Imagine trying to listen to someone whisper, but all you hear is muffled silence. Or turning up the TV so loud your family complains, yet you still can’t catch what’s being said. If this sounds familiar, and you’re in your 30s or 40s, it might not be aging-it could be otosclerosis.
What Exactly Is Otosclerosis?
Otosclerosis is a condition where abnormal bone grows in the middle ear, specifically around the stapes-one of the three tiny bones that carry sound vibrations from the eardrum to the inner ear. This bone, smaller than a grain of rice, normally moves freely like a piston. But in otosclerosis, it gets stuck. The bone hardens and fuses to the oval window, the gateway to the inner ear. When that happens, sound can’t travel properly. The result? Progressive hearing loss. It’s not a tumor. It’s not an infection. It’s a glitch in bone remodeling. Normally, bone breaks down and rebuilds in a balanced way. In otosclerosis, that balance is lost. New bone forms too quickly and doesn’t mature properly, creating spongy, porous tissue that eventually turns rigid. This process usually starts near the oval window, where the stapes connects to the cochlea.Who Gets Otosclerosis?
Otosclerosis doesn’t hit everyone evenly. About 1 in 200 people in the UK and 3 million Americans have it. It’s most common in adults between 30 and 50. Women are far more likely to be affected-about 70% of cases occur in women. And if your mom or dad had it, your risk doubles. About 60% of people with otosclerosis have a family history. Ethnicity also plays a role. People of European descent have the highest rates, followed by Asians. African populations have the lowest. This pattern suggests strong genetic roots. Researchers have found 15 different gene locations linked to otosclerosis, with the RELN gene on chromosome 7 being the most significant. It’s not a simple inherited trait, though-it’s complex, involving multiple genes and environmental triggers.How Does It Affect Hearing?
The hallmark of otosclerosis is conductive hearing loss. That means sound isn’t getting through the middle ear properly. It’s not that your inner ear or nerves are damaged-at least not at first. The problem is mechanical. The stapes can’t vibrate. So even if your cochlea works perfectly, the signal doesn’t reach it. Audiograms show a clear air-bone gap-usually between 20 and 40 decibels. That’s the difference between how well you hear sound through the air versus through bone conduction. In normal hearing, these are nearly the same. In otosclerosis, the gap widens as the bone stiffens. What do people actually notice? Trouble with low-pitched sounds. Whispers, male voices, background murmurs-all become hard to catch. High-pitched sounds like birdsong or children’s voices often remain clear longer. This is the opposite of age-related hearing loss, which starts with high frequencies. About 10-15% of people develop cochlear otosclerosis, where the abnormal bone spreads into the inner ear. That causes sensorineural hearing loss, which is harder to treat. This can lead to mixed hearing loss-both conductive and nerve-related. Progression is slow, but untreated, hearing can drop 15-20 dB over five years.What About Tinnitus?
Tinnitus-ringing, buzzing, or hissing in the ears-is incredibly common with otosclerosis. Around 80% of patients report it. For 35%, it’s bad enough to disrupt sleep or daily focus. The exact link isn’t fully understood, but it’s likely tied to the same abnormal bone activity affecting nearby nerves. Some people notice tinnitus gets worse when their hearing does. Others find it improves after surgery.
How Is It Diagnosed?
There’s no single blood test. Diagnosis relies on three things: symptoms, hearing tests, and imaging. First, an audiogram. If you have a conductive hearing loss with a clear air-bone gap and good speech understanding (above 70%), otosclerosis is suspected. Speech tests are important because if your ability to understand words is poor, something else might be going on. Next, a physical exam. An ENT will look into your ear with a microscope. The eardrum usually looks normal-no redness, no fluid. That rules out infections or Eustachian tube problems, which are common misdiagnoses. In fact, about 22% of patients wait an average of 18 months before getting the right diagnosis. Finally, a CT scan of the temporal bone. It can show the early spongy bone changes as small, dark spots (radiolucent foci) measuring 0.5 to 2.0 mm around the oval window. This isn’t always needed, but it helps when the diagnosis is unclear or if surgery is being considered.What Are the Treatment Options?
