Medication Allergy Severity Calculator
Determine the severity of a medication allergy reaction using evidence-based criteria from medical guidelines.
Enter values to calculate severity
When you take a pill, you don’t expect your immune system to go on a warpath. Yet for millions of people a drug can trigger a full‑blown allergy, ranging from a harmless rash to a life‑threatening collapse. Knowing whether a reaction is mild, moderate, or severe isn’t just academic-it decides if you need a quick antihistamine, emergency epinephrine, or a stay in a burn unit.
Key Takeaways
- Medication allergies affect 7‑10% of the population; about 5‑10% of those are severe.
- Mild reactions stay localized (e.g., small hives), moderate spread systemically but keep vital signs stable, and severe reactions involve airway, cardiovascular or multi‑organ compromise.
- Immediate identification uses the Gell‑Coombs types (I‑IV) plus the newer mixed‑mechanism Type VII category.
- Treatment escalates from antihistamines → corticosteroids → epinephrine + specialist care.
- Genetic screening (e.g., HLA‑B*15:02) and standardized severity calculators now cut severe reaction rates dramatically.
What Is a Medication Allergy?
Medication allergy is an abnormal immune response to a pharmaceutical substance that mistakenly flags the drug as harmful. This misrecognition triggers a cascade of antibodies or T‑cells, leading to symptoms that can appear minutes or weeks after exposure. According to the European Academy of Allergy and Clinical Immunology (EAACI) 2021 report, true immunologically mediated drug allergies make up 10‑15% of all adverse drug reactions, the rest being non‑immune side effects.
Gell‑Coombs Classification: The Immunology Behind the Reaction
The classic Gell‑Coombs system still guides clinicians:
- Type I hypersensitivity (IgE‑mediated) - rapid, within minutes, mast cell degranulation.
- Type II hypersensitivity (IgG/IgM cytotoxic) - targets blood cells, can cause hemolysis or thrombocytopenia.
- Type III hypersensitivity (immune‑complex) - forms circulating complexes, leading to serum sickness or glomerulonephritis.
