Hormone Therapy Decision Guide
Personalized Treatment Assessment
This tool helps determine which hormone therapy might be most suitable for your specific medical profile. Please answer the following questions based on your current health status.
If you’ve been diagnosed with hormone‑receptor‑positive breast cancer, odds are you’ve heard the names Letrozole and Tamoxifen tossed around. Both are staples in endocrine therapy, yet they work very differently and suit different patients. This guide breaks down the science, the side‑effect profile, and the real‑world factors that decide which drug might be the better fit for you.
What the drugs actually are
First, let’s get clear on the basics.
Letrozole is an aromatase inhibitor that blocks the enzyme aromatase, cutting estrogen production in postmenopausal women. It’s taken as a 2.5 mg tablet once daily.
Tamoxifen is a selective estrogen receptor modulator (SERM) that blocks estrogen receptors in breast tissue while partially activating them elsewhere. The standard dose is 20 mg once daily.
Both aim to starve estrogen‑driven tumors, but they do it from opposite ends of the hormone pathway.
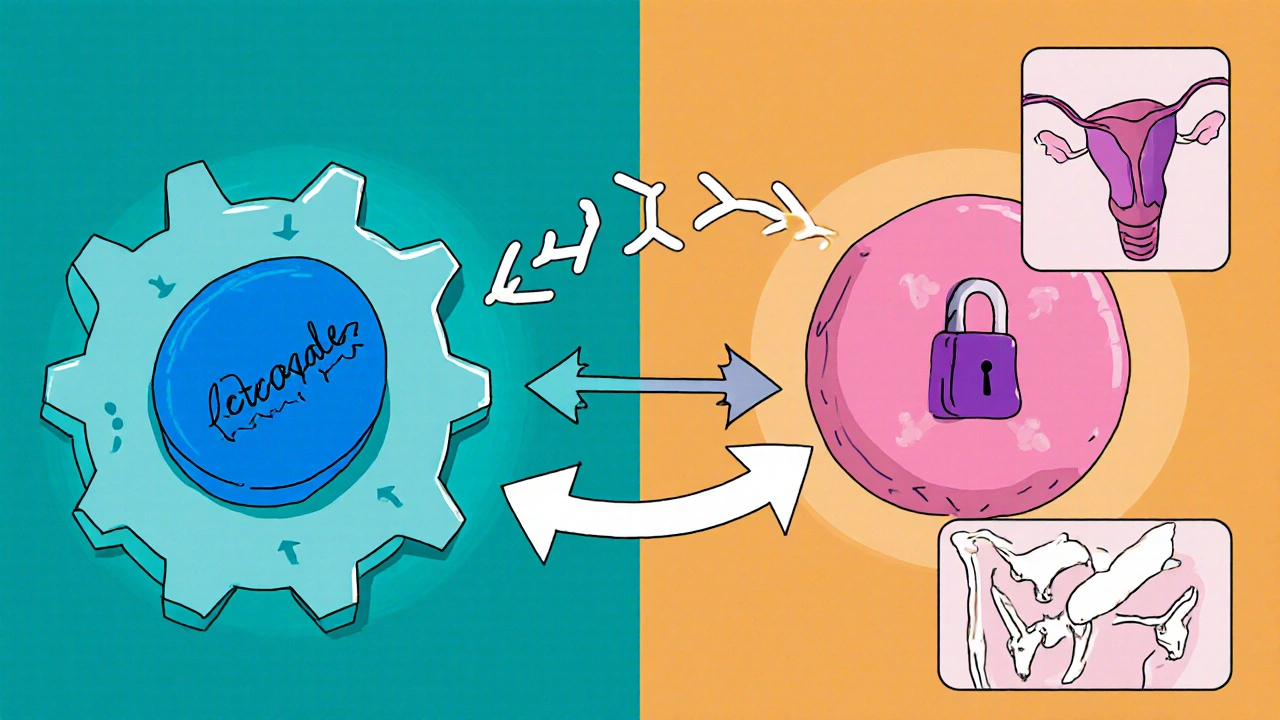
How they work - mechanism of action
- Aromatase inhibition (Letrozole): In postmenopausal women, most estrogen comes from the conversion of androgens via the aromatase enzyme. Letrozole binds tightly to aromatase, reducing circulating estrogen to less than 10% of normal levels.
