Drug-Induced Hemolytic Anemia Risk Assessment
Medication Risk Assessment
Check if your current medications may increase your risk of drug-induced hemolytic anemia. This tool helps identify potentially dangerous drugs and associated risk factors.
Risk Assessment Results
When a medication triggers your body to attack its own red blood cells, it’s not just a side effect-it’s a medical emergency. Drug-induced immune hemolytic anemia (DIIHA) happens when your immune system mistakes your red blood cells for invaders and destroys them. These cells normally live for about 120 days. In DIIHA, they’re shredded in days-or even hours. The result? Severe fatigue, shortness of breath, jaundice, and sometimes heart failure. It’s rare, but when it happens, missing the diagnosis can cost lives.
How Medications Trigger Red Blood Cell Destruction
Not all drug-induced hemolysis works the same way. There are two main paths: immune-mediated and oxidative.In immune-mediated DIIHA, the drug sticks to your red blood cells like glue. It doesn’t hurt them on its own-but your immune system sees the drug-cell combo as foreign. It makes antibodies to attack it. These antibodies tag your red blood cells for destruction by the spleen and liver. The most common culprits? Cephalosporin antibiotics, especially cefotetan, ceftriaxone, and piperacillin. Together, these three make up nearly 70% of all immune-mediated cases. Methyldopa was once a big offender, but it’s used far less now because doctors know the risk.
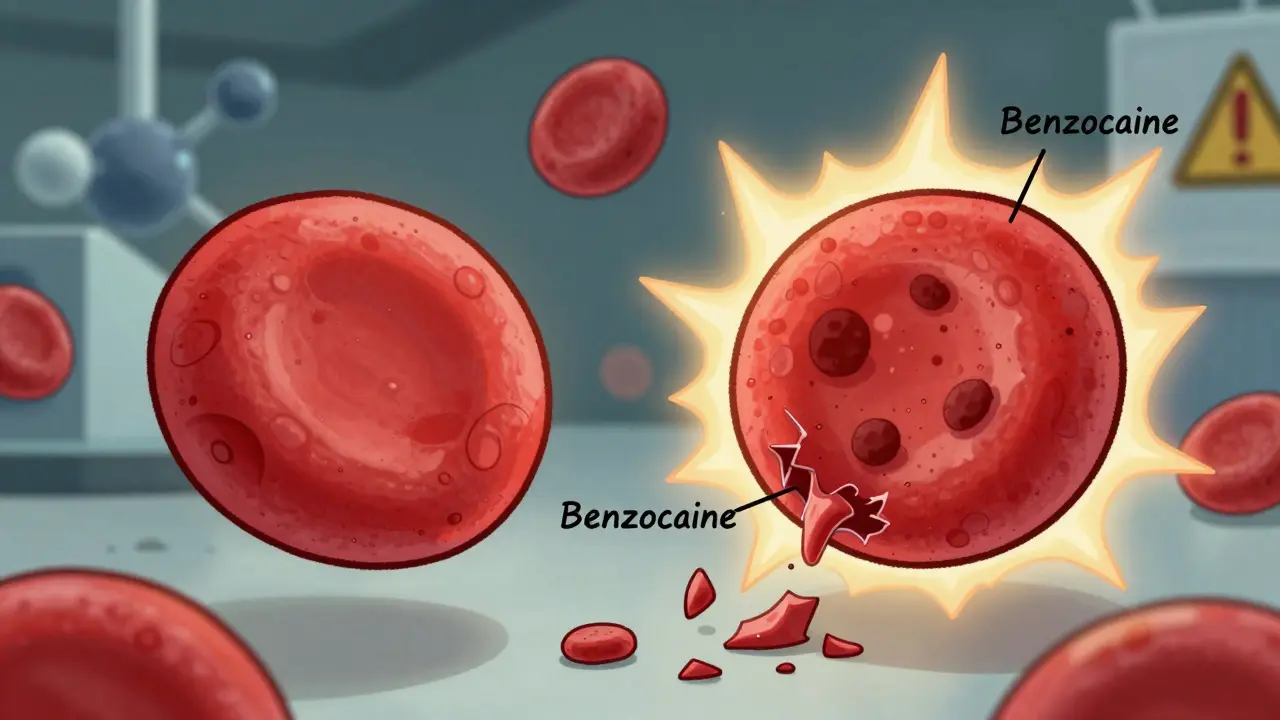
Oxidative hemolysis is different. Here, the drug doesn’t trigger antibodies. Instead, it overwhelms your red blood cells’ natural defenses. Think of it like rusting from the inside. Normally, your cells use an enzyme called G6PD to neutralize harmful oxidants. But if you’re G6PD deficient-which affects up to 14% of African American men and 15% of Mediterranean populations-your cells can’t fight back. Even normal doses of drugs like dapsone, phenazopyridine (Pyridium), or benzocaine can cause these cells to collapse. The damaged hemoglobin forms clumps called Heinz bodies, which rip the cell apart.
