Gout Risk Calculator
Assess Your Gout Risk
This tool estimates your risk of gout flare-up when taking thiazide diuretics based on your medical profile and uric acid levels.
Your Gout Risk Assessment
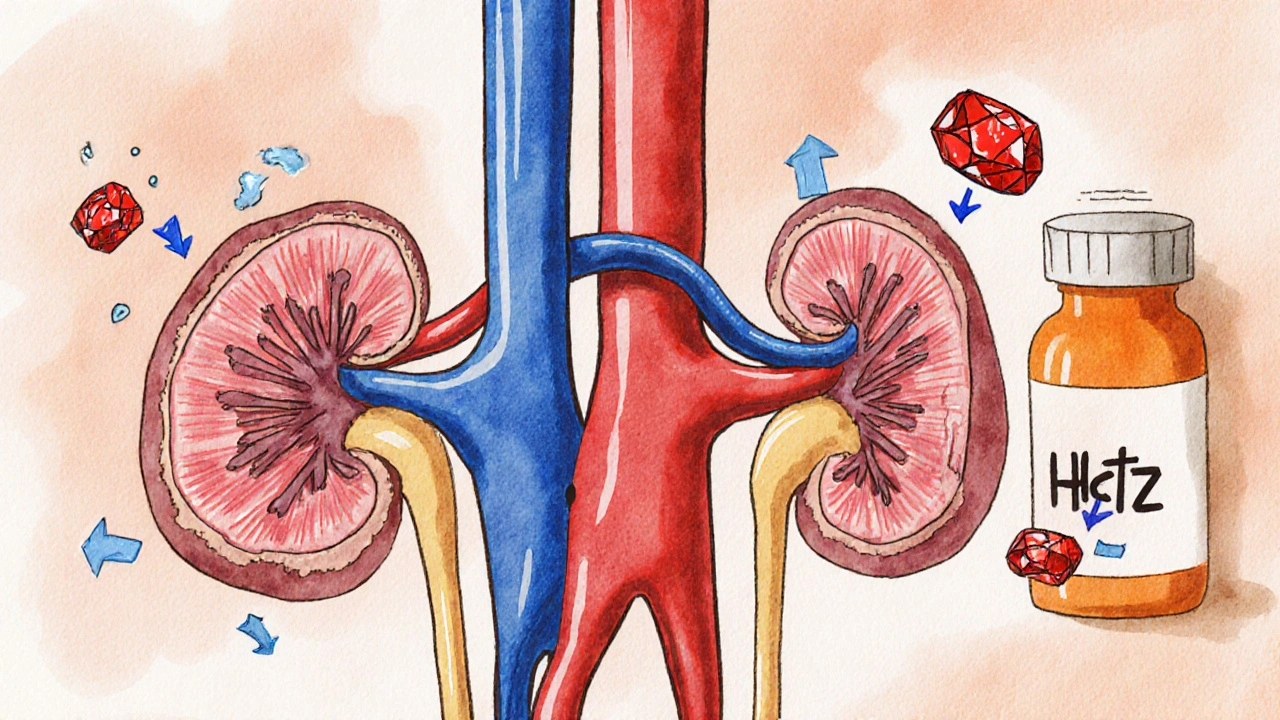
Many people take thiazide diuretics like hydrochlorothiazide (HCTZ) to control high blood pressure. It’s one of the most common pills prescribed in the U.S.-over 35 million prescriptions in 2022 alone. But if you’ve ever had gout, or if your uric acid levels are already high, this medication might be doing more harm than good. The problem isn’t just a side effect-it’s a direct, well-documented trigger for flare-ups.
How Thiazide Diuretics Raise Uric Acid
Thiazide diuretics work by making your kidneys flush out more sodium and water. That lowers blood pressure. But here’s the catch: they also interfere with how your body gets rid of uric acid. Uric acid is a natural waste product from breaking down purines in food. Normally, your kidneys filter it out and send it through urine. But thiazides block the same transporters in the kidney tubules that move uric acid out.
Specifically, they compete with uric acid at the OAT1 and OAT4 transporters on kidney cells. When thiazides slip in, they push uric acid back into the bloodstream instead of letting it leave. Studies show this effect starts within 3 to 7 days of starting the drug. And it doesn’t go away-you keep accumulating uric acid as long as you’re on it.
The numbers don’t lie. Clinical trials show thiazide use can raise serum uric acid by 6% to 21% compared to baseline. For someone with already borderline levels, that’s enough to cross the saturation point: 6.8 mg/dL. Once you hit that, uric acid crystals form in joints. That’s gout.
The Real Risk: How Often Does Gout Actually Happen?
Not everyone on thiazides gets gout. About 12% to 15% develop high uric acid levels, but only 1% to 2% end up with painful gout attacks. So why does this matter so much? Because for some people, it’s not just a number-it’s life-changing pain.
