Imagine sitting down at your favorite sushi place, excited for a bowl of miso soup, only to realize the broth contains shrimp paste. Or worse - you’ve eaten it before without issue, but now your lips are tingling, your throat feels tight, and you’re not sure if it’s just a bad reaction or something serious. For the shellfish allergy community, this isn’t hypothetical. It’s a daily reality.
What Exactly Is a Shellfish Allergy?
A shellfish allergy isn’t just being sensitive to seafood. It’s an immune system overreaction to specific proteins found in marine invertebrates. Unlike fish allergies, which are triggered by parvalbumin, shellfish allergies are almost always caused by tropomyosin - a protein that’s shockingly similar across shrimp, crab, lobster, and crawfish. This protein doesn’t break down when cooked. That means grilled, fried, or boiled shellfish? Still dangerous. About 2% of people worldwide have this allergy. In adults over 40, the rate jumps to nearly 4%. And here’s the twist: you don’t need to eat shellfish to become allergic. Many people develop sensitization through dust mites or cockroaches. Their immune systems see tropomyosin in mites and think, "This looks like shrimp." So when they later eat shrimp, their body goes into full alarm mode - even if they’ve never had a reaction before.Cross-Reactivity: Why One Allergy Can Mean Avoiding Everything
Not all shellfish are created equal when it comes to cross-reactivity. Crustaceans - shrimp, crab, lobster - share over 95% of their tropomyosin structure. If you’re allergic to shrimp, you have a 75% chance of reacting to crab or lobster. The risk is even higher between shrimp and crab - up to 92% IgE binding similarity. Mollusks are a different story. Clams, oysters, scallops, and mussels have very different proteins. Only 15-20% of people allergic to shrimp will react to these. That’s why some allergists now recommend testing for specific proteins before cutting out entire food groups. If your IgE is only reacting to tropomyosin and not to other mollusk proteins, you might safely eat scallops - even if you can’t touch shrimp. But here’s where things get messy: many people test positive for shellfish on blood tests without ever having symptoms. Why? Because their immune system is cross-reacting with dust mites. A 2025 study found that 68% of dust mite-allergic patients had IgE antibodies to shellfish - but only 12% of them actually got sick when eating it. That’s a false positive. And if your doctor only does a standard shellfish extract test, you might be unnecessarily avoiding crab for life.Diagnosis: Don’t Rely on Blood Tests Alone