- SERM activity (Tamoxifen): Tamoxifen competes with estrogen for the estrogen receptor (ER) in breast cells. When it binds, it blocks the receptor’s ability to trigger tumor growth. In bone and the uterus, it can act like estrogen, which explains some of its unique side‑effects.
Because Letrozole slashes estrogen production, it’s most effective in women who no longer have ovaries producing estrogen - i.e., postmenopausal patients. Tamoxifen, on the other hand, works regardless of menopausal status, making it the go‑to for premenopausal women.
Who should take which drug?
The choice often boils down to three patient factors: menopausal status, risk of bone loss, and personal tolerance for certain side effects.
| Attribute | Letrozole (Aromatase Inhibitor) | Tamoxifen (SERM) |
|---|---|---|
| Mechanism | Blocks estrogen synthesis | Blocks estrogen receptors in breast, partial agonist elsewhere |
| Typical patient | Postmenopausal women | Premenopausal & postmenopausal women |
| Common dose | 2.5 mg daily | 20 mg daily |
| Key side effects | Joint pain, bone loss, hot flashes | Hot flashes, risk of endometrial cancer, deep‑vein thrombosis |
| Impact on bone | Decreases bone mineral density | Preserves or modestly improves bone density |
| Cardiovascular risk | Neutral to slight increase | Higher risk of blood clots |
| FDA‑approved duration | 5 years (can be extended to 10) | 5 years (option to switch after 2-3 years) |
How effective are they?
Large Phase III trials give us solid numbers.
The BIG 1‑98 study randomized postmenopausal women to letrozole, anastrozole, exemestane, or tamoxifen. Letrozole showed a 2.5% absolute improvement in disease‑free survival (DFS) over tamoxifen after five years (84.0% vs 81.5%). The hazard ratio (HR) was 0.81, meaning a 19% lower risk of recurrence.
In premenopausal cohorts, tamoxifen remains the standard because aromatase inhibitors are ineffective without ovarian suppression. Added ovarian suppression (e.g., with goserelin) can bring an AI into play, but that adds complexity and cost.
Overall, for postmenopausal patients, aromatase inhibitors-including letrozole-tend to edge out tamoxifen in preventing recurrence, especially in higher‑risk disease.
Side‑effect deep dive
Both drugs are generally well‑tolerated, but the side‑effect profile can tip the balance.
Bone health is a major concern with aromatase inhibitors because reducing estrogen accelerates bone resorption. Studies report a 2-3% annual loss in lumbar spine BMD with letrozole. Calcium, vitamin D, and bisphosphonates are often prescribed alongside.
Tamoxifen, by contrast, acts like estrogen on bone, which can actually improve BMD in postmenopausal women. However, its estrogen‑like activity in the uterus raises the risk of endometrial hyperplasia and, rarely, cancer. The absolute increase is about 0.5 cases per 1,000 women per year, but it’s a factor to discuss with your oncologist.
Joint and muscle aches (arthralgia) are reported by 30-40% of patients on letrozole, sometimes severe enough to cause discontinuation. Switching to tamoxifen or adding analgesics can help.
Both agents can cause hot flashes, but tamoxifen patients often describe them as more intense because the drug blocks estrogen receptors in the brain’s thermoregulatory center.
Venous thromboembolism (VTE) risk is higher with tamoxifen-about 2-3 times the baseline. For patients with a personal or family history of clotting, letrozole may be a safer bet.
Special populations and practical tips
- Premenopausal women: Tamoxifen is the first line unless ovarian suppression is planned. Letrozole alone won’t work.
- Patients with osteoporosis: Letrozole can worsen bone loss. Consider baseline DEXA scan; if T‑score < ‑2.0, a bisphosphonate or switching to tamoxifen may be wiser.
- History of endometrial cancer: Avoid tamoxifen; letrozole is preferred.
- High cardiovascular risk: Both drugs are relatively safe, but tamoxifen’s clotting risk warrants caution. Low‑dose aspirin may be discussed.
- Adherence concerns: Letrozole’s once‑daily 2.5 mg pill is easy, but joint pain can discourage use. Tamoxifen’s 20 mg pill is also simple but requires monitoring for VTE.
Making the decision - a quick checklist
- Are you postmenopausal? If yes, both are options; if no, stick with tamoxifen (or add ovarian suppression).
- Do you have osteoporosis or low bone density? Consider tamoxifen or add bone‑protective therapy.
