Medication Heartburn Risk Calculator
How to use this tool
Select your medications and answer a few simple questions to get your personalized heartburn risk assessment. This tool is based on the latest medical research about medication side effects.
Many people take medications every day without thinking twice-until their stomach starts burning, or they feel that familiar sour taste rising in their throat. Heartburn and upset stomach from pills aren’t just inconvenient. They’re common, often avoidable, and sometimes dangerous if ignored. You might assume it’s just bad luck or something you ate, but the truth is, your medication could be the real culprit.
Which Medications Are Most Likely to Cause Heartburn?
Not all pills are created equal when it comes to stomach irritation. Some are notorious for triggering heartburn, even in people who’ve never had acid reflux before.
NSAIDs like ibuprofen and aspirin are the top offenders. Around 20-30% of people who take ibuprofen regularly get heartburn from it. Aspirin isn’t far behind, hitting 15-25%. These drugs work by blocking enzymes that cause pain and swelling, but they also shut down protective chemicals in your stomach lining. Without those, stomach acid starts eating away at the tissue. Chronic use can raise your risk of ulcers from less than 2% to over 15%.
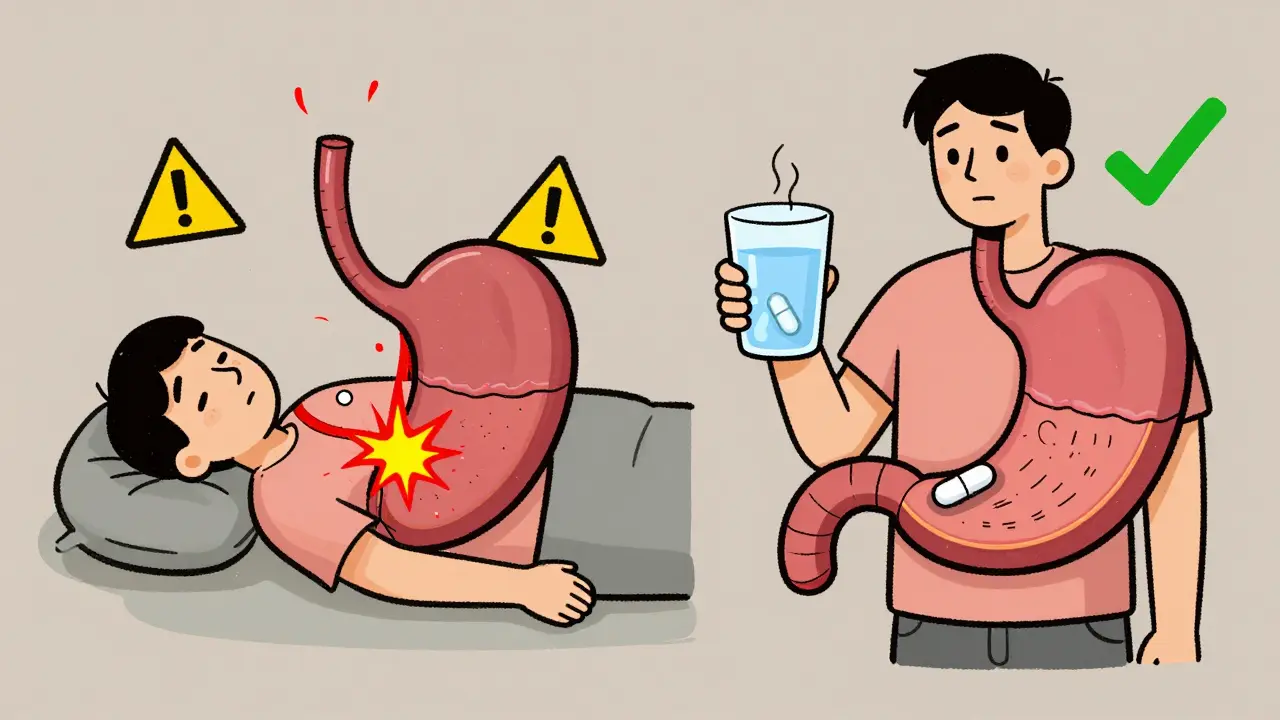
Tetracycline antibiotics, especially doxycycline, are another big problem. If you take it without enough water or lie down right after, the pill can get stuck in your esophagus. That leads to pill-induced esophagitis-inflammation and even ulcers. About 12% of people who don’t follow the rules end up with this. It’s not rare. It’s preventable.
