Ever rolled over in bed and suddenly felt like the room was spinning? Or looked up at a shelf and got hit with a wave of dizziness so strong you had to grab onto something? If this sounds familiar, you might be dealing with BPPV - benign paroxysmal positional vertigo. It’s not dangerous, but it can feel terrifying. And worse, it’s often misdiagnosed as something else entirely.
BPPV is the most common cause of vertigo you’ve never heard of. It affects more than 2 in every 100 people over 40, and nearly 1 in 5 people who visit a doctor for dizziness end up with this diagnosis. It’s not a brain tumor, not a stroke, not even a migraine. It’s a tiny crystal - literally - that got loose in your inner ear and is sending your brain mixed signals. And the good news? There’s a simple, fast, and highly effective fix.
What Exactly Is BPPV?
BPPV stands for benign paroxysmal positional vertigo. Let’s break that down:
- Benign - It’s not life-threatening. No cancer. No brain damage.
- Paroxysmal - It comes in sudden bursts, usually lasting less than a minute.
- Positional - It’s triggered by specific head movements: rolling over, sitting up, bending down, or looking up.
- Vertigo - That spinning sensation, like you’re on a merry-go-round even when you’re still.
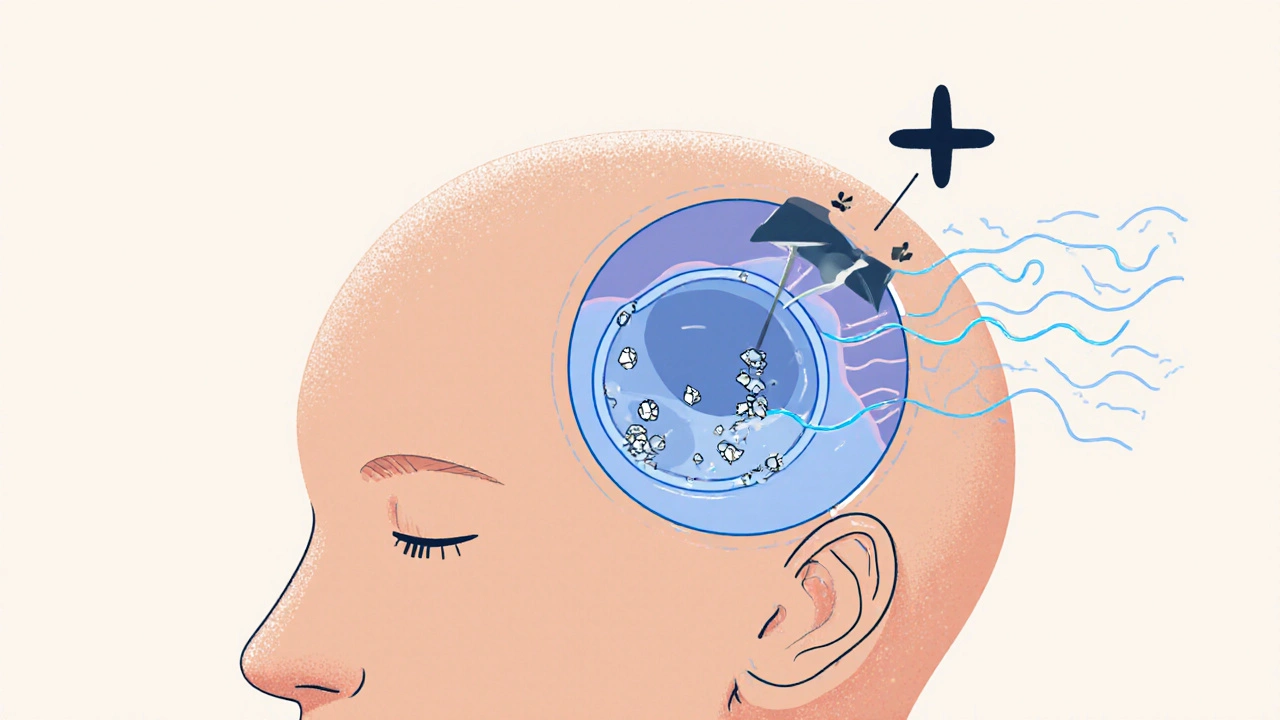
The problem starts in your inner ear, specifically in the vestibular system - the part that helps you balance. Inside this system are tiny calcium carbonate crystals called otoconia. Normally, they sit in a little sac called the utricle, helping you sense gravity and straight-up-and-down movement. But sometimes, for reasons we don’t fully understand, these crystals break loose. They drift into one of the three fluid-filled semicircular canals - tubes that sense head rotation.