- Any prior endometrial issues? Letrozole is safer.
- History of blood clots? Letrozole carries lower VTE risk.
- Can you tolerate joint pain? If not, tamoxifen may be more comfortable.
- Discuss duration and the possibility of switching after 2‑3 years - many clinicians start with tamoxifen then switch to an AI for added benefit.
Ultimately, the choice is a partnership between you and your oncology team, weighing disease risk against personal health priorities.
Frequently Asked Questions
Can I switch from tamoxifen to letrozole later?
Yes. Many treatment plans start with tamoxifen for 2-3 years, then transition to an aromatase inhibitor like letrozole for the remaining years. This sequence can improve DFS while limiting early‑stage side effects.
Do I need regular blood tests while on letrozole?
Baseline liver function and lipid panels are recommended, then annually. Letrozole can raise cholesterol, so monitoring helps manage cardiovascular risk.
Is tamoxifen safe during pregnancy?
Tamoxifen is contraindicated in pregnancy because it can cause fetal harm. Effective contraception is required throughout treatment and for a month after stopping.
How quickly do side effects like joint pain appear with letrozole?
Arthralgia often emerges within the first 3-6 months. Early physiotherapy, NSAIDs, or switching to an AI with a different pharmacokinetic profile can help.
What is the typical duration of hormone therapy?
Standard therapy lasts five years. Recent trials show extending to ten years further lowers recurrence for high‑risk patients, but the decision balances benefit against cumulative toxicity.
Bottom line
If you’re postmenopausal and have healthy bones, letrozole usually offers a slight edge in preventing cancer return. If you’re premenopausal, have osteoporosis, or a history of clotting, tamoxifen (or tamoxifen combined with ovarian suppression) remains the safer choice. Talk to your oncologist about your personal risk factors, bone health, and lifestyle preferences-there’s no one‑size‑fits‑all answer.
Andrew Hernandez
October 21, 2025 AT 00:40Many patients find that the choice between letrozole and tamoxifen hinges on bone health and menopausal status. Letrozole reduces estrogen synthesis which can accelerate bone loss while tamoxifen tends to protect bone density. For postmenopausal individuals with stable bone density letrozole often offers a slight advantage in disease‑free survival. If osteoporosis is a concern tamoxifen may be a safer route. Discussing these factors with a healthcare team ensures a personalized plan.
Demetri Huyler
October 30, 2025 AT 05:53Look, as any true American who’s read the latest oncology journals knows, letrozole is the razor‑sharp edge of hormone therapy. It slices estrogen like a hot‑knife through butter, and our labs have shown the numbers speak louder than any European hype. Sure, tamoxifen has its place, especially for the younger crowd, but if you’re post‑menopausal and want the best odds, you grab letrozole and you don’t look back. The US healthcare system even pushes it forward because the data are solid, plain and simple.
Wesley Humble
November 8, 2025 AT 12:06While your enthusiasm is noted, the comparative efficacy data must be contextualized. The BIG 1‑98 trial demonstrated a modest absolute improvement of 2.5 % in disease‑free survival for letrozole over tamoxifen, corresponding to a hazard ratio of 0.81. This translates to a relative risk reduction of 19 % in recurrence, which, while statistically significant, should be weighed against the distinct adverse‑event profiles of each agent. Furthermore, the incidence of arthralgia in letrozole‑treated cohorts approximates 30‑40 %, whereas tamoxifen carries a heightened risk of venous thromboembolism and endometrial pathology. Ultimately, therapeutic selection hinges on patient‑specific comorbidities and preferences. 😊
barnabas jacob
November 17, 2025 AT 18:20Yo, let’s cut the crap – the pharmacodynamics of an AI versus a SERM are worlds apart. Letrozole’s aromatase inhibition triggers a downstream hypo‑estrogenic cascade that can precipitate osteoclastic activity, whereas tamoxifen’s partial agonism muddles the receptor‑signalling matrix. If u got low BMD, u’re basically signing up for a bone‑fracture free‑fall with letrozole. Also, the endometrial hyperplasia risk ain’t a joke; tamoxifen’s agonist effect on uterine tissue is a classic off‑target effect. Bottom line, pick the drug that aligns with your risk‑benefit algorithm, not just the hype.
