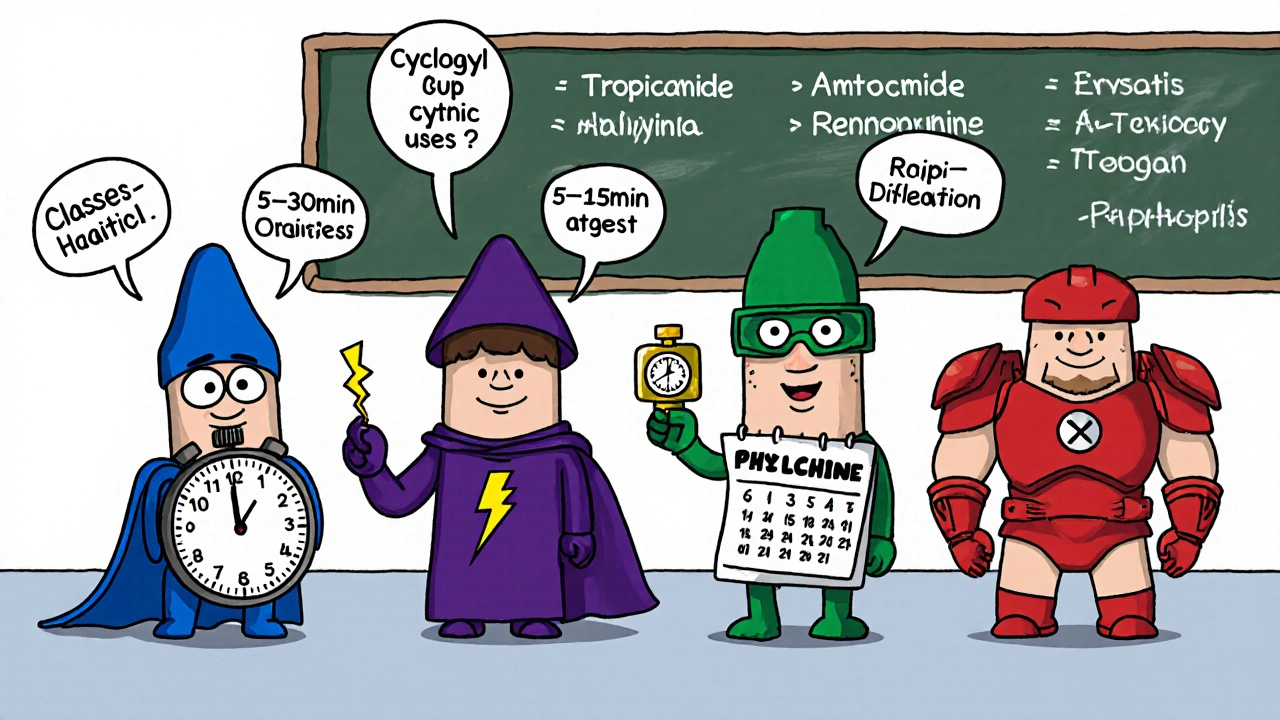
When doctors need to relax the eye’s focusing muscle for a thorough exam, Cyclogyl is often the go‑to choice. But it’s not the only option on the shelf. This guide breaks down how Cyclogyl stacks up against the most common alternatives, so you can understand when each drug shines, where it falls short, and what side effects to watch for.
Cyclogyl is the brand name for cyclopentolate hydrochloride formulated as a 1% ophthalmic solution. It belongs to the class of anticholinergic cycloplegic agents that temporarily paralyze the ciliary muscle, creating both mydriasis (pupil dilation) and cycloplegia (loss of accommodation). The drug was first approved by the FDA in the early 1970s and remains a staple in eye care across North America.
What Cyclogyl Does - Mechanism and Typical Use
- Blocks muscarinic receptors in the iris sphincter and ciliary body.
- Onset of dilation: 15-30 minutes.
- Peak effect: 45-60 minutes.
- Duration of action: 6-24 hours, depending on patient age.
