Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these mistakes happen because someone didn’t double-check the medication name, the strength, or the dosage form before giving or taking a drug. It’s not always a pharmacist’s mistake. It’s not always a doctor’s. Sometimes, it’s just a quick glance at a label that missed a tiny but deadly detail. You don’t need to be a doctor to prevent these errors. You just need to know how to check properly.
Why Checking Medication Details Matters
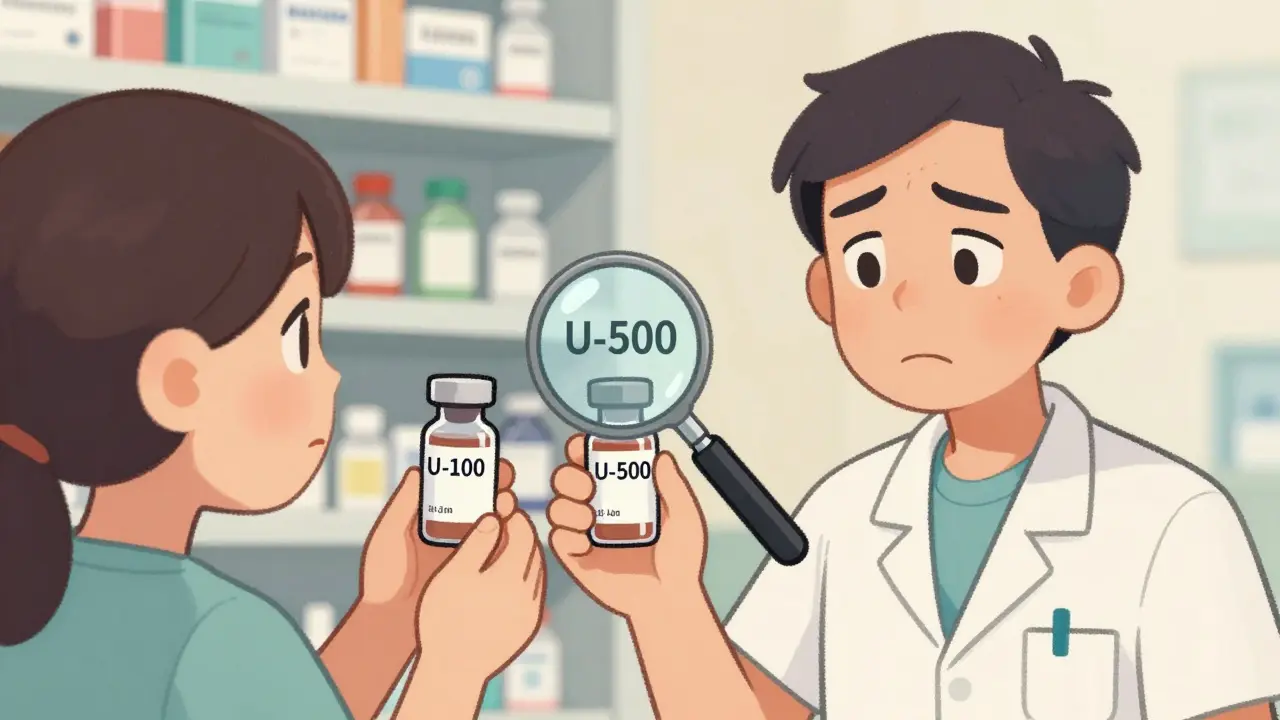
Think about insulin. One vial says U-100. Another says U-500. They look almost identical. If you grab the wrong one, you could give yourself five times the dose-and that could kill you. That’s not hypothetical. In 2023, over 300 insulin-related errors were reported to the FDA, mostly because someone confused the strength. The same thing happens with heparin, epinephrine, and morphine. These are called high-alert medications because even a small mistake can lead to death. The problem isn’t just about dangerous drugs. It’s about how information is written. A label that says 10mg without a space can be misread as 100 mg. A handwritten U for units can look like a 0. A prescription that says MS could mean morphine sulfate-or magnesium sulfate. Two completely different drugs. One saves lives. The other can end them. The Institute for Safe Medication Practices (ISMP) says the most dangerous abbreviation isn’t a letter or symbol-it’s the absence of the strength. If a prescription doesn’t clearly state the dose, people guess. And guessing with meds is never safe.What to Check: The Three Critical Pieces
Every time you handle a medication-whether you’re picking it up at the pharmacy, giving it to a loved one, or taking it yourself-verify these three things:- Drug Name - Is it spelled correctly? Does it match the prescription? Watch out for look-alike names like prednisone and prednisolone, or hydroxyzine and hydroxyurea. Many hospitals now use Tall Man lettering to make these stand out: predniSONE vs. predniSOLONE.
