When your doctor talks about a biologic drug - maybe for rheumatoid arthritis, Crohn’s disease, or cancer - you might hear the word biosimilar come up. It sounds confusing. Is it a copy? Is it safe? Will it work the same? Here’s the truth, in plain language: biosimilars are not generics, but they’re not experiments either. They’re highly tested, FDA-approved versions of complex biologic medicines, designed to work just like the original - at a lower cost.
What Makes a Biologic Different From Regular Medicine?
Most pills you take, like aspirin or metformin, are made from chemicals. They’re small, simple molecules. You can recreate them exactly in a lab. That’s what generics are: exact copies of those chemical drugs. Biologics are different. They’re made from living cells - yeast, bacteria, or animal cells - engineered to produce proteins that treat disease. Think of them as tiny, complex machines built by biology. Examples include drugs like Humira (adalimumab), Enbrel (etanercept), and Herceptin (trastuzumab). These are used for autoimmune diseases, cancer, and diabetes. Because they come from living systems, no two batches of a biologic are perfectly identical. Even the original manufacturer can’t make them exactly the same every time. That’s why you can’t make a perfect copy. And that’s why biosimilars exist.What Exactly Is a Biosimilar?
A biosimilar is a biologic medicine that is highly similar to an already approved biologic - called the reference product. It’s not identical, but it’s close enough that it works the same way in your body. The FDA requires biosimilars to go through more than 100 tests before approval. These include:- Testing the protein’s shape and structure
- Measuring how it behaves in the body (bioactivity)
- Checking for purity and contamination
- Running clinical trials comparing side effects and effectiveness
Biosimilars vs Generics: The Big Difference
This is where people get confused. Generics and biosimilars both save money. But they’re not the same.| Feature | Generic Drug | Biosimilar |
|---|---|---|
| What it copies | Small-molecule chemical drug | Large, complex biologic protein |
| Can it be identical? | Yes - chemically identical | No - highly similar, but not identical |
| Manufacturing | Chemical synthesis in a lab | Living cells in bioreactors |
| Testing required | Basic bioequivalence studies | Extensive analytical, animal, and clinical trials |
| Examples | Generic ibuprofen, metformin | Hyrimoz (adalimumab), Ogivri (trastuzumab) |
Are Biosimilars Safe?
Yes. The FDA approves them only after proving they’re as safe and effective as the original. In Europe, biosimilars have been used for over 15 years. Millions of patients have taken them. Studies show no increase in side effects or loss of effectiveness over time. The FDA tracks every biosimilar through post-market surveillance. If a problem shows up - even years later - they investigate it. That’s how they know these drugs stay safe in the real world. You might hear stories about people switching from a brand-name biologic to a biosimilar and feeling different. That’s possible - but it’s not because the biosimilar is worse. It’s because your body responds differently to any change in medication. That’s why your doctor always checks in after a switch.
Why Do Biosimilars Cost Less?
Developing a biologic can cost over $1 billion. Biosimilar makers don’t have to repeat all the early research. They start from the approved reference product. That cuts development time and cost. As a result, biosimilars typically cost 15% to 30% less than the original biologic. That’s not as big a discount as generics (which can be 80% cheaper), but it still adds up - especially for drugs you take for life. In the U.S., insurance companies often push for biosimilars because they’re cheaper. You might get a letter saying your plan requires you to try the biosimilar first. That’s called a step therapy rule. It’s not about your health - it’s about cost.What Do Biosimilars Look Like on Your Prescription?
The original biologic has a brand name (like Humira) and a generic name (adalimumab). The biosimilar has a brand name too (like Hyrimoz) - but its generic name is the same as the original, with a four-letter suffix added to tell them apart. So:- Original: adalimumab (Humira)
- Biosimilar: adalimumab-hjdb (Hyrimoz)
Can You Switch From the Original to a Biosimilar?
