Vitamin D Level Checker for Statin Tolerance
For millions of people taking statins to lower cholesterol and prevent heart attacks, muscle pain isn’t just an annoyance-it’s a dealbreaker. About 1 in 5 patients stop taking statins because of muscle aches, weakness, or cramps. And for years, many doctors have looked to vitamin D as a possible fix. Could fixing a vitamin D deficiency help people stick with their statins? The answer isn’t simple, and the science has taken a sharp turn in recent years.
Why Vitamin D Got So Much Attention
Around 2009, a small but eye-opening study caught the attention of cardiologists. Researchers found that 92% of patients who had quit statins due to muscle pain started tolerating them again after their vitamin D levels were corrected. That’s not a small number. It suggested a powerful, easy-to-fix link: low vitamin D = muscle problems = statin intolerance. Follow-up studies echoed this. One 2017 study showed that patients with vitamin D levels below 20 ng/mL had a 90% success rate restarting statins after supplementation. Those with higher levels? Only 33% could tolerate them again. It made sense biologically, too. Vitamin D helps regulate calcium and muscle function. Deficiency is known to cause muscle weakness. Statins, meanwhile, can interfere with muscle cell energy production. So if your muscles are already struggling from low vitamin D, adding a statin might push them over the edge. Doctors started checking vitamin D levels routinely in patients with statin-related muscle complaints. Many began supplementing with 1,000-2,000 IU daily before trying statins again. For some, it worked. Patients reported feeling stronger, pain faded, and they stayed on their meds.The Big Study That Changed Everything
But science doesn’t rely on anecdotes or small observational studies. It needs randomized trials-where patients are randomly assigned to get the real treatment or a dummy pill, and neither the patient nor the doctor knows which is which. That’s the gold standard. In 2022, the JAMA Cardiology study dropped a bombshell. It looked at over 2,000 people starting statins as part of the massive VITAL trial. Half got 2,000 IU of vitamin D daily. The other half got a placebo. After a year, the results were clear: no difference. Both groups had the same rate of muscle pain (31%) and the same rate of stopping statins (13%). This wasn’t a fluke. It was a large, well-designed, rigorously controlled study. It didn’t find a benefit. And that’s the problem: now we have two conflicting stories. One says vitamin D fixes statin muscle pain. The other says it doesn’t.Why the Conflict? The Hidden Flaws in the “Helpful” Studies
The early studies that showed vitamin D helping were mostly observational. They looked at patients who already had low vitamin D and muscle pain, gave them supplements, and saw improvement. But here’s the catch: those patients weren’t randomly assigned. They were self-selected. Maybe they were more health-conscious. Maybe they changed their diet, exercised more, or got more sun after their diagnosis. Maybe their pain improved simply because they were paying more attention to their body. Also, muscle pain from statins is subjective. There’s no blood test that confirms it. Patients say, “My legs hurt,” and that’s it. That makes it easy for placebo effects to show up. If you believe vitamin D will help, you might feel better-even if it’s not doing anything physiologically. The 2017 study that showed 90% success? It didn’t have a placebo group. Patients knew they were getting vitamin D. That’s a huge red flag. The 2022 trial did. And it found nothing.
What About Statin Types? Does Vitamin D Help More With Some?
Some studies suggest certain statins are easier to tolerate after vitamin D correction. The 2017 study found that after supplementation, pravastatin and rosuvastatin were best tolerated. Atorvastatin, the most commonly prescribed statin, was less likely to work-even after vitamin D was fixed. One 2019 study even found that patients on atorvastatin had higher vitamin D levels to begin with, raising the question: do statins affect vitamin D, not the other way around? That’s a twist. Maybe statins are boosting vitamin D levels slightly, not the other way around. If true, then low vitamin D might just be a marker of something else-like poor overall health, less sun exposure, or even more severe statin side effects-not the cause.Who Might Still Benefit?