When you move your head, the crystals shift the fluid inside the canal. That fluid normally tells your brain, “Hey, I’m turning left.” But when a loose crystal is floating around, it sends the wrong signal: “I’m spinning!” Even though you’re just turning over in bed. Your eyes jerk involuntarily (that’s called nystagmus), you feel nauseous, and your whole body feels off-balance. It’s a mismatch between what your eyes see, what your inner ear feels, and what your body knows - and your brain can’t reconcile it.
Who Gets BPPV - And Why?
BPPV doesn’t care about your fitness level or diet. It mostly shows up in people over 50. About 1 in 10 people over 70 will have it at least once. Women are 1.5 to 2 times more likely to get it than men. It can happen after a head injury, a fall, or even just from aging. In many cases, there’s no clear trigger - it just happens.
It’s not caused by stress, lack of sleep, or caffeine. You can’t catch it from someone else. And it’s not a sign of something worse - unless you have other symptoms like double vision, slurred speech, numbness, or weakness. Those would point to a central cause, like a stroke. BPPV is purely a problem in the inner ear.
Doctors can usually diagnose BPPV just by asking you a few questions and doing a quick test. The gold standard is the Dix-Hallpike maneuver. You sit on the edge of a table, the doctor turns your head to one side, then quickly lowers you backward so your head hangs off the table. If you have posterior canal BPPV (which is the case in 80-90% of people), you’ll feel dizzy within a few seconds - and your eyes will dart in a very specific way. The test is uncomfortable but not painful, and it ends as soon as the dizziness stops.
Why Most People Get It Wrong
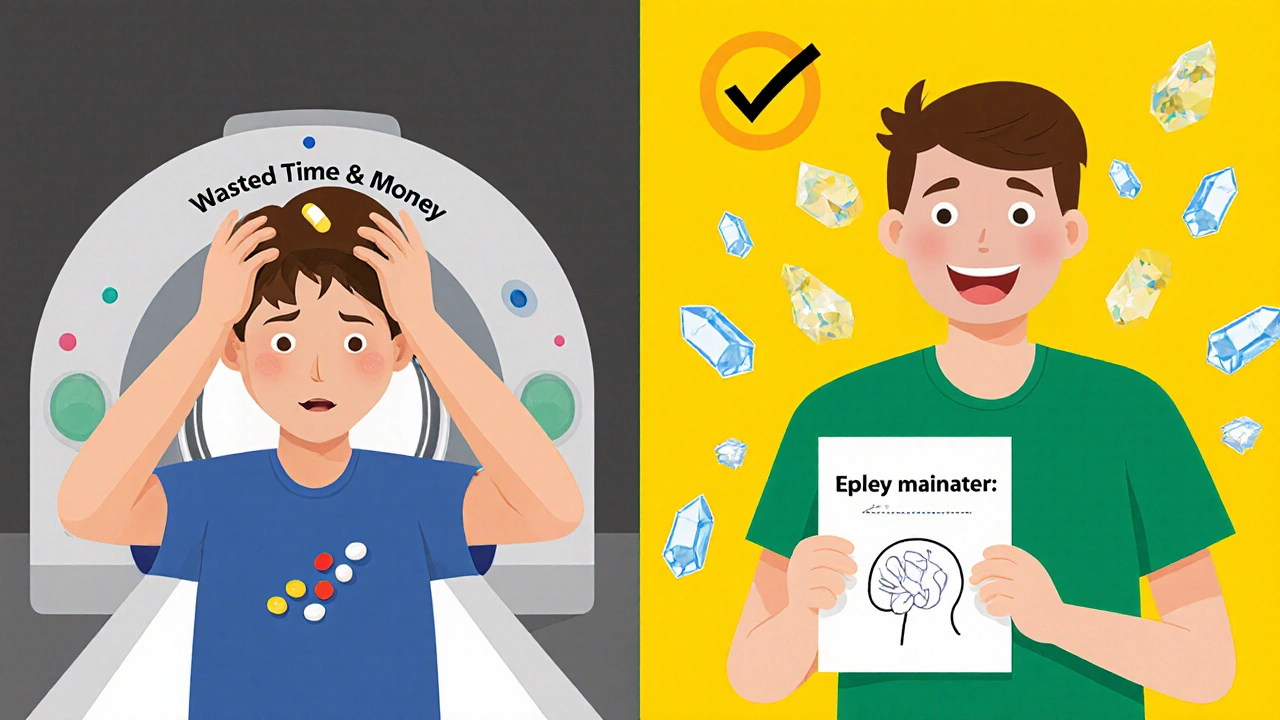
Here’s the frustrating part: BPPV is misdiagnosed in up to 35% of cases. Why? Because many doctors don’t know how to test for it. They hear “dizziness,” assume it’s an ear infection or anxiety, and hand you a prescription for meclizine or diazepam - drugs that make you sleepy and don’t fix the root problem.