And here’s the catch: even if you don’t know you have G6PD deficiency, a single dose of a risky drug can trigger a crisis. That’s why it’s not just about known allergies-it’s about hidden vulnerabilities.
Which Drugs Are Most Likely to Cause This?
The list of drugs linked to hemolytic anemia is longer than most people realize. But not all are equal in risk.For immune-mediated DIIHA, the top offenders are clear:
- Cefotetan
- Ceftriaxone
- Piperacillin
- Penicillin and related antibiotics
- Methyldopa (historically significant, now rare)
- NSAIDs like ibuprofen or naproxen (less common, but documented)
For oxidative hemolysis, the triggers include:
- Dapsone
- Phenazopyridine (Pyridium)
- Primaquine
- Sulfa drugs
- Ribavirin
- Amyl nitrate and butyl nitrate (sometimes used recreationally)
- Topical benzocaine (in sprays or gels for sore throats or teething)
It’s not just about the drug name-it’s about the dose, duration, and your genetics. Someone with normal G6PD can take dapsone for months without issue. Someone with the deficiency can crash after one tablet. That’s why knowing your history matters.
What Symptoms Should You Watch For?
The signs of hemolytic anemia aren’t always obvious at first. They mimic other common problems-flu, exhaustion, stress. But when they show up together, they’re a red flag.Here’s what most patients experience:
- Fatigue (92% of cases)
- Weakness (87%)
- Shortness of breath (76%)
- Rapid heartbeat (tachycardia over 100 bpm in 68%)
- Pale skin or mucous membranes (73%)
- Yellowing of the skin or whites of the eyes (jaundice in 81%)
- Dark urine (from hemoglobin breakdown)
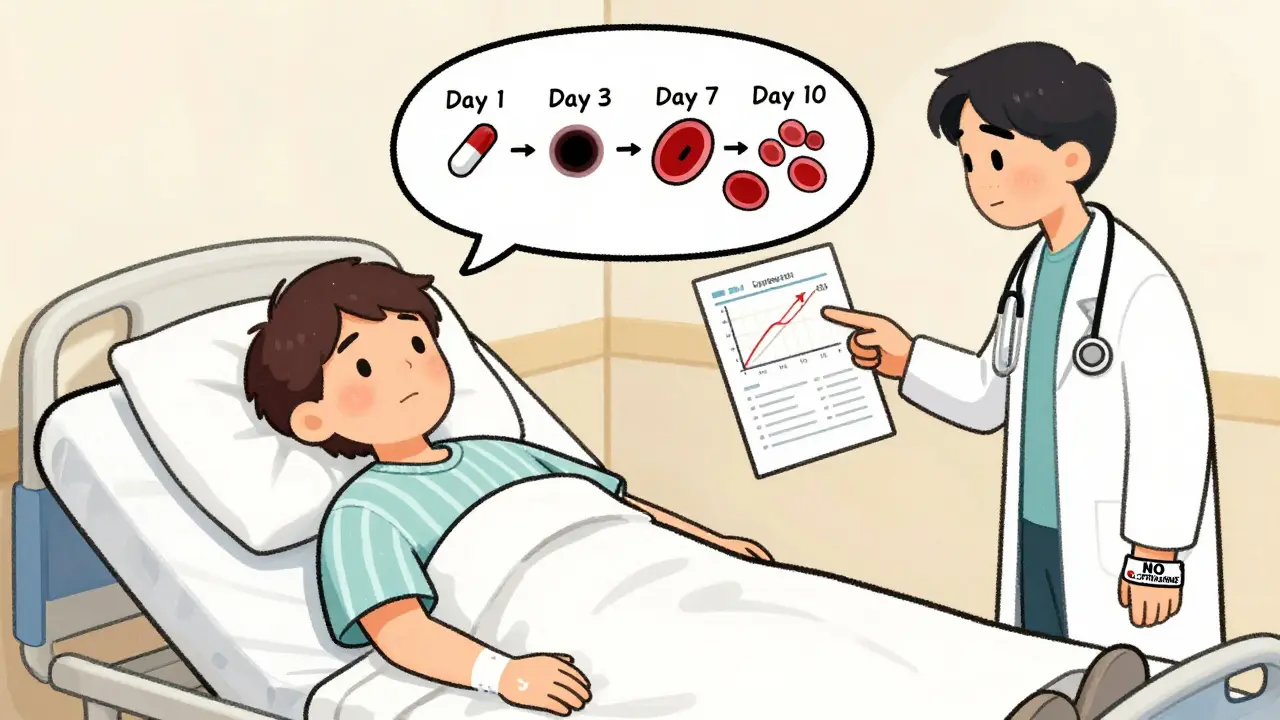
These symptoms don’t appear immediately. Immune-mediated DIIHA usually shows up after 7 to 10 days of taking the drug. Oxidative hemolysis can hit within 24 to 72 hours-especially in G6PD-deficient people. That’s why timing matters. If you started a new antibiotic last week and suddenly feel awful, it’s not just a bad reaction-it could be your blood cells being destroyed.