- Type IV hypersensitivity (T‑cell mediated) - delayed, 48‑72 h, manifests as maculopapular rash, Stevens‑Johnson Syndrome (SJS) or toxic epidermal necrolysis (TEN).
In 2024 the EAACI task force added a provisional Type VII mixed‑mechanism category for reactions that show both IgE and T‑cell features, accounting for roughly 15‑20% of severe cases.
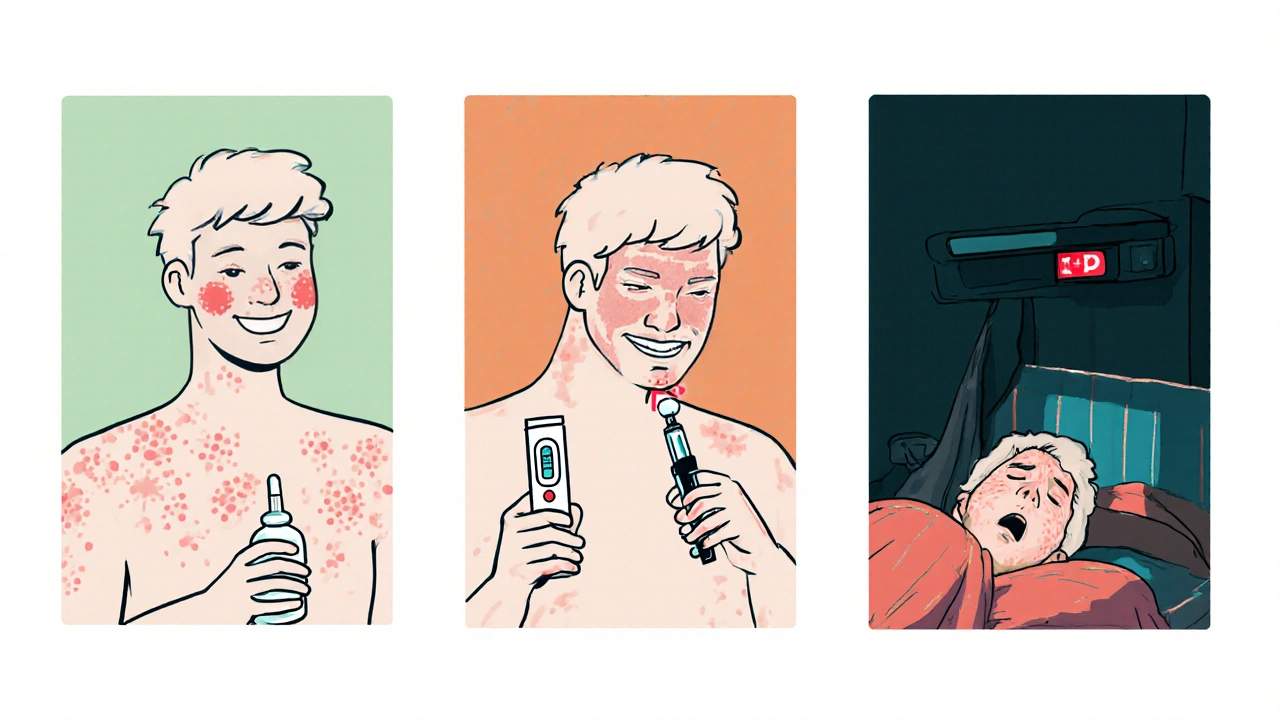
How Mild, Moderate, and Severe Reactions Differ
Severity isn’t just a matter of size; it’s about which organ systems are involved and how quickly they collapse.
Mild Reactions
Typical signs:
- Localized urticaria covering <10% of body surface area.
- Itchy, non‑progressive rash or “red man syndrome” from rapid vancomycin infusion.
- Serum histamine usually 2‑5 ng/mL (if measured).
Management is usually a single dose of a non‑sedating antihistamine (e.g., cetirizine 10 mg) and drug discontinuation. Symptoms resolve within 24‑48 hours in >90% of cases (DynaMed 2023).
Moderate Reactions
These cross the threshold from skin‑only to systemic involvement but still hold vital signs steady.
- Urticaria 10‑30% body surface area, possibly with facial angio‑edema.
- Fever 38‑39 °C, mild tachycardia, or transient hypotension (systolic 90‑100 mmHg).
- Histamine 5‑10 ng/mL, eosinophil count modestly elevated.
Recommended care: stop the offending drug, give oral corticosteroids (prednisone 0.5 mg/kg), and observe for 4‑6 hours in a monitored setting. About 75% settle within 72 hours (Langford Allergy 2024).
Severe Reactions
Life‑threatening patterns demand immediate emergency action.
- Anaphylaxis: sudden hypotension (systolic <90 mmHg), bronchospasm (FEV1 ↓ > 25%), SpO₂ <90%.
- Stevens‑Johnson Syndrome or Toxic epidermal necrolysis: <10% or >30% epidermal detachment, respectively, with mortality 5‑35%.
- Drug reaction with eosinophilia and systemic symptoms (DRESS): fever, facial edema, organ involvement (liver, kidneys), eosinophils >1,500 µL.
First‑line treatment is intramuscular epinephrine 0.3‑0.5 mg (1 mg/mL) for adults, rapid airway support, and immediate transfer to an emergency department or specialized burn unit (EAACI 2023). Mortality for anaphylaxis sits around 0.001‑0.015%, but delayed recognition pushes it higher, especially for SJS/TEN.