Calcium channel blockers, used for high blood pressure, relax the muscle between your stomach and esophagus. That’s good for your arteries, but bad for your reflux. About 10-20% of users report heartburn. Amlodipine and nifedipine are the usual suspects. Beta blockers, on the other hand, cause heartburn in only 5-10% of people-making them a better option if you’re already prone to acid reflux.
Metformin, the go-to drug for type 2 diabetes, hits about 20-30% of new users with nausea, bloating, and heartburn. It’s not an allergy. It’s a side effect that usually fades after 2-4 weeks. Still, that first month can feel unbearable.
Bisphosphonates like alendronate (for osteoporosis) are the most dangerous if misused. If you don’t take them with a full glass of water and stay upright for an hour, they can burn holes in your esophagus. About 5-10% of users develop serious injury. Hospitalizations happen. And they’re almost always avoidable.
Why Do Pills Cause Heartburn? It’s Not Just Acid
It’s not just about stomach acid spilling upward. The problem is more complex.
Some drugs directly irritate the lining of your esophagus or stomach. That’s why doxycycline and bisphosphonates are so risky-they’re harsh chemicals that don’t dissolve quickly. If they linger, they burn.
Others relax the lower esophageal sphincter (LES), the muscle that keeps stomach contents from backing up. Calcium channel blockers and theophylline (used for asthma) do this. When the LES loosens, acid flows back easily-even if you haven’t eaten anything spicy.
And then there are drugs like NSAIDs that reduce protective prostaglandins. These chemicals normally help your stomach repair itself and produce mucus to shield against acid. Take them away, and your stomach becomes vulnerable. That’s why even a low-dose aspirin can cause trouble over time.
What You Can Do Right Now
You don’t have to suffer-or quit your meds-just because your stomach hurts.
Take pills with a full glass of water-at least 8 ounces. This isn’t just advice. It’s science. Drinking enough water helps the pill move through your esophagus fast, reducing contact time. For doxycycline and bisphosphonates, this cuts esophagitis risk by 60-70%.
Stay upright for at least 30 minutes after taking your pill. No lying down. No slouching on the couch. No napping. This simple habit prevents 80-90% of pill-induced esophagitis cases. It’s that effective.
Take NSAIDs with food. Eating before or with ibuprofen or naproxen reduces heartburn by 40-50%. Food acts like a buffer. It doesn’t stop the drug from working, but it keeps it from directly touching your stomach lining.
Try an antacid before your pill. If you know you’re going to take an NSAID, pop an over-the-counter antacid like Tums or Rolaids 30 minutes beforehand. It lowers heartburn chances by 30-40%. It’s cheap, fast, and doesn’t interfere with most medications.
Ask about PPIs if you’re on long-term NSAIDs. If you’re taking ibuprofen daily for arthritis or back pain, your doctor might recommend a proton pump inhibitor like omeprazole. Studies show PPIs cut NSAID-related ulcer risk by 70-80%. It’s not a cure-all, but for high-risk users, it’s a game-changer.
When to Worry-Red Flags You Can’t Ignore
Most medication-induced heartburn is annoying, not life-threatening. But some signs mean you need help now.
- Chest pain that feels like pressure or squeezing-especially if it spreads to your arm or jaw. This isn’t heartburn. It could be your heart.
- Difficulty swallowing-like food is getting stuck. That’s a sign of esophageal narrowing or scarring.
- Bloody vomit or black, tarry stools. These mean bleeding in your GI tract. NSAIDs are the usual cause.
- Unexplained weight loss or persistent nausea. Could be something deeper.
If you have any of these, don’t wait. See your doctor. Delaying care can lead to strictures (narrowing of the esophagus) or Barrett’s esophagus-a condition that slightly raises your risk of esophageal cancer.
What About Stopping the Medication?
It’s tempting. You’re in pain. You want relief. But quitting your meds without talking to your doctor can be dangerous.