Severe cases can drop hemoglobin by 3 to 5 grams per deciliter in just 48 hours. That’s like losing a full liter of blood overnight. And when hemoglobin falls below 6 g/dL, the heart starts struggling. Studies show 8% of these patients develop heart failure. Another 15% show signs of cardiomyopathy. It’s not theoretical-it’s measurable, and it’s dangerous.
How Doctors Diagnose It
There’s no single test. Diagnosis is a puzzle made of symptoms, history, and lab results.First, your doctor checks for signs of hemolysis:
- Elevated indirect bilirubin (above 3 mg/dL)
- High lactate dehydrogenase (LDH above 250 U/L)
- Low haptoglobin (below 25 mg/dL)
These markers mean red blood cells are breaking down faster than your body can replace them. Then comes the peripheral blood smear. If you see spherocytes (small, round red cells without the normal dip), it points to immune destruction. If you see Heinz bodies (dark clumps inside red cells), it’s oxidative damage.
The gold standard for immune-mediated cases? The direct antiglobulin test (DAT). It finds antibodies stuck to your red blood cells. It’s positive in 95% of immune DIIHA cases-but not always. Early on, or with certain drugs, it can be negative. That’s why doctors can’t rely on it alone.
If G6PD deficiency is suspected, testing is essential. But here’s the trap: during active hemolysis, the test can give false negatives. Why? Because the test measures enzyme levels in older red blood cells-and those are the ones being destroyed. The new ones, still healthy, aren’t counted yet. That’s why experts recommend waiting 2 to 3 months after the episode to test accurately.
What Happens After Diagnosis?
The first and most critical step? Stop the drug. Immediately. No exceptions. No waiting. No “maybe it’s something else.”Once the drug is out of your system, your bone marrow starts making new red blood cells. In most cases, hemoglobin levels begin to rise within 7 to 10 days. Full recovery usually takes 4 to 6 weeks.