Medications like meclizine only mask the symptoms for a few hours. They don’t move the crystals. And if you take them for days or weeks, you might delay the real fix. Worse, they can make you feel foggy, unsteady, or even more dizzy over time. The American Academy of Otolaryngology says vestibular suppressants should be avoided for BPPV unless nausea is severe and short-term.
Some patients get MRIs or CT scans - but those show nothing. The crystals are too small to be seen on imaging. An MRI might rule out a stroke, but if your symptoms match BPPV, you don’t need one. The Cochrane Review found that imaging has less than a 5% chance of finding anything useful in typical BPPV cases - and it adds $1,200 to $1,800 to your bill.
The Real Fix: Canalith Repositioning
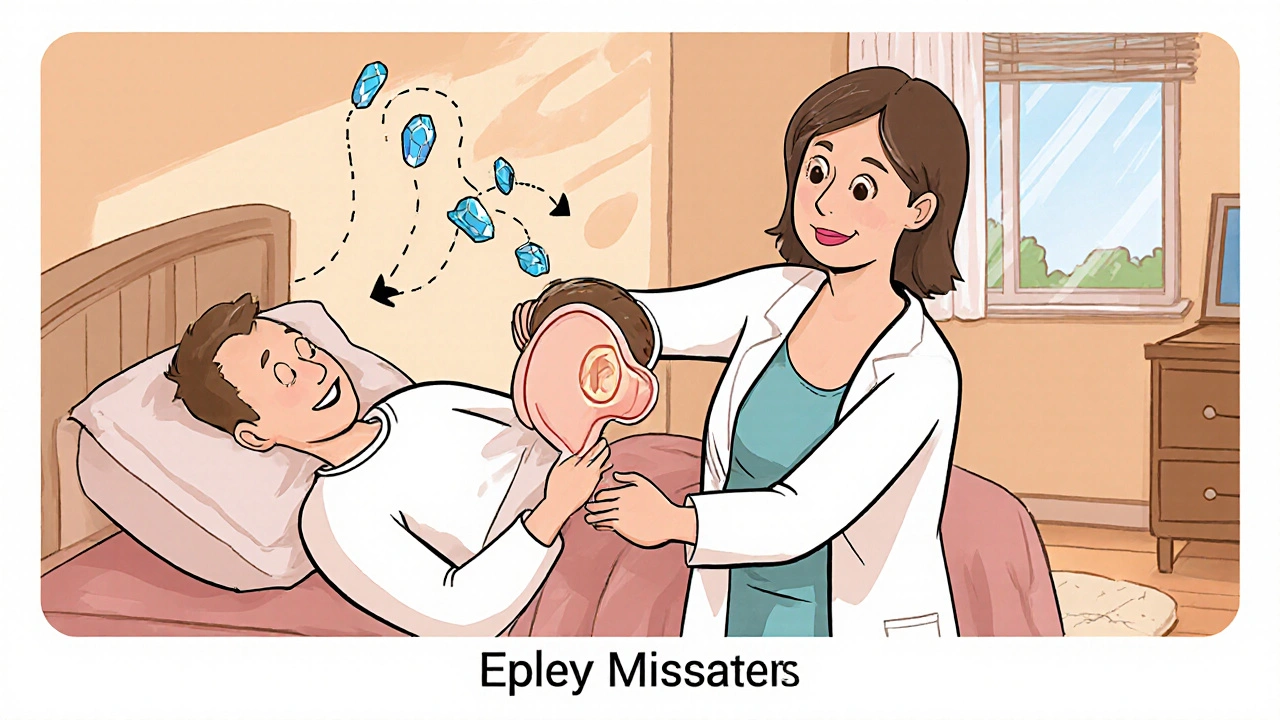
The cure for BPPV isn’t a pill. It’s a series of head movements - called canalith repositioning procedures. The most common one is the Epley maneuver. It’s not magic. It’s physics.