Yes. Studies show switching is safe. The Arthritis Foundation, the American Cancer Society, and the FDA all agree: switching from a brand-name biologic to a biosimilar doesn’t increase risk. Many patients have switched back and forth without issues. If your doctor says it’s okay, you can switch. If you’re nervous, ask for time to think about it. You’re not obligated to switch right away.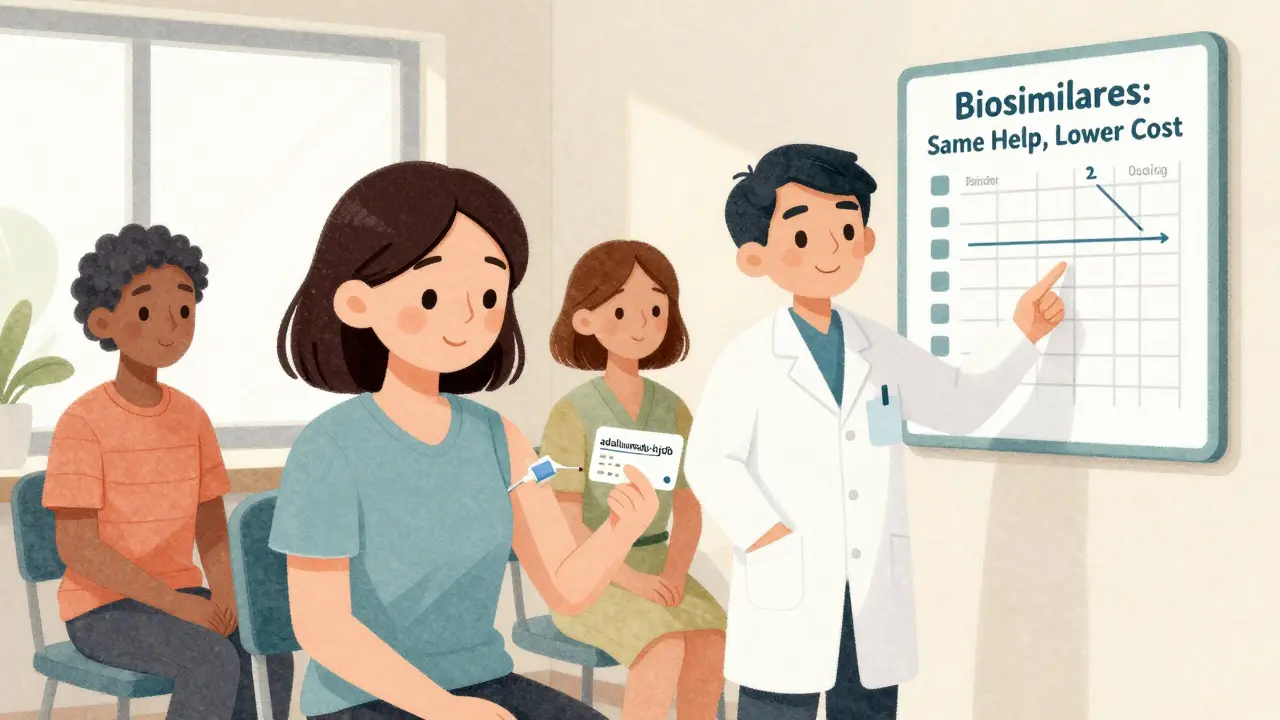
What About “Interchangeable” Biosimilars?
There’s a special category called “interchangeable” biosimilars. These are biosimilars that the FDA says can be swapped for the original drug without the doctor’s approval - just like a generic. The first one approved was Semglee, an interchangeable version of insulin glargine (Lantus), in 2021. More are coming. But even if a biosimilar isn’t labeled “interchangeable,” it’s still safe and effective. The label just means the pharmacist can swap it without calling your doctor.What Should You Do as a Patient?
Here’s what matters most:- Don’t panic. Biosimilars aren’t cheap knockoffs. They’re rigorously tested.
- Ask questions. If your doctor suggests a biosimilar, ask: “Is this the same as my current drug? Will it work the same way?”
- Check your insurance. They might require you to try the biosimilar first. That’s normal.
- Know your drug name. Write down the full name - brand and generic with suffix - so you don’t get confused.
- Report side effects. If something feels off, tell your doctor. It’s rare, but important.
The Bottom Line
Biosimilars are a smart, science-backed way to make life-changing biologic treatments more affordable. They’re not perfect copies - but they’re close enough to work just as well. And for millions of people with chronic conditions, that means better access, lower costs, and the same chance at a good quality of life. They’re not magic. They’re medicine - carefully made, carefully tested, and carefully approved.Are biosimilars the same as generics?
No. Generics are exact chemical copies of simple drugs, like aspirin or metformin. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They can’t be identical, but they work the same way in your body after passing strict FDA tests.
Are biosimilars safe to use?
Yes. The FDA requires biosimilars to go through over 100 tests, including clinical trials with hundreds of patients. They must prove they’re as safe and effective as the original biologic. Millions of patients in Europe and the U.S. have used them without unexpected safety issues.
Can I switch from my current biologic to a biosimilar?