There are two main paths: hearing aids and surgery. Hearing aids are the first step for many. About 65% of people start here. They amplify sound, especially in the low-frequency range where otosclerosis hits hardest. Modern digital aids can even filter out background noise. They’re non-invasive, reversible, and effective. But they don’t fix the root problem. Hearing will likely keep getting worse over time. Surgery is the only way to restore natural hearing. The gold standard is stapedotomy. In this procedure, a tiny hole (0.6-0.8 mm) is drilled into the fixed stapes footplate. A prosthetic piston-usually made of titanium or stainless steel-is inserted and connected to the incus bone. This bypasses the stiff bone and lets sound vibrations pass through again. Success rates are high. Around 90-95% of first-time surgeries restore hearing to within 10 dB of normal. Most patients notice improvement within days. One teacher in Tampa said after her surgery, she could finally hear students whispering in the back row. There’s a catch. About 1% of patients experience sudden, permanent sensorineural hearing loss after surgery. It’s rare, but devastating. That’s why informed consent is critical. Surgeons must explain this risk clearly. Revision surgeries-those done after a failed first operation-have lower success rates, around 75%. That’s why choosing an experienced otologist matters. At Mount Sinai, surgeons need to complete 50 supervised stapedotomies before operating independently.New Developments in 2025
The field is evolving. In March 2024, the FDA approved the StapesSound™ prosthesis, coated with titanium-nitride. Early results show a 94% success rate at 12 months-higher than older models. The coating reduces scar tissue and adhesions, which are a common cause of long-term failure. Drug therapy is also advancing. Sodium fluoride, long used for osteoporosis, is now being tested for otosclerosis. A 2024 study showed it slowed hearing loss by 37% over two years compared to placebo. It’s not a cure, but for people who aren’t ready for surgery-or who have cochlear involvement-it’s a promising option. Genetic screening is on the horizon. Researchers are working on polygenic risk scores to identify people at high risk before symptoms appear. Within five years, doctors may be able to predict otosclerosis in young adults with a family history and monitor them closely.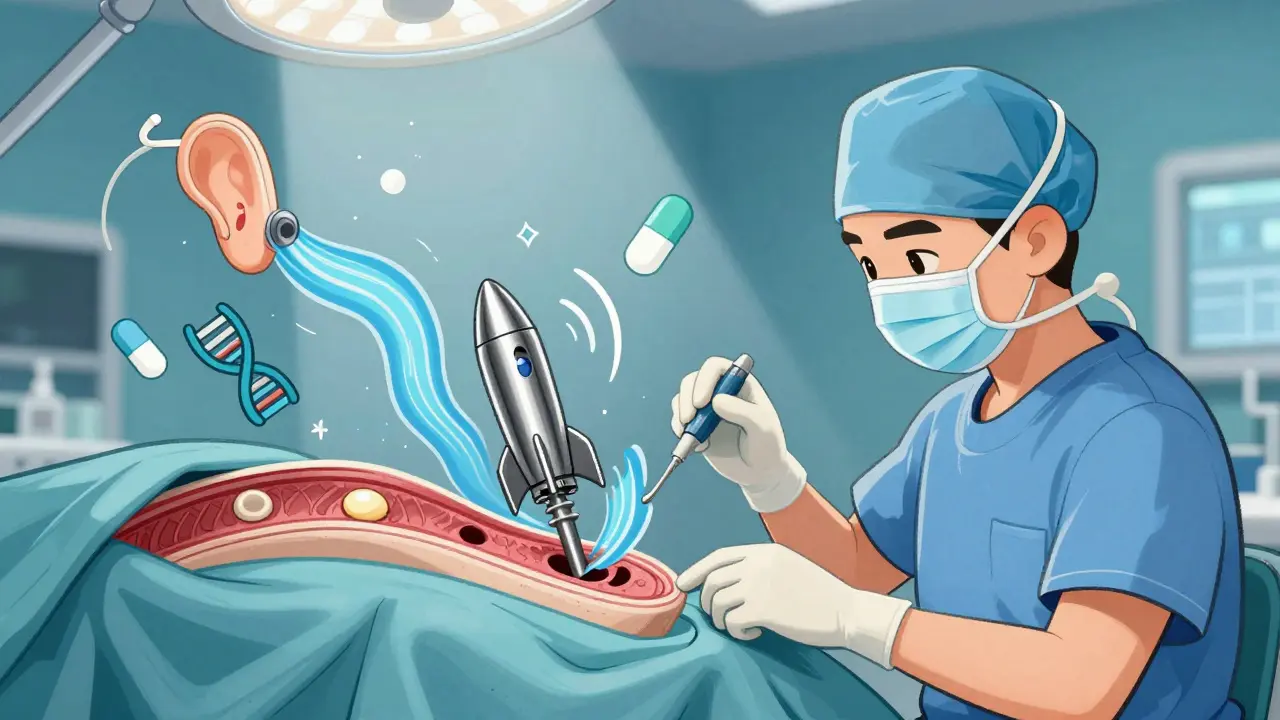

Layla Anna
January 2, 2026 AT 18:35Wow, this really hit home for me. I’ve had tinnitus for years and just thought it was stress… turns out my mom had otosclerosis too. I’m getting tested next week. Thank you for writing this with so much heart.
❤️
Alex Warden
January 3, 2026 AT 23:17Of course it’s more common in white people. The gene’s European. We built the science. The rest of the world is just catching up.