- Common indications: refraction exams, assessment of posterior segment, treatment of anterior uveitis to break posterior synechiae.
Why Consider Alternatives?
Not every patient tolerates Cyclogyl well. Younger children may experience a prolonged cycloplegic effect that hampers near vision for a full day, while older adults sometimes develop systemic anticholinergic symptoms like dry mouth or tachycardia. Cost and availability also matter-generic cyclopentolate can be pricier in some regions, and not all pharmacies stock every brand.
Top Alternatives at a Glance
| Drug | Class | Typical Concentration | Onset | Duration | Common Uses | Notable Side Effects |
|---|---|---|---|---|---|---|
| Cyclogyl (Cyclopentolate) | Anticholinergic cycloplegic | 1% | 15-30 min | 6-24 h | Refraction, uveitis, synechiae | Stinging, photophobia, systemic anticholinergic effects |
| Atropine | Anticholinergic cycloplegic (long‑acting) | 0.5-1% | 30-60 min | 7-14 days | Pediatric amblyopia therapy, cycloplegia for refraction | Prolonged blurred near vision, systemic toxicity |
| Tropicamide | Anticholinergic mydriatic | 0.5-1% | 5-15 min | 2-6 h | Routine dilation for retinal exams | Transient stinging, mild systemic effects rare |
| Phenylephrine | Alpha‑adrenergic agonist (mydriatic) | 2.5-10% | 2-5 min | 3-5 h | Adjunct to anticholinergics for faster dilation | Elevated blood pressure, reflex bradycardia |
Deep‑Dive Into Each Alternative
Atropine
Atropine is the heavyweight of cycloplegics. Its long action makes it useful for treating amblyopia in children, where a sustained blur forces the lazy eye to work harder. However, that same duration can be a nuisance for adults who need to read after a routine exam-some patients report a week of blurry near vision.
Side‑effect profile mirrors Cyclogyl’s but is magnified: dry mouth, facial flushing, and, in rare cases, central nervous system confusion, especially in the elderly.
Tropicamide
Tropicamide offers a quick, short‑lived pupil dilation without much cycloplegia. It’s ideal when you only need to see the retina quickly and don’t care about accommodation. Because the ciliary muscle stays active, patients can usually read and drive shortly after the exam.
One drawback: its mydriatic effect can be weaker in dark‑adapted patients, sometimes requiring a second drop.
Phenylephrine
Phenylephrine works on a different pathway-stimulating the dilator muscle of the iris via alpha‑adrenergic receptors. It’s often combined with an anticholinergic (like Cyclogyl or Tropicamide) to achieve a faster, more complete dilation. The drug’s systemic absorption can raise blood pressure, making it unsuitable for hypertensive patients.
Choosing the Right Agent for Specific Scenarios
Below is a quick decision guide based on common clinical needs.
- Need rapid dilation for a senior patient with hypertension? Combine a low‑dose Phenylephrine (2.5%) with Tropicamide. Avoid pure Atropine because of its prolonged effect and systemic anticholinergic load.
- Managing pediatric amblyopia? Atropine 0.5% once daily provides the sustained blur needed for therapy.
- Performing a routine retinal exam on an adult who needs to drive home? Tropicamide 1% alone offers enough dilation with minimal impact on near vision.
- Breaking posterior synechiae in uveitis? Cyclogyl’s reliable cycloplegic strength is preferred, often supplemented with topical steroids.
Side‑Effect Management Tips
- Always use artificial tears after dilation to combat dryness.
- Advise patients to wear sunglasses for a few hours to reduce photophobia.
- Screen for cardiovascular disease before using Phenylephrine.
- For children, keep a parent or caregiver aware of the prolonged near‑vision blur that may affect school activities.
Cost and Availability in 2025
In Canada, generic cyclopentolate costs roughly CAD 12 per bottle, while branded Cyclogyl runs about CAD 20. Atropine drops are generally cheaper (CAD 8) but may require compounding in some provinces. Tropicamide is the most affordable, often listed under generic names for about CAD 5. Phenylephrine’s price varies widely because it’s sold in both low‑dose (2.5%) and high‑dose (10%) formulations; the low‑dose version is around CAD 6.