Quick Reference: Severity Comparison Table
| Feature | Mild | Moderate | Severe |
|---|---|---|---|
| Onset | Seconds‑minutes (IgE) or days (delayed) | Minutes‑hours (IgE) or 2‑3 days (delayed) | Immediate (anaphylaxis) or 7‑14 days (SJS/TEN) |
| Skin involvement | Local hives <10% BSA | Widespread hives 10‑30% BSA, possible angio‑edema | SJS/TEN >30% BSA, full‑thickness skin loss |
| Systemic signs | None or mild pruritus | Fever, mild hypotension, tachycardia | Hypotension, bronchospasm, organ failure |
| Lab markers | Histamine 2‑5 ng/mL | Histamine 5‑10 ng/mL, modest eosinophilia | Histamine >10 ng/mL, eosinophils >1,500 µL, elevated creatinine/LFTs |
| First‑line treatment | Antihistamine | Antihistamine + corticosteroid, observe | Epinephrine, airway management, ICU/burn unit |
| Typical outcome | Full resolution <48 h | Resolution 2‑5 days with therapy | Survival 70‑95% with rapid care; high morbidity |
Recognizing Severity at the Bedside
Even seasoned clinicians miss severe reactions about 20% of the time. A quick mental checklist helps:
- Ask: Is there airway compromise? Look for stridor, voice changes, or swelling.
- Check blood pressure and heart rate - a systolic below 90 mmHg flags severe.
- Assess skin: Measure body‑surface‑area involvement; >30% = TEN level.
- Order rapid labs: serum tryptase for anaphylaxis, creatinine/LFTs for DRESS.
- Document exact timing and dose - this drives later testing.
Using the American College of Allergy’s online severity calculator (12 parameters, score >50 = severe) standardizes the decision.
Diagnostic Tools: From Skin Testing to Genetic Screening
Choosing the right test hinges on the reaction type.
- Skin testing (prick or intradermal) detects IgE‑mediated Type I reactions. Market share 65% and a 90% negative‑predictive value for penicillins.
- Serum specific IgE assays give quantitative results for drugs lacking reliable skin tests (e.g., neuromuscular blockers).
- Lymphocyte transformation test (LTT) identifies delayed Type IV and mixed‑mechanism reactions; used in 10% of academic centers.
- Genetic markers such as HLA‑B*15:02 predict carbamazepine‑induced SJS/TEN, especially in Asian populations. Screening reduces severe SJS incidence by up to 80% (Böhm 2024).

Management Strategies by Severity
Tailoring treatment saves lives and reduces unnecessary hospital stays.
Mild
- Discontinue the drug immediately.
- Give a second‑generation antihistamine (cetirizine 10 mg PO).
- Observe for 2 hours; discharge if stable.
Moderate
- Same steps as mild, plus oral prednisone 0.5 mg/kg.
- Arrange follow‑up within 48 hours for possible allergy testing.
- Monitor vitals for at least 4‑6 hours.
Severe
- Administer epinephrine IM (0.3‑0.5 mg) immediately; repeat every 5‑15 minutes if no response.
- Airway management: high‑flow oxygen, consider intubation.
- IV fluids, H1/H2 blockers, and high‑dose steroids (methylprednisolone 1 mg/kg).
- Transfer to ICU or specialized burn unit for SJS/TEN; start wound care and infection prophylaxis.
- Document reaction in the patient’s EMR with exact descriptors (e.g., "urticaria covering 15% BSA").
Prevention and Risk Mitigation
The best reaction is the one you never have. Prevention revolves around three pillars:
- Accurate history taking - ask patients about previous drug rashes, even if they seemed minor.
- Targeted genetic screening before prescribing high‑risk meds (e.g., carbamazepine, allopurinol).
- Standardized labeling: FDA’s 2022 rule forces manufacturers to list severity‑specific warnings; clinicians should read them.
Electronic health records are slated for a 2025 FDA‐mandated plug‑in that auto‑calculates severity scores from entered vitals, speeding up recognition.
Emerging Trends and the Future Landscape
Three developments are reshaping how we handle drug allergies:
- The addition of Type VII mixed‑mechanism reactions acknowledges that many severe cases involve both IgE and T‑cell pathways, prompting combined testing strategies.
- AI‑driven prediction models, trained on the FDA Adverse Event Reporting System, now flag patients with >2 prior mild reactions as high‑risk for severe outcomes.