- Strength - What’s the amount? Is it 5 mg, 50 mg, or 500 mg? Always confirm the unit: mg, mcg, mL, units. Never assume. If it says 0.5 mg, make sure it’s not written as .5 mg. Leading zeros matter. If it says 5000 units/mL, check if it’s supposed to be 50 units/mL. That’s a 100-fold difference.
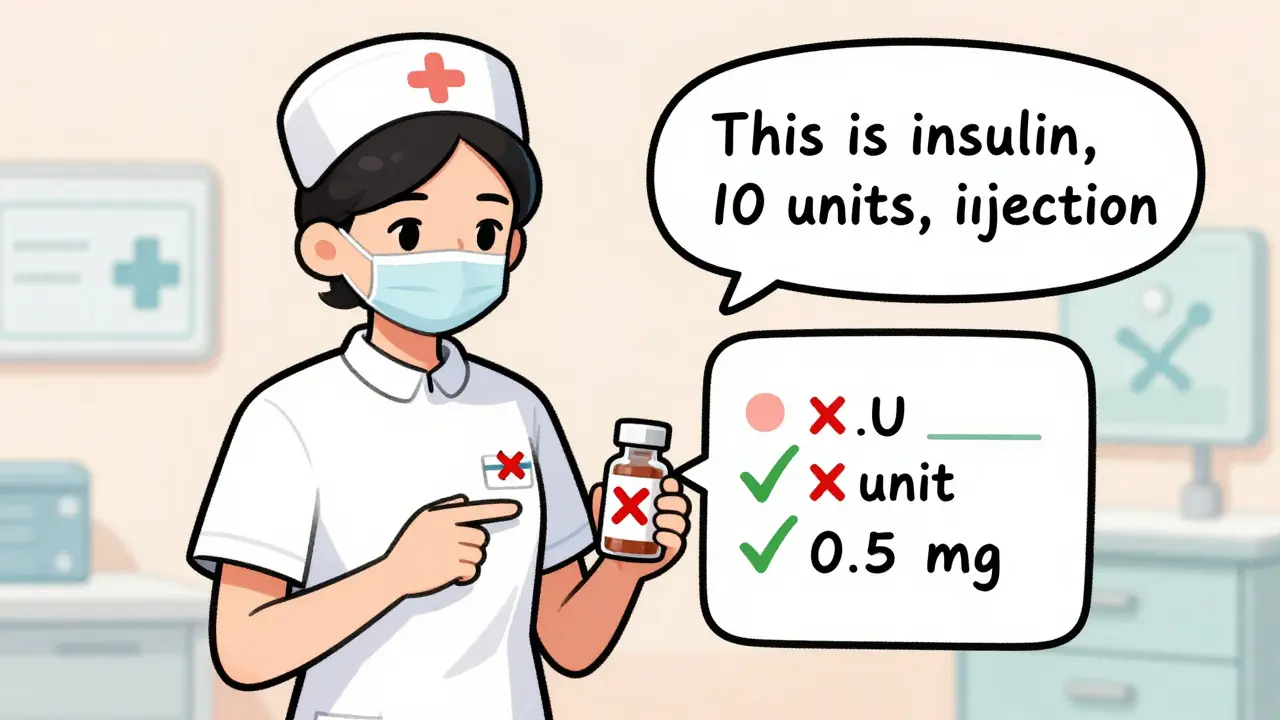
- Dosage Form - Is it a tablet, capsule, liquid, patch, or injection? Giving a pill meant to be swallowed when it’s actually a suppository can be dangerous. Oral medications should never be injected. Topical creams shouldn’t be taken by mouth. The form tells you how to use it-and if you’re wrong, you’re risking harm.
How to Verify: A Step-by-Step Process
You don’t need fancy tools. You just need to slow down and follow three key steps:- Check the prescription or order - Before you even touch the medication, look at the written or electronic order. Does it include the full drug name, exact strength with units, and dosage form? If any part is missing, unclear, or abbreviated, stop. Ask for clarification.
- Compare it to the label on the container - Hold the medication bottle or package next to the prescription. Read the name, strength, and form out loud. Match each part. If the label says Amoxicillin 500 mg capsule but the order says 500 mg tablet, don’t give it. Call the prescriber.
