When your blood pressure stays too high, doctors don’t just tell you to eat less salt or walk more. They reach for a pill. And for millions of people, that pill is one of three classes: beta-blockers, ACE inhibitors, or ARBs. These aren’t just random drugs - they’re the backbone of hypertension treatment. But here’s the thing: not all of them work the same way, and not all of them are safe for everyone. Some cause a dry cough so bad you can’t sleep. Others make you feel like you’re dragging through molasses. And a few? They could save your life after a heart attack.
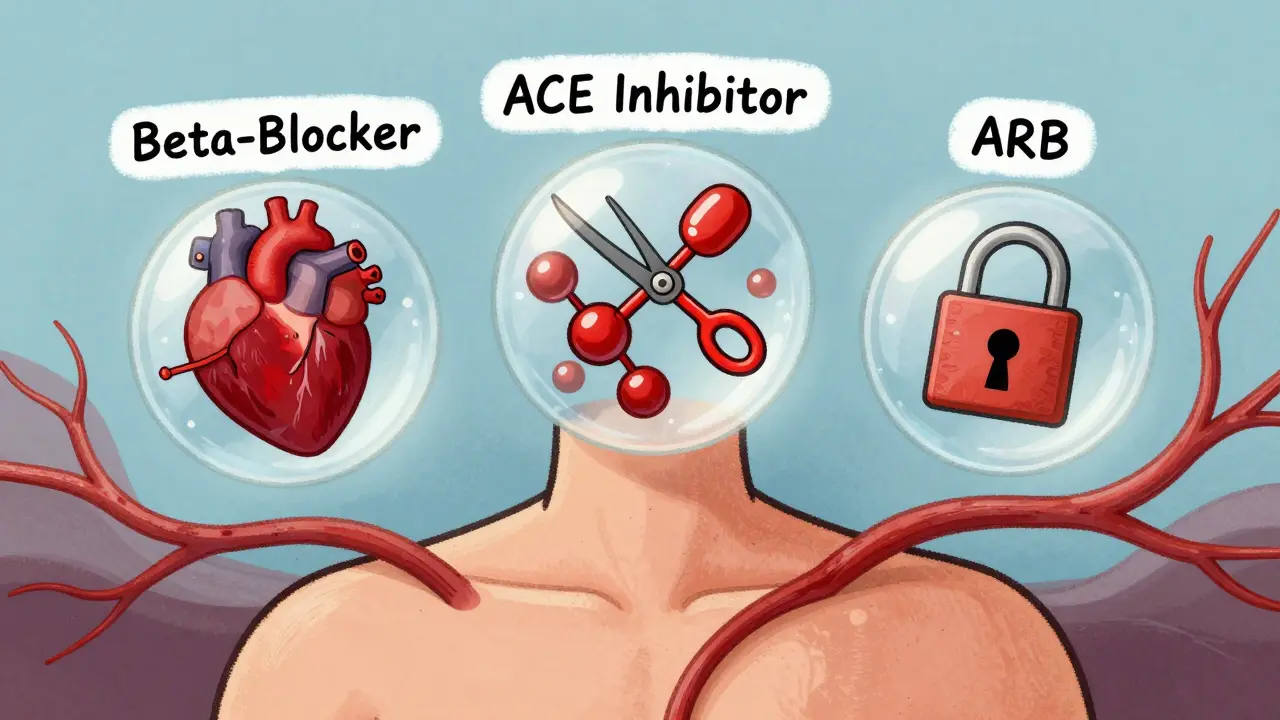
How These Drugs Actually Work (No Jargon)
Your body has a system called the renin-angiotensin system. It’s like a pressure regulator. When your blood pressure drops too low, it kicks in to raise it. But in people with high blood pressure, this system is stuck on “high.”
ACE inhibitors - like lisinopril, enalapril, and ramipril - block an enzyme called angiotensin-converting enzyme. That stops your body from making angiotensin II, a chemical that tightens blood vessels. Less angiotensin II = looser vessels = lower pressure. Simple.
ARBs - losartan, valsartan, candesartan - do something similar but smarter. Instead of blocking the enzyme, they block the receptor that angiotensin II uses to tighten blood vessels. It’s like cutting the signal to the lock instead of breaking the keymaker. No angiotensin II can get through, so your vessels stay relaxed.
Beta-blockers - metoprolol, carvedilol, bisoprolol - work differently. They don’t touch the blood vessels. They slow your heart. By blocking beta receptors, they reduce how hard and how fast your heart pumps. That lowers pressure, yes, but it also drains your energy. That’s why people on beta-blockers often say they feel tired, sluggish, or even depressed.
The Cough That Won’t Go Away
If you’ve ever taken lisinopril and started coughing - a dry, scratchy, nighttime cough that doesn’t respond to cough syrup - you’re not alone. About 1 in 5 people on ACE inhibitors get it. It’s not an allergy. It’s a side effect of bradykinin, a chemical that builds up when ACE is blocked. Bradykinin irritates your throat. It’s harmless, but it’s unbearable.