The goal is simple: guide the loose crystals out of the semicircular canal and back into the utricle, where they belong. The Epley maneuver does this by using gravity and precise head positioning. It’s done in a doctor’s office, but you can also do a modified version at home with a video guide.
Here’s how the Epley maneuver works for posterior canal BPPV:
- You sit upright on a bed, with your legs stretched out.
- The doctor turns your head 45 degrees toward the affected side.
- You lie back quickly, keeping your head turned, so your head hangs slightly off the bed.
- You wait 30-60 seconds until the dizziness and eye jerking stop.
- You turn your head 90 degrees to the opposite side, still lying down.
- You wait another 30-60 seconds.
- You roll onto your side, facing the floor, keeping your head turned.
- You wait 30-60 seconds again.
- You sit up slowly, keeping your head bent forward.
Each position lets gravity pull the crystals along the canal until they drop back into the utricle. The whole thing takes about 10 minutes. Most people feel better right away. Some feel a little off-balance for a day or two - that’s normal.
Success rates? Around 90% after one session. For horizontal canal BPPV (a rarer form), the Lempert roll is used instead. And if you’re not sure which canal is affected, a trained specialist can tell from the direction of your eye movements.
Can You Do It Yourself?
Yes - and many people do. A 2021 JAMA Otolaryngology study found that people who followed a video-guided Epley maneuver at home had a 72% success rate. That’s close to what you get in the clinic. Written instructions? Only 45% effective. Videos work because they show you the exact angle, timing, and speed.
But there are risks if you do it wrong:
- Moving too fast can make the crystals jump into another canal - turning posterior BPPV into horizontal BPPV.
- Not waiting long enough between positions means the crystals don’t settle.
- Doing it on the wrong side can make symptoms worse.
That’s why it’s best to get diagnosed first. If you’re unsure which ear is affected, try the Dix-Hallpike on both sides. The side that triggers stronger dizziness is likely the bad one. But if you’re confused, see a specialist. Physical therapists, audiologists, and ENTs are trained to do this.
What If It Comes Back?
BPPV loves to return. About 15% of people get it again within a year. By five years, it’s 35%. After ten years? Half of all patients will have had another episode.
That doesn’t mean it’s getting worse. It just means your inner ear is prone to losing crystals. Some people have it once and never again. Others get it every few years. There’s no way to prevent it completely - but one study found that people with low vitamin D levels had a 24% higher recurrence rate. Taking 1,000 IU daily might help if you’re deficient.
After treatment, avoid sleeping on the affected side for a few days. Some doctors recommend avoiding lying flat for 48 hours - though that’s debated. Most experts agree: don’t panic. If it comes back, just do the maneuver again.
What Doesn’t Work
Let’s clear up some myths:
- Vestibular suppressants - They don’t fix BPPV. They just make you drowsy.
- Chiropractic neck adjustments - No evidence they help. Could even be dangerous.
- Herbal supplements - Ginkgo biloba, ginger, or magnesium won’t move crystals.
- Acupuncture - Might help with nausea, but not the vertigo itself.
There’s one exception: the Brandt-Daroff exercises. These are home-based movements done twice a day for 10-14 days. They’re about 50% effective - slower than the Epley, but useful if you can’t access a provider. They work by helping your brain adapt to the false signals. But they don’t reposition the crystals. So if you want fast relief, go with repositioning.
When to See a Specialist
You don’t need to see a specialist right away - but you should if:
- Your dizziness lasts longer than a minute.