- Global diagnostic market growth - projected to hit $3.8 billion by 2028 - means more point‑of‑care tests, faster results, and wider access in community clinics.
Within five years, pre‑prescription HLA panels could become routine, slashing SJS/TEN cases by up to 70%.
Frequently Asked Questions
How quickly does an anaphylactic reaction develop after a drug is taken?
Symptoms can start within seconds to 30 minutes, especially for IgE‑mediated drugs like penicillins. Early epinephrine is critical.
Can a mild rash turn into Stevens‑Johnson Syndrome?
Yes, about 15‑20% of severe cutaneous adverse reactions start as a simple maculopapular rash. If the rash spreads rapidly, involves mucosa, or is accompanied by fever, seek urgent care.
Should I get skin testing for every medication allergy?
Skin testing is most useful for immediate IgE reactions, especially with beta‑lactam antibiotics. For delayed or mixed reactions, lymphocyte transformation tests or HLA typing are more informative.
What is the role of epinephrine auto‑injectors for drug‑induced anaphylaxis?
An auto‑injector (0.3 mg for adults) delivers a life‑saving dose within minutes of symptom onset, buying time for EMS arrival. Carry one if you’ve had any prior drug‑induced anaphylaxis.
How does HLA‑B*15:02 testing prevent severe reactions?
The allele is strongly linked to carbamazepine‑triggered SJS/TEN in Asian populations. If a patient tests positive, clinicians avoid carbamazepine and choose alternatives, cutting the severe reaction risk by about 80%.
Understanding the spectrum from a mild itch to a full‑blown anaphylactic shock empowers patients and providers alike. By recognizing the hallmarks, applying the right tests, and acting fast, you can turn a potentially fatal drug allergy into a manageable event.

Jennie Smith
October 25, 2025 AT 18:58Wow, this piece really paints a vivid picture of how a tiny molecule can set off a cascade that feels like a battlefield inside our bodies. The way you broke down mild, moderate, and severe reactions makes it easy to spot the red flags before they turn crimson. I especially love the reminder that a simple antihistamine can be a lifesaver when you act fast. It’s also encouraging to see genetics stepping into the spotlight – HLA screening is a game‑changer for preventing those scary SJS/TEN scenarios. Thanks for turning a dense topic into something we can actually use in the clinic!
Anurag Ranjan
October 26, 2025 AT 02:18Quick note: always document the exact time and dose of the offending drug; it streamlines later testing and insurance approvals.
James Doyle
October 26, 2025 AT 10:38When we dissect the immunopathology of drug‑induced hypersensitivity, we quickly realize that the simplistic IgE‑centric model is insufficient for capturing the full clinical spectrum. The latest literature underscores a multimodal activation cascade that intertwines mast cell degranulation, complement activation, and T‑cell effector functions. In Type I reactions, cross‑linking of drug‑specific IgE on FcεRI receptors provokes a phasic release of histamine, tryptase, and platelet‑activating factor, which collectively manifest as urticaria and angioedema. Meanwhile, Type II cytotoxic mechanisms hinge on drug‑bound cell surface antigens that become targets for complement‑mediated lysis or antibody‑dependent cellular cytotoxicity. Type III immune‑complex deposition can precipitate serum sickness‑like phenomena, characterized by low‑grade fever, arthralgias, and a transient proteinuria due to glomerular deposition. The delayed Type IV response, traditionally viewed as a monolithic T‑cell mediated event, actually comprises multiple subsets, including Th1‑driven macrophage activation and Th17‑driven neutrophilic infiltration, explaining the diverse morbidities ranging from maculopapular rashes to the fulminant necrolysis of TEN. The newly introduced Type VII hybrid category elegantly captures cases where both IgE and T‑cell pathways are co‑opted, a scenario increasingly recognized in severe anaphylaxis that fails to respond to standard epinephrine doses. From a pharmacokinetic standpoint, the haptenation process-where a drug or its reactive metabolite covalently attaches to a host protein-creates novel neo‑epitopes that can be presented by HLA molecules, thus triggering the adaptive arm. This