Yes. Studies show switching is safe and effective. Many patients have switched back and forth between the original and biosimilar without problems. Always talk to your doctor first - but don’t assume you can’t switch. It’s a common and approved practice.
Why do biosimilars cost less than the original drugs?
Developing a new biologic costs over $1 billion. Biosimilar makers use the approved original drug as a blueprint, so they don’t need to repeat early research. This cuts costs, and savings are passed on - typically 15% to 30% less than the brand-name version.
Will my insurance cover a biosimilar?
Most insurance plans encourage or require biosimilars because they’re cheaper. You might be asked to try the biosimilar first before they pay for the brand-name drug. This is called step therapy. It’s legal and common - but you can always ask your doctor to appeal if you have concerns.
What does the four-letter suffix on biosimilar names mean?
It’s a unique identifier added to the generic name to tell the biosimilar apart from the original and other biosimilars. For example, adalimumab-hjdb (Hyrimoz) is different from adalimumab-afzb (Cyltezo). This helps doctors and pharmacists track which drug you’re taking, especially if you have side effects.

Alexandra Enns
January 23, 2026 AT 17:29Let me stop you right there - biosimilars are just Big Pharma’s way of keeping you hooked while they milk the system. The FDA? Controlled by lobbyists. That ‘no clinically meaningful difference’ line? Total BS. I’ve seen people go from Humira to some cheap knockoff and end up in the ER with rashes and fevers. They’re not the same. They can’t be. Living cells? Please. You can’t replicate biology like it’s a Lego set.
And don’t even get me started on those four-letter suffixes - that’s not for safety, that’s to confuse you so you don’t realize you’re being swapped out like a cheap battery. This isn’t medicine. It’s corporate sabotage dressed in white coats.
Marie-Pier D.
January 23, 2026 AT 22:24Oh my gosh, I’m so glad someone finally explained this clearly!! 💖 I was terrified when my doctor switched me to Hyrimoz - I thought I was being ‘downgraded’ or something. But reading this made me feel so much better. My rheumatoid arthritis hasn’t flared since the switch, and my co-pay dropped from $120 to $35. I’m crying happy tears 😭 Thank you for not making this sound like a scary sci-fi movie. You’re a lifesaver!!
Dolores Rider
January 25, 2026 AT 02:31They’re lying. Biosimilars are a Trojan horse. You think you’re getting the same drug? Nah. The original biologic has a ‘signature’ - like a fingerprint - that only the original manufacturer can replicate. The biosimilar makers? They reverse-engineer it with cheap lab tech and Chinese raw materials. Then they sneak it past the FDA because the regulators are on payroll.
And that ‘four-letter suffix’? That’s not for tracking - it’s so they can kill you quietly if you report side effects. The CDC’s database? All scrubbed. I’ve got screenshots. Ask me for them.
Jenna Allison
January 25, 2026 AT 19:30Just to clarify - biosimilars aren’t ‘copies’ at all. They’re ‘highly similar biologics’ with the same mechanism of action, but minor structural variations due to the complexity of mammalian cell expression systems. The key is that these variations don’t impact clinical outcomes - which is why over 100 analytical assays, pharmacokinetic studies, and immunogenicity assessments are required.
Also, the FDA’s ‘no clinically meaningful difference’ standard is legally binding. If a biosimilar fails even one of the 100+ tests, it’s rejected. So yes, they’re safe. No magic. Just science. And yes, they save lives and money. That’s not a bug - it’s a feature.
Sharon Biggins
January 26, 2026 AT 01:36I switched to a biosimilar last year after being on Humira for 5 years. I was nervous - super nervous. But my rheumatologist sat with me for 20 minutes and explained everything. I didn’t feel any different. No new rashes, no fatigue spikes. I even saved $800 a month.
Don’t let fear scare you. Talk to your doc. Ask questions. You’ve got this. 💪 And if you’re worried? You can always switch back. Your body, your choice.
John McGuirk
January 27, 2026 AT 00:41Let’s be real - this whole biosimilar thing is just the pharma industry’s way of getting around patent laws. They didn’t invent anything. They just watched the original company spend a billion dollars and then copied the damn thing. Now they’re calling it ‘science’?
And don’t tell me about ‘clinical trials’ - those are run by the same companies that make the drugs. It’s a closed loop. You think the FDA is independent? LOL. I’ve seen the documents. They’re in bed with Merck and Pfizer.
Meanwhile, real patients are being turned into lab rats. And you’re all clapping because your insurance card says ‘approved’? Pathetic.