Rajesh Myadam
November 27, 2025 AT 00:33I hear you on the complexities of the mechanisms you mentioned. It can feel overwhelming when the scientific jargon stacks up, especially when you’re trying to make a personal health decision. Remember that your oncology team can break down these pathways into what matters for your own case. If bone health is a concern, they may recommend a DEXA scan and possibly a bisphosphonate alongside letrozole. Likewise, regular gynecologic monitoring can mitigate tamoxifen‑related uterine risks. Taking one step at a time and keeping open communication can make the process feel more manageable.
Alex Pegg
December 6, 2025 AT 06:46Honestly, the whole hype around one drug being superior feels overblown. While the stats show a slight edge for letrozole in certain trials, real‑world adherence often drops because of joint pain. For many patients, the predictable side‑effect profile of tamoxifen, especially its bone‑preserving qualities, outweighs a marginal recurrence benefit. The decision should be grounded in individual tolerance, not just headline numbers. Also, the US healthcare emphasis on newer agents sometimes discounts long‑standing therapies that have proven safety.
laura wood
December 15, 2025 AT 13:00Your point about adherence is really important. Many people struggle with the arthritic symptoms that can come with aromatase inhibitors, and that can affect their overall treatment success. Keeping an open line with your oncologist about side‑effects allows for adjustments, whether it’s switching medication or adding supportive therapies. It’s also helpful to explore lifestyle measures like gentle exercise and adequate calcium intake to protect bone health regardless of the chosen drug. Ultimately, feeling heard and supported can make a big difference in navigating these choices.
Sebastian Green
December 24, 2025 AT 19:13Bone health really matters when picking between these hormones.
Kate McKay
January 3, 2026 AT 01:26You’ve taken the first brave step by diving into the details of hormone therapy, and that curiosity will serve you well.
Understanding the nuances between letrozole and tamoxifen isn’t just academic; it directly influences your quality of life during treatment.
First, consider your menopausal status – if you’re postmenopausal, letrozole’s ability to slash estrogen production often translates into a modest improvement in disease‑free survival.
On the other hand, tamoxifen works across the menopausal spectrum, making it the default for premenopausal patients.
Second, think about bone health – aromatase inhibitors can accelerate bone loss, so a baseline DEXA scan is a smart move before committing to letrozole.
If your T‑score is already low, discuss adding a bisphosphonate or even switching to tamoxifen, which tends to preserve bone density.
Third, evaluate your cardiovascular and clotting risk; tamoxifen’s estrogenic activity in the liver can raise the chance of venous thromboembolism.
For anyone with a personal or family history of clots, letrozole might be the safer option.
Fourth, be aware of joint pain – many patients report arthralgia within the first few months of letrozole therapy, and that can be a deal‑breaker.
Physical therapy, NSAIDs, or even a temporary switch to tamoxifen can alleviate that discomfort.
Fifth, keep an eye on lipid panels, because letrozole can nudge cholesterol upward, requiring periodic monitoring.
Sixth, remember that treatment duration is typically five years, but extending to ten years has shown additional benefit for high‑risk cases.
Balancing the long‑term benefits against cumulative side effects is a personal decision that should involve your support network.
Don’t hesitate to ask your oncologist about a sequential approach – many clinicians start with tamoxifen for two to three years and then transition to an aromatase inhibitor.
That strategy can capture the early safety of tamoxifen while later leveraging the recurrence‑preventing power of letrozole.
Finally, trust your instincts; you know your body and lifestyle better than anyone else.
If you stay proactive, keep up with follow‑up appointments, and advocate for supportive measures like calcium, vitamin D, and regular exercise, you’ll be positioning yourself for the best possible outcome.
You’ve got this, and the medical community is there to help you navigate each step.
JessicaAnn Sutton
January 12, 2026 AT 07:40Your encouragement, while well‑intentioned, glosses over the critical ethical responsibility of informing patients about the quantitative risk differentials. The absolute benefit of letrozole in disease‑free survival is limited to 2.5 %, a figure that must be juxtaposed against a 30–40 % incidence of arthralgia and a measurable increase in lipid parameters. Moreover, the endometrial safety profile of tamoxifen, albeit not flawless, remains favorable for patients with compromised bone health. It is incumbent upon clinicians to present these statistics without embellishment, ensuring that patients can execute an autonomous, data‑driven choice. Ignoring such nuances constitutes a breach of informed consent.