Research tracking over 247,000 hypertensive adults found that after 180 days of taking thiazides, the risk of needing gout medication jumped by 41%. That’s not a small bump. And the longer you take it, the worse it gets. After one year, the chance of needing allopurinol or colchicine was nearly 19%, compared to 14% for people on other blood pressure pills.
What’s worse? Many doctors don’t catch it until it’s too late. Patients come in with a swollen, red big toe-classic gout-and the doctor sees high blood pressure. They don’t connect the dots. But the link is strong enough that major guidelines now say: if you’ve had gout before, avoid thiazides unless you’re already on urate-lowering therapy.
Who’s Most at Risk?
It’s not just about the drug. Genetics, diet, and kidney health all play a role. But here’s who should be extra careful:
- Men with uric acid levels above 7.0 mg/dL
- Women with levels above 6.0 mg/dL
- Anyone who’s had even one gout attack in the past
- People with chronic kidney disease
- Those who drink alcohol regularly or eat a lot of red meat, shellfish, or sugary drinks
Here’s the tricky part: high blood pressure itself increases your risk of gout. So does being overweight. That makes it hard to tell if the gout came from the diuretic or the condition it’s treating. But studies show thiazides add independent risk-on top of everything else.
Chlorthalidone vs. Hydrochlorothiazide: Is One Worse?
For years, people thought chlorthalidone was riskier than hydrochlorothiazide because it’s stronger and lasts longer. But a 2019 study comparing them directly found no difference in gout risk when doses were matched. Both raise uric acid the same way. So if you’re switching from one to the other thinking it’s safer, you’re not getting any benefit.
That’s important because chlorthalidone is often used in combination pills. If you’re on a combo with a calcium channel blocker or ACE inhibitor, you might not even realize you’re on a thiazide. Always check the active ingredients.
What About Other Diuretics?
Loop diuretics like furosemide (Lasix) are even more likely to cause gout than thiazides. They’re stronger at blocking uric acid excretion. So if you’re on a loop diuretic for heart failure or edema, gout risk is even higher.
But there’s good news: not all diuretics do this. Potassium-sparing diuretics like spironolactone and eplerenone don’t interfere with uric acid transporters. In fact, spironolactone may slightly lower uric acid levels. If you have both hypertension and gout, switching to spironolactone could be a smart move-especially if you’re also on an ACE inhibitor or ARB.

Alternatives That Don’t Raise Uric Acid
If you’re on a thiazide and have gout or high uric acid, you don’t have to give up on blood pressure control. There are better options:
- Losartan (Cozaar): This is an ARB, but it’s special. It actually helps your kidneys dump more uric acid by blocking the URAT1 transporter. It’s one of the few blood pressure drugs that may help both conditions at once.
- Calcium channel blockers like amlodipine: These have no effect on uric acid. They’re just as effective for lowering blood pressure as thiazides.
- ACE inhibitors like lisinopril: They have a neutral or slightly beneficial effect on uric acid.
Cost is a concern. Generic hydrochlorothiazide costs about $4 for 90 pills. Losartan and amlodipine are a bit pricier-$10 to $15-but still affordable. And if you’re avoiding gout attacks, that extra cost could save you thousands in ER visits and missed work.
What Should You Do?
If you’re taking a thiazide diuretic and have gout, here’s your action plan:
- Check your uric acid level. If it’s above 6.8 mg/dL, you’re at risk.
- Review your meds with your doctor. Ask: “Is this the best choice for me given my gout history?”
- If you must stay on a diuretic, ask about switching to spironolactone.
- If you’re on losartan, you’re already ahead of the game.
- Watch your diet: limit beer, shellfish, organ meats, and sugary sodas. Drink more water.
- If you’ve had multiple gout attacks, ask about allopurinol. Start low-100 mg daily-and monitor uric acid levels every 2 to 3 months.
Don’t stop your medication cold turkey. Blood pressure can rebound dangerously. Work with your doctor to switch safely.
The Bottom Line
Thiazide diuretics are cheap, effective, and widely used. But they’re not harmless. For people with gout or high uric acid, they’re a ticking time bomb. The science is clear: these drugs raise uric acid, and that raises your risk of painful, disabling attacks.
The good news? You have choices. You don’t have to live with high blood pressure and gout. There are alternatives that control pressure without triggering pain. The key is awareness-and talking to your doctor before it’s too late.
If you’ve had even one gout flare after starting HCTZ or chlorthalidone, that’s not a coincidence. That’s your body telling you something. Listen to it.
Can thiazide diuretics cause gout even if I’ve never had it before?
Yes. While not everyone develops gout, thiazide diuretics can trigger the first attack in people with no prior history. About 1% to 2% of users develop symptomatic gout within the first year, and risk increases with longer use. People with high uric acid, obesity, or a family history of gout are most vulnerable.