Standard skin prick tests and IgE blood tests can be misleading. A positive result doesn’t always mean you’ll have a reaction. That’s why component-resolved diagnostics (CRD) are changing the game. Instead of testing for whole shellfish extracts, CRD looks at specific proteins: tropomyosin, sarcoplasmic calcium-binding protein (SCBP), arginine kinase. If your IgE is high for tropomyosin, you’re likely allergic to all crustaceans. If it’s high for SCBP, you’re probably allergic to shrimp - and possibly more sensitive to heat-stable proteins. If your IgE is low for tropomyosin but high for mites? You might be fine eating shellfish. The gold standard? An oral food challenge - done under medical supervision. If your history and tests are unclear, this is the only way to know for sure. Many people are told they’re allergic based on a single reaction years ago, but with proper testing, they find out they can eat lobster after all.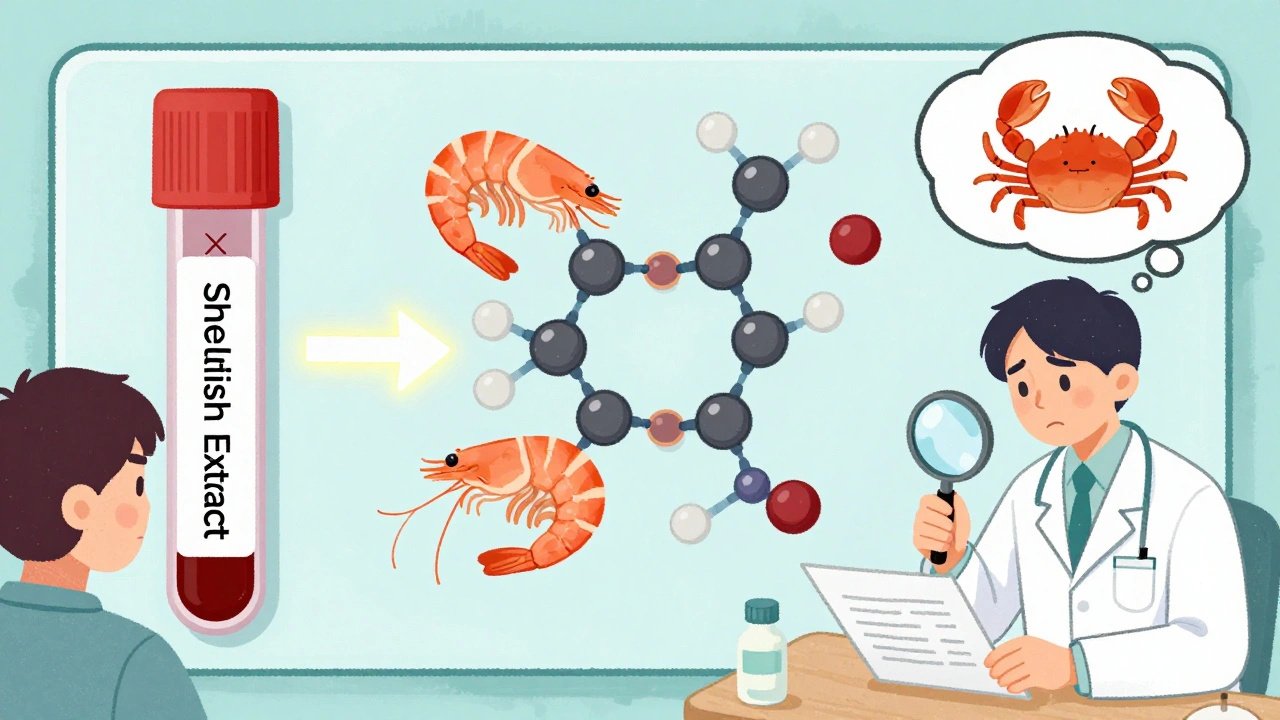
Dining Out: The Real Danger Isn’t the Menu - It’s the Kitchen
Most allergic reactions don’t happen because someone added shrimp to your dish. They happen because the same oil fried your fries after shrimp. Or the same grill touched your steak after grilled shrimp skewers. Or the server didn’t know the soy sauce had anchovy or shrimp paste. A 2022 survey found 68% of people with shellfish allergies had at least one accidental exposure while dining out. Nearly a quarter needed epinephrine. The biggest trouble spots? Asian restaurants (41% of reactions), seafood joints (87% of all reactions), and places with shared fryers. Here’s what actually works:- Call ahead - 24 hours in advance. Ask to speak to the chef, not just the server. Servers are often trained to say "yes" to avoid conflict. Chefs know the truth.
- Use a chef card - printed, clear, in the restaurant’s language. FARE’s cards are available in 15 languages. Don’t rely on "I’m allergic to shrimp." Say: "I have a life-threatening allergy to crustaceans. Cross-contact with shrimp, crab, or lobster can trigger anaphylaxis. Please use clean utensils, pans, and oil. No sauces, broths, or seasonings containing shellfish."
- Avoid restaurants with seafood on the menu unless they have a dedicated fryer and prep area. Shared oil causes 63% of crustacean reactions.
- Use apps like AllergyEats or Nosh List. They’re built by people with allergies who’ve been burned (literally). 120,000+ users report which restaurants are safe.
Hidden Ingredients: The Sneaky Culprits
Shellfish isn’t always obvious. It’s in:- Broths and soups (especially in Asian cuisines - fish sauce, shrimp paste)
- Seasonings and spice blends (some "seafood flavoring" is made from ground crab or shrimp)
- Surimi (imitation crab meat - often made from pollack but processed with crab extract)
- Salad dressings and marinades (fish sauce, oyster sauce)
- Even some vitamins and supplements - shellfish-derived glucosamine is common

What About Shellfish-Free Alternatives?