- You have hearing loss, ringing in your ears, or a feeling of fullness.
- You have numbness, weakness, trouble speaking, or double vision.
- You’ve had a head injury in the past week.
- Two Epley maneuvers didn’t help.
These could point to Meniere’s disease, vestibular neuritis, or something more serious. If you’re unsure, ask your doctor for a referral to a vestibular therapist or an ENT with balance expertise.
Many major hospitals now have vestibular rehab programs. In Toronto, places like Sunnybrook and Toronto Western offer these services. You can also find certified physical therapists who specialize in vertigo through the Canadian Physiotherapy Association.
The Bottom Line
BPPV is common, harmless, and fixable. It’s not a sign of aging - it’s a mechanical glitch. And the fix? A 10-minute maneuver that costs nothing but a little time. No pills. No scans. No surgery.
If you’ve been living with dizziness that comes and goes with head movements, don’t accept it as normal. Don’t keep taking pills that don’t work. Ask your doctor about the Dix-Hallpike test. If they don’t know it, ask for a referral. Or find a video guide and try the Epley maneuver yourself - after confirming which side is affected.
One treatment. One chance. And you might never feel dizzy again from this.
Is BPPV dangerous?
No, BPPV is not dangerous. It’s called "benign" because it doesn’t cause brain damage, stroke, or death. But the sudden spinning can lead to falls, especially in older adults. That’s why getting it treated quickly matters - not because the condition itself is risky, but because the symptoms can be unsafe.
Can BPPV go away on its own?
Yes, BPPV can resolve on its own, usually within a few weeks. But waiting means enduring dizziness, nausea, and balance problems. The Epley maneuver works in minutes, not weeks. Why suffer when you can fix it fast?
Why does my head feel weird after the Epley maneuver?
It’s normal to feel slightly off-balance or foggy for a day or two after the maneuver. That’s your brain adjusting to the fact that the crystals are no longer floating in the wrong place. It’s not a sign the treatment failed - it’s a sign it worked. Give yourself a day to recover.
Can I do the Epley maneuver twice in one day?
If your symptoms haven’t improved after one attempt, you can try again the same day - but wait at least an hour between attempts. Doing it too often or too fast can cause the crystals to move into another canal, making things worse. One well-performed maneuver is better than three rushed ones.
What’s the difference between BPPV and Meniere’s disease?
BPPV causes short bursts of vertigo triggered by head movement. Meniere’s causes longer episodes (20 minutes to hours), often with ringing in the ear, hearing loss, and pressure. BPPV doesn’t affect hearing. Meniere’s does. The treatments are completely different - BPPV needs repositioning; Meniere’s needs diet changes, diuretics, or injections.
Do I need an MRI for BPPV?
No. If your symptoms match BPPV - brief dizziness with head movement, no hearing loss or neurological signs - an MRI won’t help. It costs money and exposes you to unnecessary stress. Doctors should only order imaging if something doesn’t fit the classic picture.
Can stress cause BPPV?
Stress doesn’t cause BPPV. But it can make you more aware of your symptoms and worsen your anxiety about them. That can make the dizziness feel worse. The root cause is always a loose crystal in the inner ear - not anxiety or tension.
How many times do I need the Epley maneuver?
Most people feel better after one session. About 15% need a second one, and fewer than 5% need a third. If you don’t improve after two attempts, you might have a different type of vertigo - or the maneuver wasn’t done correctly. See a specialist for confirmation.
Brian Bell
November 14, 2025 AT 22:19Scarlett Walker
November 16, 2025 AT 03:15Sean Evans
November 16, 2025 AT 06:43Ashley Durance
November 16, 2025 AT 17:00Ryan Anderson
November 18, 2025 AT 00:28Anjan Patel
November 19, 2025 AT 20:31gent wood
November 20, 2025 AT 05:14Nathan Hsu
November 20, 2025 AT 20:43Eleanora Keene
November 21, 2025 AT 11:32Kevin Wagner
November 22, 2025 AT 02:17Hrudananda Rath
November 22, 2025 AT 09:52Don Ablett
November 22, 2025 AT 10:47Scott Saleska
November 23, 2025 AT 01:45Brittany C
November 23, 2025 AT 07:56Joe Goodrow
November 23, 2025 AT 19:43