- Confirm before giving or taking it - This is your last line of defense. Before swallowing, injecting, or applying the drug, say it out loud: “This is [drug name], [strength], [dosage form] for [patient name].” This is called the read-back method. Nurses who use it reduce errors by nearly 90%. It works for patients too.
Common Mistakes That Lead to Errors
Even experienced people make the same mistakes over and over. Here are the top ones:- Using abbreviations - Never write or rely on U for units, μg for micrograms, or q.d. for daily. Use unit, mcg, and daily. The FDA and ISMP banned these abbreviations for a reason.
- Ignoring decimal points - Writing .5 mg instead of 0.5 mg can lead to a tenfold overdose. Always use a leading zero for numbers under 1.
- Assuming the label is correct - Pharmacies make mistakes too. A 2020 study found that barcode scanning cut dispensing errors by 83%. But if you skip the check because the scanner beeped, you’re still at risk.
- Not checking the vial or package - Some medications come in similar-looking bottles. Heparin vials, for example, can have different strengths stored side by side. Always read the actual vial-not just the box.
What to Do When Something Doesn’t Look Right
If you spot a mismatch, don’t ignore it. Don’t assume it’s a typo. Don’t think, “It’s probably fine.” Here’s what to do:- Stop. Don’t proceed.
- Compare the order, the label, and the medication one more time.
- If it still doesn’t match, contact the prescriber or pharmacist. Say: “I’m seeing a discrepancy between the order and the label. Can you confirm the strength and form?”
- Document what you saw. Even if you’re a patient, write down the details. You might need to refer to them later.

Tools That Help (But Don’t Replace Your Brain)
Technology can help, but it’s not perfect. Electronic health records (EHRs) can flag look-alike names. Barcode scanners verify the right drug is going to the right person. But:- Systems can glitch. A 2022 study found 41% of pharmacists said their EHR didn’t flag dangerous strength combinations.
- Alert fatigue is real. If a system beeps 20 times an hour, people start ignoring it.
- AI tools are emerging, like Google Health’s image recognition for labels, but they’re still in testing. Don’t rely on them yet.
What You Can Do Right Now
You don’t need to wait for a hospital policy or a new app. Start today:- When you pick up a new prescription, read the label out loud and compare it to the doctor’s instructions.
- Keep a list of your meds, including name, strength, and form, in your phone or wallet.
- If you’re helping someone else, always verify before giving the dose-even if you’ve done it a hundred times before.
- Ask your pharmacist: “Is this the right strength and form for what was prescribed?” They’re trained to catch errors.
Final Thought: Safety Is a Habit, Not a One-Time Check
Medication safety isn’t about being perfect. It’s about being consistent. One missed check can have lifelong consequences. But if you make checking the name, strength, and form a habit-every single time-you’re not just protecting yourself. You’re protecting everyone around you.What if the medication label doesn’t match the prescription?
Stop immediately. Do not take or give the medication. Contact the prescribing doctor or pharmacist to confirm the correct details. Never assume it’s a typo or that it’s close enough. Even small differences in strength or form can be dangerous. Document the discrepancy in case you need to refer to it later.
Why is spacing important in medication labels?
Spacing prevents misreading. For example, "10mg" can be mistaken for "100 mg" if the space is missing. The ISMP found that simply adding a space between the number and unit (e.g., "10 mg") reduces medication errors by about 12%. Always write and read strengths with a space: "5 mg", "0.5 mL", "1000 units".
Are abbreviations like "U" or "μg" still allowed?
No. Abbreviations like "U" for units and "μg" for micrograms are banned by the FDA and ISMP because they’re easily misread. "U" can look like a "0" or a "4," leading to 10-fold dosing errors. "μg" can be mistaken for "mg." Always use "unit" and "mcg" instead. These are the only safe forms.
What are high-alert medications?
High-alert medications are drugs that carry a higher risk of serious harm if used incorrectly. Examples include insulin, heparin, epinephrine, morphine, and potassium chloride. Even small mistakes-like giving the wrong strength or form-can cause death. These drugs require extra verification steps, including double-checking by two people in hospitals and always confirming the label before use.
Can I trust the barcode on the medication package?
Barcodes reduce errors by 83% when used correctly, but they’re not foolproof. If the label is damaged, the barcode is misprinted, or the system is outdated, it can scan the wrong item. Always visually verify the drug name, strength, and form-even if the scanner beeps. Never rely on technology alone.
How can I help a family member avoid medication errors?