That’s why ARBs became so popular. They don’t cause bradykinin buildup. So no cough. In a 2021 study of over 300,000 patients, people on ARBs were 38% less likely to develop a cough than those on ACE inhibitors. And angioedema - a rare but dangerous swelling of the face or throat - happens less often too.
Real people say it best. On Reddit, one user wrote: “Switched from lisinopril to valsartan after six months of coughing so hard I peed myself. Within two days, it was gone. I felt like I could breathe again.” That’s not an outlier. CVS Health found that 78% of people who quit ACE inhibitors did so because of cough.
Which One Is Best for Your Heart?
Not all high blood pressure is the same. If you’ve had a heart attack, ACE inhibitors are still the gold standard. The SAVE trial in 1992 showed they cut death risk by 19% after a heart attack. The HOPE trial in 2000 showed a 20-25% drop in major heart events. That’s not small. That’s life-changing.
But if you have heart failure with reduced pumping power (HFrEF), things changed in 2014. The PARADIGM-HF trial compared enalapril (an ACE inhibitor) to sacubitril-valsartan (a new combo drug that includes an ARB). The ARB combo didn’t just match it - it beat it. It cut heart failure deaths by 20% and overall deaths by 16%. Now, guidelines say if you qualify, you start with the combo, not the ACE inhibitor.
Beta-blockers? They’re not for everyone with high blood pressure. If you’re young, healthy, and just have high numbers, beta-blockers aren’t the best pick. The INVEST trial showed atenolol led to 16% more strokes than other drugs. But if you have heart failure or you’ve had a heart attack? Carvedilol and bisoprolol can slash your death risk by 30-35%. The difference isn’t just in the drug - it’s in the class. Carvedilol isn’t the same as atenolol.

The Hidden Trade-Offs
Every drug has a price. For ACE inhibitors, it’s the cough. For ARBs, it’s cost - they’re often more expensive than generic lisinopril. But the real cost comes in what they don’t do.
Beta-blockers mess with your metabolism. They can raise triglycerides by 10-15% and drop your “good” HDL cholesterol by 5-10%. That’s bad news if you’re already prediabetic or overweight. They also make you tired. One study found 28% of patients on metoprolol felt too exhausted to work. Switching to nebivolol - a newer beta-blocker - cut that to 14%.
And here’s something most people don’t know: combining an ACE inhibitor with an ARB sounds like a good idea - double the power, right? Wrong. The ONTARGET trial showed it increased kidney failure risk by 38%. That’s not better. That’s dangerous. No doctor should ever prescribe both together for routine high blood pressure.
Who Gets Which Drug - And Why
Doctors don’t just pick a drug at random. They match it to your body.
- Diabetic kidney disease? ACE inhibitors win. The RENAAL trial showed they reduce protein in urine 21% better than ARBs. That’s critical for protecting your kidneys.
- Older adults with high blood pressure? ARBs are gaining ground. A 2021 study found ARBs linked to slower cognitive decline. That’s huge for brain health.
- Post-heart attack? ACE inhibitors still lead. Even with newer drugs, the evidence for ACE inhibitors here is rock-solid.
- Heart failure? Sacubitril-valsartan is now first-choice if you qualify. If not, ACE inhibitors or ARBs work fine.
- Just high blood pressure with no other issues? ARBs or calcium channel blockers (like amlodipine) are better than beta-blockers. Beta-blockers don’t protect your brain as well.
Primary care doctors still prescribe ACE inhibitors as first-line in 58% of cases. But cardiologists? They’re already switching. In 2022, 68% of cardiologists said they’d start a new patient on an ARB instead of an ACE inhibitor - just to avoid the cough.
What Patients Actually Experience
Numbers tell part of the story. Real people tell the rest.
On Drugs.com, lisinopril has a 5.8 out of 10 rating. 42% of users report cough. 8% quit because of side effects. Losartan? 7.1 out of 10. Only 15% report problems. That’s not a small gap. That’s a life difference.
One man in Toronto wrote: “I was on lisinopril for two years. I couldn’t talk on the phone without coughing. My wife said I sounded like a dying cat. Switched to valsartan. No cough. No fatigue. I feel like myself again.”
Another: “Metoprolol made me so tired I couldn’t play with my kids. I thought I was getting old. Turns out, it was the beta-blocker. Switched to amlodipine. Energy came back in a week.”
These aren’t rare stories. They’re common. And they’re why adherence matters. CVS Health found that 63% of people stayed on ARBs after a year. Only 57% stayed on ACE inhibitors. The reason? Cough. Simple as that.
Dosing and Starting Out
You don’t start high. You start low and go slow.
- ACE inhibitor: Lisinopril 10 mg once daily. Max dose: 40 mg.
- ARB: Losartan 50 mg once daily. Max dose: 100 mg.
- Beta-blocker: Metoprolol succinate 25-50 mg once daily. Max dose: 200 mg.
If you have heart failure, the rules change. Carvedilol starts at 3.125 mg twice a day. You double the dose every two weeks. It takes 12-16 weeks to reach the target. Rushing it can make you worse.