But not everyone recovers on their own. If your hemoglobin drops below 7-8 g/dL, or you’re dizzy, short of breath, or have chest pain, you’ll need a blood transfusion. It’s not optional-it’s life-saving.
Some patients get corticosteroids like prednisone. But here’s the truth: their benefit is unclear. Many people improve just by stopping the drug. Steroids carry risks-weight gain, mood swings, high blood sugar-and aren’t always worth it.
For the 10-15% of cases where antibodies keep attacking even after the drug is gone, things get more complex. These are called drug-independent autoantibodies. Treatment then moves to:
- Intravenous immunoglobulin (IVIG) at 1 g/kg per day for two days
- Rituximab (375 mg/m² weekly for four weeks)
- Azathioprine or cyclosporine for long-term suppression
Recent data shows 78% of these stubborn cases respond within 3 to 6 weeks. And new drugs are coming. In 2024, early trials showed efgartigimod-a drug that clears antibodies from the blood-helped 67% of patients within four weeks.
The Hidden Danger: Methylene Blue and G6PD Deficiency
If you develop methemoglobinemia-where hemoglobin can’t carry oxygen properly-doctors might reach for methylene blue. It’s a lifesaver… unless you’re G6PD deficient.Methylene blue itself is an oxidant. In someone with low G6PD, it doesn’t fix the problem-it makes it worse. It can trigger a massive, deadly hemolytic crisis. That’s why it’s absolutely contraindicated in these patients. If you’re being treated for methemoglobinemia and your doctor orders methylene blue, ask: “Do I have G6PD deficiency?” If you don’t know, don’t take it.
Alternative treatments exist-ascorbic acid (vitamin C), exchange transfusion, or hyperbaric oxygen. But they’re not as fast. That’s why knowing your G6PD status matters before any treatment begins.
Why This Is So Often Missed
Doctors aren’t careless. But DIIHA is rare-and sneaky.A 2024 study found 43% of cases were misdiagnosed at first. Patients were told they had the flu, an infection, or liver disease. One patient was sent home with antibiotics for “possible pneumonia” while her red blood cells were being destroyed. She didn’t improve. She returned days later, pale and gasping. Only then did someone connect the dots.
Internal medicine residents correctly identified DIIHA in only 58% of cases on their first try. After targeted training on drug lists and lab patterns, that jumped to 89%. That’s not a failure of skill-it’s a failure of awareness.
Hospitals that added alerts to their electronic systems-flagging high-risk drugs like ceftriaxone or dapsone in patients with unexplained anemia-saw a 32% drop in severe cases over 18 months. Technology helps. But so does thinking differently. When you see anemia, don’t just ask: “What’s causing low iron?” Ask: “What did this person start taking recently?”
What You Can Do
If you’re on any of these medications and feel unusually tired, short of breath, or notice your skin turning yellow:- Stop the drug immediately and contact your doctor.
- Don’t wait for it to get worse.
- Ask for a blood test: CBC, LDH, haptoglobin, bilirubin, and a peripheral smear.
- If you’re of African, Mediterranean, or Southeast Asian descent, ask about G6PD testing-even if you’ve never had symptoms before.
- Keep a list of all medications you’ve taken in the past 30 days, including over-the-counter and topical products.
There’s no vaccine for this. No pill to prevent it. But awareness saves lives. The drugs that cause this are common. The reaction is rare. But when it happens, speed is everything.
Can a single dose of a drug cause hemolytic anemia?
Yes, especially in people with G6PD deficiency. Oxidative hemolysis can begin within 24 to 72 hours after taking drugs like dapsone, phenazopyridine, or benzocaine. Immune-mediated cases usually take longer-7 to 10 days-but even a single dose can start the process if the immune system has been sensitized by prior exposure.
Is hemolytic anemia from drugs permanent?
