15, 2026 AT 05:47Wow. You all are so dramatic. It’s just a pill. You think you’re special because you have a ‘narrow therapeutic index’? Newsflash: every drug has a therapeutic window. You just don’t understand how to take it.
Stop blaming the system. Start taking responsibility. If you don’t monitor your levels, that’s on YOU. If you don’t ask questions, that’s on YOU. If you don’t read the label, that’s on YOU.
Stop being a victim. Get educated. Or stop complaining.
Alex Ogle
February 16, 2026 AT 02:25I work in a hospital pharmacy. I’ve seen what happens when NTI drugs get switched without warning. One patient - 68, on tacrolimus after a kidney transplant - got a different generic. No one flagged it. His levels dropped. Rejection started. He lost the organ. Died two months later.
His family never knew. The pharmacy chart didn’t note the change. The doctor didn’t check. The patient didn’t know.
That’s not an outlier. It’s systemic. We need mandatory barcode scanning for ALL NTI drugs at the point of dispensing. We need real-time alerts to prescribers. We need a national NTI registry.
And until then? If you’re on one of these drugs - don’t just ‘be careful.’ Be obsessive. Because no one else will be.