Even with the 2022 trial results, some experts still believe vitamin D matters-for the right people. The 2017 study showed that only those with severe deficiency (≤20 ng/mL) had dramatic improvements. Those with levels above 20 didn’t benefit much. That’s a key detail. If you’re taking a statin and you’re truly deficient-say, your level is 12 ng/mL-correcting that might help your muscles recover. It won’t necessarily fix statin pain, but it might remove one layer of muscle stress. And if you’re already deficient, you should be supplementing anyway. Vitamin D deficiency is linked to bone loss, fatigue, and immune issues. Fixing it is good for your health, regardless of statins. But if your vitamin D level is 25 ng/mL or higher? There’s no strong reason to think extra vitamin D will let you tolerate statins better. You’re not deficient. Taking more won’t help-and might even mask other underlying issues.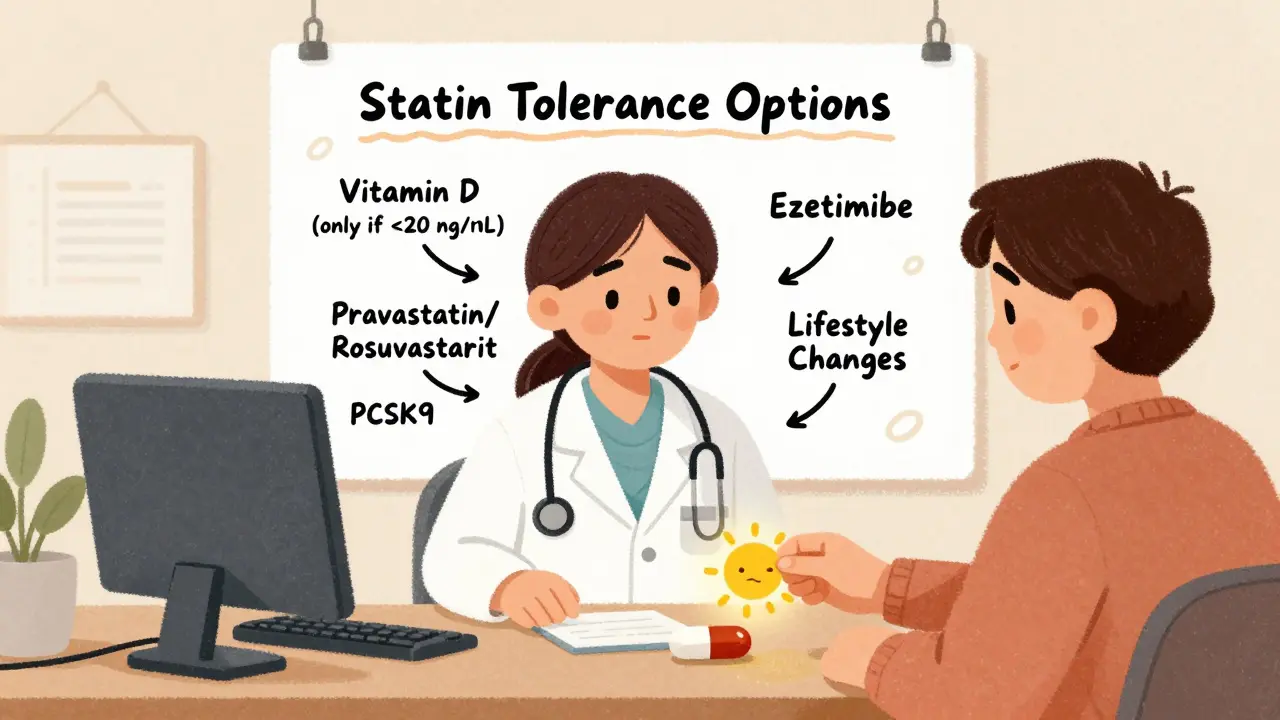
What Should You Do If You Can’t Tolerate Statins?
Don’t assume vitamin D is the answer. But don’t ignore it either. Here’s a practical approach:- Get your vitamin D level checked if you have muscle pain on statins. If it’s below 20 ng/mL, supplement with 1,000-2,000 IU daily until it’s above 30 ng/mL.