No. In over 95% of cases, stopping the drug leads to full recovery within 4 to 6 weeks. The body replaces destroyed red blood cells naturally. The only exception is if the immune system develops persistent autoantibodies-this happens in a small fraction of cases and may require longer-term treatment.
Can children get drug-induced hemolytic anemia?
It’s rare in children, but it does happen. When it does, children often present with more severe anemia than adults-average hemoglobin levels can drop to 5.2 g/dL. Because symptoms like fatigue and pale skin are common in kids, it’s often missed. Any unexplained anemia in a child who recently took antibiotics or pain relievers should raise suspicion.
Should I get tested for G6PD deficiency if I’ve never had symptoms?
If you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent, yes. G6PD deficiency is inherited and often silent until triggered. Many people live their whole lives without knowing they have it-until they take a drug like dapsone or sulfamethoxazole and have a sudden, severe reaction. Testing is simple and can prevent a life-threatening event.
Are herbal supplements or vitamins safe if I’m at risk?
Not necessarily. Some herbal products, like naphthalene (found in mothballs or certain traditional remedies), can trigger oxidative hemolysis. High-dose vitamin C (ascorbic acid) can help in methemoglobinemia but may worsen oxidative stress in rare cases. Always tell your doctor about every supplement you take-even if you think it’s “natural.”
Can I ever take the drug again if I had DIIHA once?
No. Re-exposure to the same drug-even years later-can cause an even faster and more severe reaction. Once you’ve had drug-induced hemolytic anemia, that drug is permanently off-limits. Make sure your medical records and pharmacy profile are updated, and wear a medical alert bracelet if you’ve had a severe reaction.
Akshaya Gandra _ Student - EastCaryMS
January 4, 2026 AT 19:28i just started taking ibuprofen for my headache and now i feel kinda tired… is this normal? i’m from india and we use these all the time
Ashley Viñas
January 5, 2026 AT 17:20Oh sweet mercy. Another person who thinks OTC meds are harmless. You know what’s scarier than DIIHA? People who don’t even know what G6PD is and still pop pills like candy. You’re lucky you didn’t end up in the ICU.
And yes, that fatigue? It’s not ‘normal.’ It’s your red blood cells screaming for help. Stop the ibuprofen. Get a CBC. Now.
Joseph Snow
January 6, 2026 AT 14:35Let me guess-this is another Big Pharma fear-mongering piece. Who funded this? The blood transfusion industry? The lab testing conglomerates? The fact that you listed NSAIDs as ‘common culprits’ is statistically absurd. Hemolysis from ibuprofen? Please. There are more deaths from apple seeds than from drug-induced hemolytic anemia. This is fear porn disguised as medicine.
melissa cucic
January 7, 2026 AT 12:16Thank you for this meticulously detailed, clinically grounded exposition. I particularly appreciate how you distinguished between immune-mediated and oxidative pathways-so often conflated in lay literature.
It’s worth emphasizing, too, that the DAT’s false-negative potential in early-phase DIIHA is not merely a technical footnote; it’s a diagnostic blind spot with life-or-death consequences. And the G6PD testing timing caveat? Absolutely critical. So many clinicians rush to test during acute hemolysis, then wrongly reassure patients based on a misleadingly ‘normal’ result.
Knowledge, as you’ve shown, is the only true prophylaxis.
Angie Rehe
January 8, 2026 AT 13:20Why are we still using outdated terms like ‘immune-mediated’? It’s not immune-mediated-it’s hapten-driven antibody production. And you didn’t even mention the role of complement activation via the classical pathway in ceftriaxone cases. Also, phenazopyridine isn’t just for UTIs-it’s in half the OTC ‘bladder relief’ blends. That’s a hidden exposure vector.
And where’s the data on drug-drug interactions? Like when someone takes dapsone + sulfamethoxazole + NSAIDs? Synergistic oxidative stress. You’re leaving out the pharmacokinetic synergy. This is surface-level.