Michael Camilleri
January 27, 2026 AT 13:40It’s not about whether biosimilars work - it’s about what this says about our society. We’ve reduced human suffering to a spreadsheet. We don’t care about the soul of medicine anymore - only the bottom line. A biologic isn’t just a protein - it’s hope. It’s dignity. It’s the quiet moment when someone breathes without pain for the first time in years.
And now we’re swapping it for a cheaper version because the insurance company doesn’t want to pay $10,000 a month? That’s not progress. That’s moral decay.
Yes, it’s safe. But is it right? That’s the question nobody’s asking.
Darren Links
January 27, 2026 AT 13:45Okay but have you ever heard of the ‘biosimilar paradox’? The more they try to prove it’s the same, the more they prove it’s NOT. If it were truly identical, why the hell do they need 100 tests? Why not just one? Because biology isn’t math. You can’t replicate a living system like it’s a spreadsheet.
And the suffixes? That’s not safety - that’s liability. They know something’s off. They just don’t want you to sue them. They want you to think you’re getting the same thing. You’re not. You’re getting a version with unknown variables.
Ask yourself: if it’s so safe, why don’t they let you switch without a doctor’s note? Oh wait - they do now. That’s the red flag.
Husain Atther
January 27, 2026 AT 16:58This is a very balanced and thoughtful explanation. As someone from India, where access to expensive biologics is a major barrier, biosimilars have been a game-changer. My cousin with Crohn’s disease started on a biosimilar last year - she’s now able to work again and even travel. No side effects. No issues.
Science doesn’t care about borders. What matters is whether it helps people. And it does. Let’s not let fear or conspiracy theories take away hope from those who need it most.
Helen Leite
January 28, 2026 AT 16:18THEY’RE HIDING SOMETHING!! 😱 I read a Reddit thread where a guy said his biosimilar made him hallucinate. He thought his cat was talking to him!! 🐱🗣️ And then the hospital said it was ‘anxiety’ - but he was on the biosimilar for 3 days! That’s not anxiety - that’s chemical poisoning!!
And why do they call it ‘adalimumab-hjdb’? Why not just ‘Humira 2.0’? Because they don’t want you to know it’s the same drug!! It’s all a cover-up!! 🚨 I’m switching back to the original - I’d rather pay $1000 a month than risk my brain!!
asa MNG
January 28, 2026 AT 18:50yo so i got switched to some biosimilar and now my knees hurt more?? like wtf?? i thought this was supposed to be the same??
my doc says its all in my head but i swear i felt better on humira. now i get dizzy after the shot. also i think my blood is turning to sludge. i checked on google and its all bad signs. i demand my old drug back. they are lying to us. the gov is in on it. i saw a video of a guy in a lab coat laughing while injecting it. i know what i saw. send help.
Sushrita Chakraborty
January 29, 2026 AT 13:13While the article presents a scientifically accurate overview of biosimilars, it is worth noting that the regulatory frameworks in the European Union, which have been in place for over 15 years, demonstrate a higher degree of transparency and post-marketing surveillance than those currently operational in the United States. Additionally, the nomenclature system - while necessary - should be standardized globally to prevent confusion among healthcare providers and patients. The four-letter suffix, though functional, lacks linguistic intuitiveness and may impede patient comprehension in non-English-speaking populations. A more inclusive approach to naming is both ethically and practically imperative.
lorraine england
January 29, 2026 AT 21:39I totally get why you’re nervous - switching meds is scary. But honestly? My mom’s been on a biosimilar for her psoriasis for two years now. No flare-ups, no weird side effects. She says it feels just like before.
And yeah, it’s cheaper - but that’s not the point. The point is she can afford to keep living. I think that’s kind of beautiful. You don’t have to be a hero to choose safety and savings. You just have to be human.
Himanshu Singh
January 30, 2026 AT 07:39There’s a quiet revolution happening here. We’re not just talking about drugs - we’re talking about access. For years, biologics were reserved for the wealthy. Biosimilars are changing that. A child in rural India can now get treatment that once cost more than their family’s annual income.
It’s not about perfection. It’s about possibility. The science is sound. The results are real. Let’s not let fear, misinformation, or ego block the door to healing for millions.
Medicine isn’t about brands. It’s about breath. And every breath matters.
Jamie Hooper
January 31, 2026 AT 16:48so i just got switched to this biosimilar thing and now my insurance says im not allowed to go back to humira?? like what?? i didnt even get to choose??
and why does my pill bottle say adalimumab-hjdb?? who even made up that word?? sounds like a virus name. i think they’re trying to make us forget what we’re taking. this is a cult. i’m calling my senator.