How long does it take for uric acid to drop after stopping thiazides?
Uric acid levels usually return to baseline within 2 to 3 months after stopping thiazide diuretics. Some people see improvement in as little as 4 weeks, especially if they also reduce alcohol and purine-rich foods. But if crystals have already formed in joints, symptoms may linger until the body clears them out.
Is chlorthalidone worse than hydrochlorothiazide for gout?
No. Studies comparing the two show they raise uric acid to the same degree when given in equivalent doses. The belief that chlorthalidone is riskier was based on older assumptions. Both drugs work the same way in the kidneys and carry the same gout risk.
Should I avoid all diuretics if I have gout?
Not all. Loop diuretics like furosemide increase gout risk even more. But potassium-sparing diuretics like spironolactone and eplerenone do not raise uric acid and may even help lower it. They’re safe alternatives for people with both hypertension and gout.
Can I take allopurinol with thiazide diuretics?
Yes, but it’s not ideal. Allopurinol can prevent gout attacks while you’re on a thiazide, but it doesn’t fix the root problem-the drug is still raising your uric acid. The better approach is to switch to a different blood pressure medication that doesn’t interfere with uric acid clearance, like losartan or a calcium channel blocker.
Does drinking more water help reduce uric acid from thiazides?
Yes, but it’s not enough on its own. Staying well-hydrated helps your kidneys flush out more uric acid, which can lower your risk of crystal formation. But if you’re on a thiazide, the drug is still blocking the key transporters. Water helps, but switching medications is the only way to truly eliminate the risk.
Bharat Alasandi
November 19, 2025 AT 08:34Bro, I was on HCTZ for 3 years and didn’t realize my toe pain was gout until I collapsed at a BBQ. Turned out my uric acid was at 8.2. Doc said it was the diuretic. Switched to amlodipine and boom-no more flare-ups. Life’s better now. Don’t ignore the signs.
Kristi Bennardo
November 19, 2025 AT 18:31This is an outrage. The pharmaceutical industry has been quietly poisoning millions of hypertensive patients with thiazides for decades while pushing them toward expensive, unnecessary gout treatments. Who benefits? Not you. Not me. The stockholders. Wake up.
Shiv Karan Singh
November 20, 2025 AT 04:12LMAO so now we’re blaming the drug and not the guy who eats 10 shrimp tacos every weekend? 😂 You think HCTZ is the villain? Try cutting out the beer and red meat first. Then come back.
Ravi boy
November 21, 2025 AT 22:37bro i had gout after starting hctz and i thought it was just a bad toe injury till my cousin who is a nurse said its prob the med. switched to losartan and my uric acid dropped like a rock. no more pain. also drink more water lol
Matthew Karrs
November 23, 2025 AT 09:28They say it’s 1-2% risk. But what if you’re in that 1-2%? And what if your doctor never checks your uric acid? What if you’re just told to take more colchicine? This isn’t medicine-it’s gambling with your joints. And they wonder why people distrust the system.
Matthew Peters
November 24, 2025 AT 09:13Whoa. I didn’t realize chlorthalidone and HCTZ were basically the same in terms of gout risk. That’s wild. I thought chlorthalidone was the ‘stronger’ one so it’d be worse. Turns out they’re both just sneaky little uric acid blockers. Mind blown. Also-spironolactone as an alternative? That’s actually genius. Why isn’t this talked about more?
Liam Strachan
November 26, 2025 AT 08:19Interesting read. I’ve got hypertension and a bit of high uric acid, but no gout yet. I’ve been thinking about switching meds anyway-this just gave me the push. Thanks for laying it out so clearly. I’ll bring this to my doc next week. Maybe losartan’s the way to go?
Gerald Cheruiyot
November 26, 2025 AT 08:52There’s a deeper truth here. We treat symptoms like they’re separate problems-high BP here, gout there. But the body doesn’t work that way. It’s all connected. A diuretic that helps one system breaks another. Maybe we need to stop seeing pills as magic bullets and start seeing them as tools that shift the whole ecosystem. We’re not just treating disease-we’re playing with physiology.
Michael Fessler
November 27, 2025 AT 15:26Just want to add-allopurinol + thiazide isn’t a no-go, but it’s a bandaid. The real fix is switching meds. Also, if you’re on a combo pill like Amturnide or Tekturna HCT, you might not even know you’re getting HCTZ. Always check the label. I’ve seen so many patients miss this. And hydrate. Even if you’re on meds, water helps flush the crystals. Not a cure, but it helps.
daniel lopez
November 28, 2025 AT 23:30Of course the FDA and Big Pharma don’t warn you. They’re too busy making billions off gout meds and combo pills. They want you on thiazides forever so you keep buying allopurinol and colchicine. They don’t care if you’re in pain. They care about your prescription refill rate. Read the studies-this isn’t a side effect. It’s a feature.