Stopping beta blockers suddenly can cause a spike in blood pressure or even a heart attack. Discontinuing metformin without a plan can send your blood sugar out of control. Tapering off some drugs requires medical supervision.
According to research, about 7% of patients stop their prescriptions because of stomach issues-even though simpler fixes exist. That’s unnecessary risk. Your doctor can switch you to a gentler alternative, adjust the dose, or add protective meds. Don’t assume you have to suffer.

New Solutions on the Horizon
Pharma companies are listening. In 2022, the FDA approved a new delayed-release version of doxycycline that dissolves lower in the digestive tract-cutting esophageal exposure by nearly half. In 2023, new coated NSAIDs showed 30-35% fewer stomach complaints in clinical trials.
Hospitals are starting to use AI tools in electronic records that flag risky drug combinations before they’re even prescribed. If you’re on blood pressure meds and NSAIDs, the system might alert your doctor to switch one of them.
Future options include patches and sprays that deliver drugs through the skin or under the tongue-bypassing the stomach entirely. These are still in trials, but they could change everything for people who can’t tolerate pills.
Bottom Line: You Have Control
Medication-induced heartburn isn’t a life sentence. It’s not your fault. And it’s not something you just have to live with.
Start with the basics: water, upright posture, food with NSAIDs. Talk to your doctor about alternatives or protective meds. Don’t stop your prescriptions unless they tell you to. And if something feels wrong-really wrong-get it checked.
Thousands of people manage these side effects every day without quitting their meds. You can too. It’s not about avoiding pills. It’s about taking them smarter.
Can ibuprofen cause long-term stomach damage?
Yes, especially with daily use. Ibuprofen reduces protective chemicals in the stomach lining, which can lead to ulcers in 15-30% of long-term users. The risk jumps higher if you’re over 60, smoke, drink alcohol, or take other NSAIDs or steroids. Using a proton pump inhibitor like omeprazole alongside ibuprofen cuts this risk by 70-80%.
Why does doxycycline cause heartburn?
Doxycycline isn’t absorbed well in the stomach, so it stays in the esophagus longer. If you don’t drink enough water or lie down after taking it, the pill can stick and slowly burn the lining. This causes pill-induced esophagitis, which can lead to ulcers. Taking it with a full glass of water and staying upright for an hour prevents this in nearly all cases.
Is metformin heartburn permanent?
No. About 60-70% of people who get nausea, bloating, or heartburn from metformin find it improves or disappears within 2-4 weeks as their body adjusts. Taking it with food, starting with a lower dose, or switching to the extended-release version can help speed up tolerance. It rarely lasts longer than a month.
Can I take antacids with my medication?
Usually yes-but not always. Antacids like Tums or Maalox are safe with NSAIDs and can reduce heartburn. But they can interfere with antibiotics like tetracycline or thyroid meds by binding to them in the gut. Always check with your pharmacist. Take antacids at least 2 hours before or after other pills to avoid interactions.
Should I switch from NSAIDs to acetaminophen for pain?
For mild to moderate pain, yes. Acetaminophen (Tylenol) doesn’t irritate the stomach like NSAIDs do. It’s a safer choice if you’re prone to heartburn or ulcers. But it doesn’t reduce inflammation, so it won’t help with conditions like arthritis the same way ibuprofen does. Talk to your doctor about whether acetaminophen is strong enough for your needs.
Can heartburn from meds lead to cancer?
Not directly. But long-term, untreated acid reflux from meds can lead to Barrett’s esophagus-a condition where the esophagus lining changes to protect itself from acid. This increases the risk of esophageal cancer by 1-2% over many years. The key is managing reflux early. If you’ve had daily heartburn for more than 5 years, especially if you’re over 50, ask your doctor about an endoscopy.

Sangeeta Isaac
January 19, 2026 AT 20:09so i took doxycycline once like a total idiot and laid down right after… woke up feeling like my throat was a sandpaper sculpture. never again. water is not optional, it’s your new best friend.