- If you’re deficient and your pain improves after 2-3 months, you *might* be able to restart a statin. Start with a low dose of pravastatin or rosuvastatin-these seem better tolerated in this group.
- If your vitamin D is normal (≥25 ng/mL), don’t waste time on extra supplements. Focus on other options: try a different statin, lower the dose, take it every other day, or consider non-statin alternatives like ezetimibe or PCSK9 inhibitors.
- Keep a symptom diary. Note when pain starts, how bad it is, and whether it’s linked to activity or rest. This helps your doctor tell if it’s truly statin-related or something else-like arthritis or nerve issues.
The Bigger Picture: Why This Matters
Statin intolerance isn’t just about muscle pain. It’s about heart attacks. People who stop statins because of side effects have a 20-30% higher risk of heart events over the next five years. That’s huge. Finding ways to keep people on these drugs saves lives. Vitamin D seemed like a cheap, safe, easy win. But science doesn’t always give us easy answers. The truth is, we still don’t fully understand why some people get muscle pain on statins and others don’t. Genetics, age, kidney function, thyroid issues, and even exercise habits all play a role. Vitamin D might help a small subset of people with severe deficiency. But for most, it’s not the magic fix. The best path forward? Test if you’re deficient. Correct it if needed. But don’t stop there. Work with your doctor to explore other options. There are more ways to manage cholesterol than just one pill.What’s Next?
Researchers are still asking questions. Is there a genetic subgroup that responds to vitamin D? Do certain statins interact differently with vitamin D metabolism? Could combining vitamin D with other supplements like coenzyme Q10 help? For now, the evidence says this: if you’re severely deficient, fix it. It’s good for your bones, your muscles, and your overall health. But if you’re not deficient, don’t count on vitamin D to save your statin therapy. The answer lies elsewhere-and that’s where science is headed next.Can vitamin D deficiency cause muscle pain even without statins?
Yes. Vitamin D deficiency is directly linked to muscle weakness, fatigue, and diffuse muscle aches. People with very low levels (below 20 ng/mL) often report trouble climbing stairs, rising from a chair, or walking long distances. This is separate from statin-related pain but can make it harder to tell the difference. That’s why checking vitamin D levels is still important-even if you’re not on statins.
Should everyone on statins take vitamin D supplements?
No. Only take vitamin D if your blood test shows a deficiency (below 30 ng/mL). Taking extra vitamin D when you’re not deficient doesn’t improve statin tolerance and can lead to side effects like high calcium levels or kidney stones over time. Don’t self-prescribe. Get tested first.
What’s the best statin to try after vitamin D correction?
Based on clinical studies, pravastatin and rosuvastatin are most often tolerated after vitamin D repletion. Pravastatin is less likely to be metabolized by liver enzymes that may be affected by low vitamin D, and rosuvastatin has a lower risk of muscle-related side effects overall. Avoid high-dose simvastatin or atorvastatin initially-these are more likely to cause problems.
How long should I wait after starting vitamin D before trying a statin again?
Wait at least 8-12 weeks. Vitamin D levels take time to rise, and muscle tissue needs time to recover. Check your level again after 3 months. If it’s above 30 ng/mL and your muscle pain has improved, you can discuss restarting a statin with your doctor-starting with a low dose and monitoring closely.
If vitamin D doesn’t help, what are my alternatives to statins?
There are several non-statin options: ezetimibe (lowers cholesterol absorption), PCSK9 inhibitors (injections that dramatically lower LDL), bempedoic acid (oral pill with lower muscle risk), and bile acid sequestrants. Lifestyle changes-like a Mediterranean diet, regular exercise, and weight loss-are also proven to reduce cardiovascular risk. Your doctor can help you pick the best mix based on your risk level and preferences.

Jody Fahrenkrug
January 17, 2026 AT 02:52Been on statins for 6 years and my doc checked my vit D last year-was at 18. Took 2k IU daily for 3 months, muscle cramps vanished. Not saying it works for everyone, but for me? Total game changer. I don’t care what the big study says, my legs feel better.