Keep a written or digital list of all their medications, including name, strength, form, and purpose. Always check the label against the list before each dose. Use the read-back method: say the name, strength, and form out loud before giving it. Ask their pharmacist to review all meds at least once a year. Don’t assume the doctor or pharmacist caught everything.
Neil Ellis
January 22, 2026 AT 07:26Man, I never realized how many tiny things can kill you with meds. I used to just grab my insulin and go-now I read every label like it’s a treasure map. That U-100 vs U-500 thing? Chilling. I’m telling my whole family to start saying the dose out loud before they take anything. Small habit, massive safety net.
Lana Kabulova
January 23, 2026 AT 08:13STOP. USING. ABBREVIATIONS. I swear-every time I see 'U' on a label, I want to scream. It's not 'units'-it's 'you're gonna die.' And don't even get me started on .5mg vs 0.5mg. One missing zero, and boom-ER. Why is this still a thing? The FDA banned these for a reason. Use. The. Words.
Rob Sims
January 24, 2026 AT 07:27Oh wow. Another ‘be careful with meds’ post. Groundbreaking. Next you’ll tell us not to drink bleach. Look-I get it, mistakes happen. But most people aren’t idiots. They read the label. They check the bottle. You’re treating patients like toddlers. The system’s broken-not the people. Fix the damn EHRs before preaching to the choir.
Kenji Gaerlan
January 25, 2026 AT 07:52so like… if u see a med that says 10mg but the doc said 100mg… u just stop? no like… what if its a typo? maybe the doc just forgot the 0? i mean, its not like we all got phd in med stuff. maybe just call the pharmacy? idk. just saying… dont panic.
Margaret Khaemba
January 26, 2026 AT 04:12I’m a caregiver for my mom, and this post saved me. Last week I caught a mismatch on her blood thinner-label said 5mg, script said 2.5mg. I called the pharmacy and they admitted the barcode got scanned wrong. They thanked me. I told them I just read it out loud like you said. Seriously, if you’re taking meds or helping someone, do this. It’s not hard. It’s just… not automatic.
Malik Ronquillo
January 26, 2026 AT 22:16People are dying because they’re too lazy to read. That’s it. No fancy tech, no magic app. Just eyes. And a brain. And the guts to say ‘wait, this doesn’t look right.’ I’ve seen nurses roll their eyes at the ‘read-back’ thing. Then they give the wrong dose. And now someone’s dead. Don’t be that person. Slow down. It’s not that hard.
Brenda King
January 28, 2026 AT 01:13My grandma used to write her meds on a sticky note. I helped her update it every month. Name, strength, form. Even the time of day. She never had a mix-up. Simple. No apps. No scanners. Just pen and paper. And a little patience. You don’t need tech to be safe. You just need to care enough to write it down.
Keith Helm
January 29, 2026 AT 12:31Verification protocols are not optional. They are mandatory. The absence of standardized pre-administration checks constitutes a systemic failure. Compliance with ISMP guidelines is not a suggestion. It is a clinical imperative.
Daphne Mallari - Tolentino
January 30, 2026 AT 03:29While the intent of this missive is laudable, one cannot help but observe the conspicuous absence of empirical data quantifying the efficacy of the 'read-back method' in non-clinical, home-based environments. The cited 90% reduction statistic pertains exclusively to institutional nursing protocols. Extrapolating this to laypersons is statistically dubious and potentially misleading.
Alec Amiri
January 30, 2026 AT 06:35Yeah yeah, 'check your meds'-but let's be real. The system is rigged. Pharmacies mix up bottles. Doctors typo prescriptions. EHRs glitch. And then they blame the patient? Nah. You want to stop errors? Fix the system. Don't put the burden on grandma trying to read tiny print at 7 a.m. with her reading glasses on backwards.
Patrick Roth
January 30, 2026 AT 17:34Actually, in Ireland, we just use the brand name. No confusion. No U-100 nonsense. We don’t have 17 different generics for everything. Maybe if the US stopped letting Big Pharma rename every drug under the sun, we wouldn’t need this whole checklist. Just sayin’.
Oren Prettyman
January 31, 2026 AT 18:14It is worth noting that the majority of medication errors occur not during administration, but during transcription-specifically during the transition from handwritten prescriptions to electronic systems. The focus on patient-facing verification, while commendable, is misdirected. The true root cause lies in the interoperability failures between prescriber platforms and pharmacy dispensing systems. Until these backend systems are standardized and audited with regulatory rigor, patient-level interventions remain symptomatic treatment rather than curative.
Hilary Miller
January 31, 2026 AT 20:07Just read the label. Out loud. Every time. It’s that simple.