Enrique González
January 8, 2026 AT 19:35This is the kind of info every single person on meds needs to know. Seriously. Stop scrolling. Read this. Save it. Share it.
If you’ve ever taken an antibiotic and then felt like you got hit by a truck a week later? That wasn’t ‘just a bug.’ That could’ve been your blood dying.
Don’t wait for jaundice. Don’t wait for dizziness. If you feel off after starting a new drug-stop it. Call your doctor. Don’t be the person who says ‘I thought it was just tiredness.’
Aaron Mercado
January 9, 2026 AT 05:29They don’t want you to know this. They don’t want you to know that your ‘safe’ antibiotics are slowly killing you. Ceftriaxone? Used in EVERY hospital. Every. Single. One. And they don’t test you for G6PD before giving it? Why? Because it’s cheaper to treat the anemia than prevent it.
And methylene blue? That’s not a treatment-it’s a death sentence for millions who don’t know their blood type. The CDC knows. The FDA knows. But they keep pushing these drugs. Who profits? Hospitals. Labs. Pharma. You? You’re just a statistic.
Wake up.
Shanna Sung
January 9, 2026 AT 18:50Stop taking meds
josh plum
January 11, 2026 AT 04:32People like you think you’re helping, but you’re just feeding the fear machine. DIIHA is rarer than getting struck by lightning. You’re scaring people away from life-saving antibiotics because you want to feel like a medical expert.
And G6PD testing for everyone? That’s not medicine-that’s a bureaucratic nightmare. We don’t test for every genetic quirk before prescribing Tylenol. Do you want to test everyone for sickle cell before giving them a flu shot too?
This isn’t prevention. It’s paranoia dressed in white coats.
John Ross
January 12, 2026 AT 23:36As someone who’s worked in Lagos with limited diagnostics, I’ve seen this play out. A child on amoxicillin turns jaundiced. No labs. No DAT. No G6PD test. Just a mother crying, wondering why her boy’s skin turned yellow.
We stopped the drug. Gave fluids. Watched. And in 12 days-he was fine.
This isn’t just a Western problem. It’s a global one. And in places without labs, awareness is the only tool we have. This post? It’s a lifeline.
Clint Moser
January 13, 2026 AT 05:23Did you know the FDA quietly changed the labeling on ceftriaxone in 2022 to include a ‘black box’ warning for hemolysis? No? Because they buried it in the 800-page PDF no one reads. And now they’re rolling out AI systems that flag high-risk combos… but only in 12 states.
Meanwhile, Walmart pharmacies still sell benzocaine teething gel with no warning. And you think this is about ‘awareness’? No. It’s about profit margins.
They don’t care if you live. They care if you keep buying pills.
Mandy Kowitz
January 14, 2026 AT 22:36Wow. So the solution to every medical problem is ‘stop taking everything.’
Next you’ll tell me aspirin gives you internal bleeding and water causes drowning. I’m just glad I don’t live in a world where every drug is a potential death sentence.
Also, I’ve taken ceftriaxone twice. Still here. Still typing. Still not dead. Thanks for the fear.
bob bob
January 16, 2026 AT 10:35Thank you for writing this. I had no idea any of this was possible. I’ve been on dapsone for years for a skin condition and never thought twice.
Just got my G6PD test done yesterday-turns out I’m deficient. I’m so glad I read this before something bad happened.
I’m switching meds with my doctor next week. I’ll be honest-I was scared to even ask about testing. Now I’m just grateful.
Oluwapelumi Yakubu
January 17, 2026 AT 14:53Ah, the modern human-so afraid of pills that they forget the body is a temple, not a machine.
But tell me this: if the blood remembers betrayal, then why do we still trust the same hands that gave us the poison? The drug is not the villain-it is the mirror. It reflects our haste, our ignorance, our surrender to convenience.
When you take a pill, you are not healing-you are negotiating with chaos. And chaos, my friend, has no mercy.
Perhaps the real question is not ‘which drug?’ but ‘why do we keep reaching for them?’