Samyak Shertok
January 17, 2026 AT 17:09Oh wow, so now we’re blaming vitamin D deficiency for everything? Next they’ll say your WiFi router caused your statin side effects. 🤡 Science isn’t a buffet where you pick the trendiest nutrient to fix your problems. The RCT says no effect. End of story. The rest is placebo theater.
Stephen Tulloch
January 19, 2026 AT 04:06Bro, I’m on rosuvastatin and my vit D was 22. Took the supplement like a good little sheep. Pain didn’t go away. Then I switched to ezetimibe and my life improved. Stop romanticizing supplements. The real fix is knowing your body and listening to your doctor-not some 2017 anecdote with no placebo group. 🧪
Joie Cregin
January 19, 2026 AT 06:16I love how this post breaks it all down without shaming people who feel awful on statins. My mom had this nightmare for years-thought she was just getting old until they found her vit D was 11. After 4 months of supplements, she could finally walk to the mailbox without wincing. It’s not magic, but it’s not nothing either. Sometimes the fix is just removing one layer of stress from your body. 💛
Rob Deneke
January 19, 2026 AT 19:07Check your levels first dont just pop pills like candy if your vit D is fine no point if its low yeah try it but dont blame the vitamin if it doesnt work also try a different statin pravastatin is gentler
Chelsea Harton
January 21, 2026 AT 18:19vit d helps some. not all. big study says no. but my cousin felt better. so maybe it’s the placebo. or maybe it’s real. who knows. science is messy.
waneta rozwan
January 21, 2026 AT 20:58People still believe this? After the JAMA study? You’re literally clinging to a 2017 fantasy because you don’t want to admit your pain is just… part of aging or your lifestyle. Vitamin D isn’t a magic bullet. It’s a bandaid on a bullet wound. Get real.
Kasey Summerer
January 22, 2026 AT 21:05So we’re saying vitamin D fixes statin pain… unless you’re in a double-blind trial. Classic. Sounds like the same logic people use for homeopathy. ‘It worked for me!’ - yeah, and my lucky socks worked too 😏
Bobbi-Marie Nova
January 22, 2026 AT 22:18My aunt took vit D, switched to pravastatin, and now she’s hiking again. I know it’s not for everyone, but if it helps even one person avoid a heart attack? Worth a shot. No harm in testing your levels. Just don’t expect miracles.
Allen Davidson
January 23, 2026 AT 08:26Let’s not throw the baby out with the bathwater. The 2022 trial is solid, but it doesn’t invalidate what works for individuals. If you’re deficient, fix it. Your bones, your immune system, your mood-all benefit. And if your muscles feel better? That’s not placebo, that’s your body healing. Trust your experience, but stay open to science.
john Mccoskey
January 24, 2026 AT 23:35Let’s be brutally honest here. The entire vitamin D-statin narrative is a perfect storm of confirmation bias, anecdotal cherry-picking, and the pharmaceutical industry’s quiet complicity in letting patients believe there’s a simple fix so they don’t question the drug’s toxicity. The 2017 study? No control group. The 2022 trial? Rigorous. The fact that people still cling to this is less about science and more about our desperate need to believe that health problems have easy, cheap, non-pharmaceutical solutions. We’d rather blame a vitamin than accept that some people just can’t tolerate statins and need better alternatives. That’s the uncomfortable truth.
Ryan Hutchison
January 26, 2026 AT 03:31USA leads the world in vitamin D deficiency because people sit inside all day. But this isn’t about ‘fixing’ statins-it’s about fixing your lifestyle. Get outside. Move. Eat real food. Stop looking for a pill to solve a problem caused by not living like a human being. Vitamin D? Maybe. But the real fix is sunlight and squats.
Melodie Lesesne
January 26, 2026 AT 07:17My doc told me to check my vit D before trying statins again. I was at 19. Took the supplement, waited 3 months, tried rosuvastatin at half dose. No pain. I’m alive and my cholesterol’s under control. Doesn’t mean it’ll work for you. But for me? It was the missing piece. Thanks for the balanced post-this is the kind of info that actually helps.