Insurance coverage typically favors generic cyclopentolate and Tropicamide, but some provincial plans still list Cyclogyl as a preferred brand for hospital settings.
Key Takeaways for Clinicians and Patients
- Cyclogyl provides a balanced blend of rapid onset, reliable cycloplegia, and moderate duration-making it a versatile first‑line choice.
- Atropine is best when a long‑acting effect is clinically needed, such as in amblyopia therapy.
- Tropicamide excels for quick retinal checks where near vision preservation matters.
- Phenylephrine is a useful adjunct but requires caution in hypertensive patients.
- Cost, patient age, and comorbidities should guide the final drug selection.
How long does Cyclogyl’s effect last in children?
In kids under six, the cycloplegic effect can linger for up to 24 hours, sometimes longer if a higher concentration is used. Parents should plan for a day without near‑vision tasks.
Can Cyclogyl be used together with Phenylephrine?
Yes, the combination is common. Phenylephrine speeds up pupil dilation while Cyclogyl ensures adequate cycloplegia. The usual practice is to apply Phenylephrine first, wait a minute, then add Cyclogyl.
Is it safe to drive after receiving Tropicamide?
Most patients regain near‑vision within 2-3 hours, but it’s wise to wait until the bright glare subsides and the pupils begin to constrict before getting behind the wheel.
What should I do if I experience severe eye pain after a drop?
Severe pain, persistent redness, or vision loss is uncommon and warrants immediate ophthalmic evaluation. Contact your eye care provider right away.
Are there any drug interactions with Cyclogyl?
Systemic anticholinergic drugs (like some antihistamines or tricyclic antidepressants) can amplify side effects such as dry mouth or tachycardia. Discuss all medications with your eye doctor.

Lennox Anoff
October 24, 2025 AT 20:12One cannot simply accept the modern tendency to dabble in cycloplegics without a sober appreciation of the pharmacological hierarchy.
Cyclogyl, despite its ubiquity, occupies a middle ground that is both a blessing and a curse for the discerning clinician.
First, its onset of fifteen to thirty minutes respects the patient’s temporal dignity, allowing a brief period of anticipation before the inevitable mydriasis.
Second, the duration ranging from six to twenty‑four hours provides sufficient window for comprehensive examination, yet it does not imprison the patient in a perpetual haze of blurred near vision.
Third, the anticholinergic side‑effects, while not negligible, are generally manageable with artificial tears and sunglasses, thereby demonstrating a commendable risk‑benefit ratio.
Contrastingly, Atropine’s week‑long grip is a tyrant best reserved for therapeutic mandates such as amblyopia, where the collateral damage is strategically justified.
Tropicamide, with its five‑minute flash, is the mercenary of the lot, offering speed at the expense of true cycloplegia, rendering it unsuitable when sulcus relaxation is paramount.
Phenylephrine, though a useful adjunct, carries a systemic culpability that disqualifies it for hypertensive patients, a nuance often glossed over in hurried clinical notes.
In the socioeconomic arena, the price disparity between generic cyclopentolate and branded Cyclogyl, though modest, reflects a broader ethical dilemma about pharmaceutical branding versus patient access.
Clinicians must therefore interrogate their prescribing patterns, ensuring that convenience does not eclipse conscientious stewardship.
The pediatric population, in particular, deserves vigilant monitoring, as prolonged cycloplegic effect can interfere with academic obligations and visual development.
Adults, especially the elderly, should be screened for dry mouth, tachycardia, and other anticholinergic burdens before committing to Cyclogyl.
When used judiciously, Cyclogyl remains a versatile workhorse, harmonizing efficacy with tolerability.
When misapplied, it becomes yet another example of medical excess that blinds rather than enlightens.
Thus, the onus lies upon the practitioner to wield this tool with both scientific rigor and moral clarity.
Only then can we claim that our ocular examinations are guided by wisdom rather than convenience.