And why are we funding fluoride trials? We should be building more stapedotomies, not giving people pills.
Phoebe McKenzie
January 5, 2026 AT 10:44So let me get this straight-you’re telling me we’ve known about this for decades, but we’re still letting people suffer because surgery costs more than a new iPhone? And doctors won’t even do it unless they’ve done 50 supervised ops? That’s not medicine, that’s a bureaucratic prison.
You want to fix hearing loss? Fix the system. Not the ear.
gerard najera
January 5, 2026 AT 21:39Bone doesn’t just grow. It remembers.
Stapes isn’t stuck. It’s silenced.
Liam George
January 6, 2026 AT 12:32They say it’s genetic. But what if it’s not? What if it’s the aluminum in our water? The 5G towers near schools? The fluoride they pump into the water to make us docile? They don’t want you to know this is a manufactured epidemic-engineered to sell hearing aids and titanium pistons.
I’ve seen the documents. The FDA’s ‘StapesSound™’? Same company that made the cochlear implant recall in ’22. Coincidence? I think not.
They’re monetizing deafness. And your ‘treatment’? It’s just another product in their catalog.
Ask yourself: who profits when you can’t hear your own child cry?
Austin Mac-Anabraba
January 6, 2026 AT 16:49The article commits the fallacy of reification by treating otosclerosis as a discrete pathology rather than a phenotypic expression of dysregulated Wnt signaling pathways in the otic capsule. The RELN gene’s involvement suggests epigenetic modulation via methylation of CpG islands in the promoter region-a mechanism not discussed here, despite its centrality to the disease’s progression.
Furthermore, the assertion that ‘bone remodeling is imbalanced’ is ontologically misleading. Bone is not ‘too active’-it is misdirected. The osteoblasts are not overproducing; they are misinterpreting mechanical cues due to altered mechanotransduction in the perilymphatic microenvironment.
And yet, we prescribe hearing aids like Band-Aids on a ruptured aorta.
Olukayode Oguntulu
January 8, 2026 AT 12:17So you’re telling me the solution to hearing loss is to drill a hole in your skull and stick a metal rod in it? And this is considered ‘medicine’? In my country, we use herbal compresses and ancestral chants. At least they don’t leave you deaf on purpose.
But sure, go ahead. Trust the titanium. Trust the FDA. Trust the 50-ops rule. Meanwhile, your culture is already silent.
jaspreet sandhu
January 10, 2026 AT 12:16I’ve been hearing this for years. Everyone says surgery works. But I’ve seen three people who had it. One got worse. One got tinnitus so bad he quit his job. One just stopped answering calls. So now I just turn the TV up. If I can’t hear my wife, maybe she’s just not worth listening to anyway.
Also, why is this only talked about in the US? In India, people just live with it. No one makes a big deal. Maybe we’re the ones who got it right.
Bobby Collins
January 10, 2026 AT 15:50wait so you’re saying the government is hiding this? like… the fluoride thing? i always thought it was just for teeth but now i’m scared
also my aunt had this and she said the surgery felt like a tiny earthquake in her head
Heather Josey
January 12, 2026 AT 14:09This is such an important piece. Thank you for explaining the science without overwhelming the reader. I’ve worked with patients who’ve waited years because they thought it was just ‘getting old.’ You’ve given them language. You’ve given them hope.
If you’re reading this and wondering if it’s worth it-yes. The first time you hear your grandchild say ‘I love you’ without shouting? That’s worth every risk.
Donna Peplinskie
January 12, 2026 AT 16:06Thank you for sharing this so clearly… I’ve been helping my sister navigate this, and I didn’t even know about cochlear otosclerosis until now. I’m sharing this with her and our local support group. You’ve made something scary feel… manageable.
And to anyone reading this: you’re not alone. We’ve got you.
❤️
Lee M
January 14, 2026 AT 09:18They call it a glitch. But what if it’s evolution? Maybe the body’s trying to protect the cochlea from noise pollution. Maybe the bone hardens because the world is too loud.
We don’t fix the noise. We fix the ear.
That’s the real tragedy.
LIZETH DE PACHECO
January 15, 2026 AT 23:05I’m so glad someone finally wrote this without jargon. My brother had this and nobody listened until he screamed at his doctor. Please, if you think you might have this-go to an ENT who does stapedotomies. Don’t wait. Don’t second-guess. You deserve to hear your own voice again.
Stephen Gikuma
January 16, 2026 AT 09:36They say it’s genetic. But who’s paying for the research? Who owns the patents? The same companies that sell the hearing aids. The same ones that shut down the fluoride trials because they didn’t want competition.
This isn’t medicine. It’s corporate control disguised as science. And we’re letting them win.