And never, ever stop these drugs cold turkey. Especially beta-blockers. Stopping suddenly can trigger a heart attack. Always talk to your doctor first.
What’s Changing in 2025?
The game is shifting. The FDA approved a new four-drug combo in 2023 for tough-to-treat high blood pressure. It includes valsartan (an ARB), which shows how much ARBs are taking over.
The PRECISION trial, ending in 2025, is comparing ARBs and ACE inhibitors in people over 65. If ARBs prove better for brain health, guidelines will change again.
And the market? ARBs are growing faster than ACE inhibitors. By 2028, they’ll be the most prescribed renin-angiotensin drug for high blood pressure. Not because they’re stronger - but because they’re easier to live with.
But here’s the bottom line: ACE inhibitors still save lives after heart attacks. Beta-blockers still prevent death in heart failure. ARBs are the better choice for most people starting out - if you want to avoid the cough and still protect your heart and kidneys.
There’s no single best drug. There’s the best drug for you.
Joe Kwon
December 29, 2025 AT 15:38ACE inhibitors block the conversion of angiotensin I to II via ACE enzyme inhibition-classic RAAS modulation. ARBs are receptor antagonists, so they preserve the enzymatic pathway but prevent ligand binding. Beta-blockers? They’re adrenergic antagonists, reducing cardiac output and renin release. All three lower BP, but the downstream effects on bradykinin, aldosterone, and sympathetic tone vary significantly. That’s why monotherapy selection isn’t one-size-fits-all.
Nicole K.
December 30, 2025 AT 07:28Why do people keep taking these drugs if they make you feel like garbage? Just eat less salt and move your body. It’s not rocket science.
Fabian Riewe
December 30, 2025 AT 19:21Love this breakdown. I was on lisinopril for 3 years and the cough was brutal-like a chainsaw in my throat at 3 a.m. Switched to losartan and it was like someone turned off a loud alarm. No more cough, no more fatigue. Honestly? ARBs are the way to go unless you’ve got diabetic kidney disease. Then yeah, ACEs still win.
Emma Duquemin
December 31, 2025 AT 06:02OMG YES. I was on metoprolol and felt like a zombie. Couldn’t even jog with my dog anymore. Thought I was just getting old. Turns out my heart was beating like a turtle and my brain was on mute. Switched to amlodipine and suddenly I was dancing in the kitchen again. 💃🕺 Life-changing. Why do docs still push beta-blockers for *everyone*?!
Duncan Careless
January 1, 2026 AT 18:52Interesting stuff. I’m not a doctor, but I’ve seen a few patients go through this. The cough thing is real. I’d say if someone’s got a dry cough after starting an ACE, don’t wait three months-switch early. Better to lose a few bucks on an ARB than lose sleep for half a year.
Amy Cannon
January 3, 2026 AT 02:26It is truly fascinating how pharmaceutical innovation continues to refine therapeutic strategies in cardiovascular medicine. The transition from ACE inhibitors to ARBs as first-line agents for non-diabetic hypertensive patients reflects a paradigm shift toward patient-centered care, prioritizing tolerability and long-term adherence. Moreover, the emergence of sacubitril-valsartan as a superior alternative in HFrEF underscores the importance of evidence-based, trial-driven guideline evolution. One must not overlook the sociocultural implications of medication adherence, as evidenced by CVS Health data indicating higher persistence rates with ARBs-likely attributable to diminished adverse effect burden.
Kevin Lopez
January 4, 2026 AT 20:16Beta-blockers are outdated for HTN. INVEST proved it. Stick to CCBs or ARBs. End of story.
Jasmine Yule
January 5, 2026 AT 15:58Kevin, you’re right-but you’re also being rude. People need options. Not everyone can afford brand-name ARBs. And some of us have kidney issues where ACEs are still the only safe choice. Let’s not throw the baby out with the bathwater. 💙
Samar Khan
January 6, 2026 AT 04:10Why do you all act like this is some deep secret? My aunt died because her doctor kept her on lisinopril even after she started coughing up blood. 🤡 No one listens. Just push pills. Everyone’s so obsessed with ‘guidelines’ they forget people are dying. #medicalnegligence
Himanshu Singh
January 7, 2026 AT 00:51Hey i read this and i was on bisoprolol for 2 year. Tired all the time. Switched to valsartan and now i can play with my kids again. No more naps after dinner. 😊
Russell Thomas
January 7, 2026 AT 14:07Wow, so the real reason ARBs are replacing ACE inhibitors isn’t because they’re better-it’s because people can’t handle a little cough. We’re raising a generation that can’t tolerate side effects. Next they’ll ban aspirin because it gives you a stomach ache.
Greg Quinn
January 8, 2026 AT 07:00It’s funny how we treat medicine like a menu. ‘I’ll have the ARB, no cough, please.’ But hypertension isn’t about comfort-it’s about survival. ACE inhibitors reduce mortality post-MI. ARBs are nice, but they’re not magic. We’re trading convenience for evidence. And if we keep doing that, we’ll end up with a population that feels fine but dies younger. There’s a difference between tolerable and optimal.