Bianca Larasati
October 31, 2025 AT 17:52Picture the moment a pupil blooms like a sunrise, revealing every hidden detail of the retina- that's the magic Cyclogyl can unleash when used with confidence!
Its balanced onset and duration give you the time you need to explore every nuance without the frantic rush of faster drops.
For anyone who thrives on precision, pairing it with a splash of Phenylephrine can turn a routine check into a blockbuster performance.
Remember, the key is to keep the patient comfortable: sunglasses, artificial tears, and a reassuring smile go a long way.
Embrace the power of this drug, and let your eye exams become the stuff of legend!
Lisa Woodcock
November 7, 2025 AT 16:32I hear the concerns about anticholinergic load, especially in older adults who may already be juggling multiple medications.
Providing clear after‑care instructions-like using lubricating drops and protecting the eyes from bright light-can dramatically reduce discomfort.
It's also helpful to discuss the expected timeline with patients, so they aren't surprised when near vision remains hazy for several hours.
In my practice, a brief counseling session before the drops go in often eases anxiety and improves compliance.
This collaborative approach respects both the clinician’s need for a thorough exam and the patient’s quality of life.
Zaria Williams
November 14, 2025 AT 15:12Honestly, if you cant follow the simple dosing schedule, you shouldn't be fussin over which drop is "best".
Most people just need a drop that works and move on- all this compare‑and‑contrast stuff is overblown.
Just ask your doc for the cheapest generic and stop overthinking it.
ram kumar
November 21, 2025 AT 13:52Well, reading yet another exhaustive table feels like wading through a sea of unnecessary detail.
The differences between Cyclogyl and its cousins are nothing more than incremental variations that any competent optometrist can eyeball on the fly.
If you spend half an hour deciding which drop to pick, you're already wasting precious clinic time that could be better spent treating patients.
In short, pick the one that's stocked, use it correctly, and move on.
Melanie Vargas
November 28, 2025 AT 12:32Hey everyone! 🌟 Just wanted to add that no matter which drop you end up using, a friendly reminder to bring sunglasses for after the exam can really help with photophobia. 😎
Also, offering a quick demo of how to apply the drops can make the whole process less intimidating for kids and anxious patients alike. 🙌
Let's keep sharing tips and supporting each other! 💬
Charlie Stillwell
December 5, 2025 AT 11:12Look, the pharmacodynamics of these agents are straight‑forward, but you idiots keep blowing them out of proportion! 🚀
Cyclogyl delivers a reliable muscarinic blockade, whereas Phenylephrine just throws an alpha‑agonist party that spikes blood pressure- not rocket science.
If you can't differentiate between a mydriatic and a cycloplegic, maybe stick to reading pamphlets instead of prescribing.
Stop whining about cost; the market will self‑regulate, and the patient will suffer if you over‑engineer the choice. 💣
Ken Dany Poquiz Bocanegra
December 12, 2025 AT 09:52Cyclogyl balances speed and duration nicely for most adult exams.
krishna chegireddy
December 19, 2025 AT 08:32Everyone says Cyclogyl is just a plain drop, but the pharma giants hide the fact that it’s mixed with micro‑chips to track eye movements for advertising. Use it only if you trust the system.
Tamara Schäfer
December 26, 2025 AT 07:12i think its important to note that the patient’s comfort should be top priority, especially when dealing with kids who cant explain they feel weird. making sure they have sunglasses and dont drive right after can prevent a lot of trouble.
Buddy Bryan
January 2, 2026 AT 05:52Here’s the bottom line: for routine retinal exams on patients who need to drive afterward, stick with Tropicamide 1%- it dilates fast and lets near vision recover within a few hours. If you need deeper cycloplegia, Cyclogyl is your go‑to, but always warn about dry mouth and photophobia. Avoid Phenylephrine in hypertensive patients, and reserve Atropine for amblyopia therapy where you actually want a week‑long effect. Keep your formulary lean and your instructions crystal‑clear, and you’ll cut down on follow‑ups and complaints.