Dee Monroe
January 20, 2026 AT 01:03you know what’s wild? we treat pills like candy-pop ‘em dry, lie back, and blame our stomachs. but if you handed someone a piece of glass and told them to swallow it without water, they’d call you crazy. yet we do this every day with meds. it’s not the drugs being evil-it’s us being lazy. the fact that staying upright for 30 minutes cuts esophagitis by 90%? that’s not magic, that’s basic physics. we just forgot how to respect our own bodies. maybe if we treated our insides like sacred temples instead of disposable vending machines, we’d be a lot less surprised when things break.
Ben McKibbin
January 20, 2026 AT 19:32the real tragedy isn’t the heartburn-it’s how many people stop their meds because they don’t know how to take them properly. i’ve seen patients quit metformin after one week of bloating, then show up months later with HbA1c at 11.5. same with NSAIDs-people think they’re allergic to ibuprofen when they’re just taking it on an empty stomach. the solution isn’t more drugs, it’s education. pharmacists should hand out little cards with each prescription: ‘Drink water. Stay upright. Eat first.’ simple, cheap, life-changing.
Philip Williams
January 22, 2026 AT 12:02as a medical researcher, i appreciate the clarity of this post. however, i must emphasize that the 70-80% reduction in ulcer risk with PPIs applies only to patients with documented high-risk profiles. indiscriminate prescribing of proton pump inhibitors introduces its own complications: nutrient malabsorption, increased C. diff risk, and potential rebound acid hypersecretion. a risk-benefit analysis is essential, not a reflexive prescription.
Alex Carletti Gouvea
January 22, 2026 AT 17:46why are we letting big pharma tell us how to take our pills? back in my day, you took your medicine like a man-no water, no food, no whining. if your stomach burns, you’re weak. america’s gone soft. just swallow the pill and deal with it. we don’t need antacids and upright posture-we need grit.
Uju Megafu
January 23, 2026 AT 12:27oh my god i knew it. this is all part of the pharmaceutical agenda. they make the drugs to hurt you, then sell you the antacids, then the PPIs, then the endoscopies. it’s a money machine. they don’t want you to heal-they want you to be a lifelong customer. and now they’re even using AI to trap you? i’m not taking anything anymore. i’m going back to turmeric and prayer.
Samuel Mendoza
January 24, 2026 AT 23:29metformin doesn’t cause heartburn. you’re just fat.
Steve Hesketh
January 26, 2026 AT 14:06bro, i felt every word of this. i was on doxycycline for acne and nearly ended up in the ER because i took it before bed with a sip of water. my throat felt like i’d swallowed a rusty nail. but then i started drinking a whole bottle of water, standing like a statue for 45 minutes, and boom-no more burning. it’s not rocket science. it’s just respect. and honestly? i feel more in control of my health now than i ever did before. y’all, we can do better.
shubham rathee
January 27, 2026 AT 01:38you know what really causes heartburn? the government and the FDA letting pharma companies sell these pills without mandatory video instructions. like imagine if every pill came with a 30 second tiktok: 'do not lie down' 'drink water' 'eat first' but no they want you confused so you keep buying more meds. also i think the sun is a hologram but that's beside the point
MAHENDRA MEGHWAL
January 28, 2026 AT 01:14while the practical recommendations provided are empirically sound and clinically validated, one must also consider the sociocultural determinants of medication adherence. in populations with limited health literacy, even the most precise instructions may be misinterpreted or disregarded. structured patient education programs, delivered in culturally appropriate formats, remain an underutilized intervention in mitigating iatrogenic gastrointestinal injury.
Kevin Narvaes
January 28, 2026 AT 08:33i’ve been thinking… what if our stomachs are just screaming because we’ve been living wrong? we rush, we stress, we swallow chemicals like they’re candy, then wonder why we feel broken. maybe the real problem isn’t the pills-it’s the life we’re living while taking them. i stopped taking everything for a month. just sat in silence. drank chamomile. cried a lot. and guess what? my heartburn disappeared. not because of water or food… because i finally listened.
Dee Monroe
January 28, 2026 AT 14:03philip’s point about PPI overuse is spot-on. i’ve been on them for 3 years for ibuprofen-induced reflux, and now i can’t digest protein without a supplement. it’s like we trade one problem for three new ones. i’m slowly weaning off, using food and posture as my new meds. it’s not glamorous, but it’s mine. and honestly? i feel more alive than i have in a decade.