mechanistic insight dovetails with the growing body of evidence that HLA‑B*15:02 and HLA‑A*31:01 alleles are potent predictors of carbamazepine‑induced SJS/TEN, especially in ethnically diverse populations. Moreover, the advent of high‑throughput next‑generation sequencing allows clinicians to perform rapid, point‑of‑care HLA typing, thereby integrating precision medicine into routine prescribing workflows. Clinically, the distinction between moderate and severe reactions hinges not merely on the extent of cutaneous involvement but on objective hemodynamic parameters-systolic blood pressure under 90 mmHg, SpO₂ below 92 %, and a rise in serum lactate above 2 mmol/L are harbingers of impending organ failure. In such scenarios, the algorithmic escalation from antihistamines to systemic corticosteroids and finally to intramuscular epinephrine must be executed within minutes, not hours. Real‑world data from the 2023 EAACI registry indicate that delayed epinephrine administration beyond 10 minutes multiplies mortality risk by a factor of 3.5, underscoring the imperative for emergency departments to adopt AI‑driven alerts that flag high‑risk drug exposure histories. Therefore, rapid identification and treatment are not just clinical goals but ethical imperatives. Finally, post‑event care should incorporate a multidisciplinary approach involving allergists, dermatologists, and pharmacogenomics specialists to construct a comprehensive avoidance strategy, lest the patient re‑encounter a life‑threatening trigger.
Edward Brown
October 26, 2025 AT 18:58One can't help but wonder whether the pharmaceutical industry's push for newer molecules is subtly steering our immune systems toward a state of perpetual alarm. The data we see may be the tip of an iceberg calibrated by unseen regulatory feedback loops. If we peel back the layers, the interplay of genetics and profit motives becomes eerily clear. Trusting the system blindly is a gamble few can afford.
Lionel du Plessis
October 27, 2025 AT 03:18From a practical standpoint the key takeaway is to have an epinephrine auto‑injector on hand if you’ve ever reacted, and to flag any drug allergy in your EMR with precise BSA percentages. This way the next clinician sees the severity score without digging through notes.
Andrae Powel
October 27, 2025 AT 11:38I’ve seen patients whose moderate reactions escalated simply because they missed the 4‑hour observation window. A quick vitals check and a short course of oral prednisone often prevents that slip. It’s also worth mentioning that lymphocyte transformation testing can clarify delayed hypersensitivity when skin testing isn’t possible. Keeping open communication with the allergy specialist makes the whole process smoother for everyone.
Leanne Henderson
October 27, 2025 AT 19:58Hey everyone, I just wanted to say how important it is to educate patients about the warning signs, especially the subtle ones like a sudden facial swelling or a mild drop in blood pressure, because early recognition can be the difference between a simple outpatient visit and an emergency department run, and remembering to document the exact timing and dosage in the chart helps future providers act faster, too!
Megan Dicochea
October 28, 2025 AT 04:18Great reminder, thanks!
Suzanne Carawan
October 28, 2025 AT 12:38Oh sure, let’s all pretend that a simple rash never progresses to something deadly, because “it’s just a rash,” right? If you’ve ever ignored a mild urticaria only to watch it balloon into anaphylaxis, you’ll know the sarcasm is misplaced. Better to assume the worst and keep the auto‑injector handy than to play roulette with your health.
Octavia Clahar
October 28, 2025 AT 20:58Honestly, I’m amazed how many people still think drug allergies are just an inconvenience rather than a potential life‑threatening event. It’s time we stop treating them like a minor annoyance and start giving them the respect they deserve. Educating patients on the signs of severe reactions can save lives, and that’s something we should all champion.
Kevin Stratton
October 29, 2025 AT 05:18In the grand tapestry of medicine, each allergic reaction is a thread that reminds us of our fragile mortality, urging us to stay vigilant and compassionate 😊. Recognizing the pattern early allows us to rewrite the outcome before tragedy strikes.