There’s no perfect substitute for the taste of shrimp or crab. But plant-based options are improving fast. Companies like Good Catch and Ocean Hugger Foods make vegan seafood using pea protein and seaweed extracts. They don’t contain tropomyosin. They’re safe. They’re not perfect - texture and flavor are still evolving - but they’re getting better every year. Some people with shellfish allergies also avoid iodine, thinking it’s the trigger. That’s a myth. Iodine isn’t an allergen. It’s a mineral. People react to proteins - not iodine. You can safely get iodine from table salt, dairy, or eggs.What’s Next? New Treatments on the Horizon
There’s hope. In early 2024, Phase 2 results from a peptide immunotherapy trial at Mount Sinai showed 70% of participants with shrimp allergy could tolerate small amounts after 6 months of daily drops under the tongue. No anaphylaxis. No epinephrine needed. It’s not a cure - but it’s a shield. The FDA approved a new diagnostic panel in 2024 (ImmunoCAP ISAC 112) that can now tell you whether your IgE is reacting to shellfish - or just to dust mites. This means fewer people are unnecessarily avoiding crab for life. AI tools are also emerging. Apps like AllergyMapper, launched in March 2024, scan restaurant menus and flag hidden shellfish ingredients with 85% accuracy. They’re not perfect - but they’re helping people make smarter choices.Final Advice: Knowledge Is Your Best Defense
Living with a shellfish allergy isn’t about fear. It’s about strategy. You don’t have to give up dining out. You just need to know how to ask the right questions, recognize the hidden risks, and trust your own judgment over a server’s guess. Carry two epinephrine auto-injectors. Always. Even if you think you’re "just a little allergic." Reactions can get worse with each exposure. Educate your friends and family. A 2023 study found that 82% of allergic reactions happened in social settings - parties, restaurants, potlucks. If your friend doesn’t know what "cross-contact" means, they might accidentally put shrimp in your pasta. And remember: you’re not alone. Millions of people navigate this every day. The tools are better. The awareness is growing. And with the right knowledge, you can eat out - safely - without missing out on life’s flavors.Can you outgrow a shellfish allergy?
Unlike milk or egg allergies, shellfish allergy is rarely outgrown. Only about 10-15% of children with shellfish allergy lose it by adulthood. Most people who develop it after age 12 keep it for life. That’s why accurate diagnosis and long-term management are so important.
Is it safe to eat scallops if I’m allergic to shrimp?
Possibly - but not automatically. Scallops are mollusks, and cross-reactivity with crustaceans like shrimp is low (15-20%). However, some people react to both. Component-resolved diagnostics can help. If your IgE only binds to tropomyosin (found in shrimp) and not to mollusk-specific proteins, you might tolerate scallops. Always test under medical supervision before trying.
Why do I test positive for shellfish but never have symptoms?
You likely have cross-reactive IgE from dust mites or cockroaches. These bugs contain tropomyosin, the same protein found in shrimp. Your immune system gets confused and makes antibodies to it - but without actual exposure to shellfish, you never react. This is called "asymptomatic sensitization." Component testing can tell you if your IgE is truly shellfish-specific or just mite-related.
Can I eat at a sushi restaurant if I have a shellfish allergy?
It’s risky. Many sushi restaurants use shellfish in broths, sauces, and even in the rice seasoning. Even if your roll doesn’t have shrimp, the same knife or cutting board might have touched it. Call ahead. Ask if they have a dedicated prep area. Avoid anything with imitation crab, tobiko, or fish sauce. Stick to simple grilled fish or tofu dishes - and bring your chef card.
Do I need to avoid iodine if I have a shellfish allergy?
No. Iodine is not an allergen. Shellfish allergy is triggered by proteins like tropomyosin - not iodine. People with shellfish allergies can safely receive iodine-based contrast dyes, eat iodized salt, or take supplements with iodine. The myth that shellfish allergy means iodine allergy is outdated and dangerous - it’s led to unnecessary avoidance of medical procedures.
Are there any restaurants that are reliably safe for shellfish allergies?
Some chains have strong allergen protocols. Chipotle, Panera Bread, and Sweetgreen all use digital allergen menus with 98% accuracy. They train staff, separate prep areas, and update ingredient lists daily. Independent restaurants vary wildly. Use apps like AllergyEats or Nosh List - they’re built by people with allergies who’ve tested the restaurants firsthand. Don’t rely on a restaurant’s website alone.

iswarya bala
December 10, 2025 AT 04:16Lisa Whitesel
December 10, 2025 AT 08:31Larry Lieberman
December 12, 2025 AT 07:24Richard Eite
December 13, 2025 AT 02:18Katherine Chan
December 14, 2025 AT 09:00Philippa Barraclough
December 15, 2025 AT 08:45Angela R. Cartes
December 15, 2025 AT 23:54George Taylor
December 16, 2025 AT 15:21Tim Tinh
December 18, 2025 AT 08:32Courtney Black
December 19, 2025 AT 03:48Asset Finance Komrade
December 20, 2025 AT 16:29Steve Sullivan
December 22, 2025 AT 05:11Carina M
December 22, 2025 AT 05:44om guru
December 23, 2025 AT 15:25Anna Roh
December 24, 2025 AT 12:27