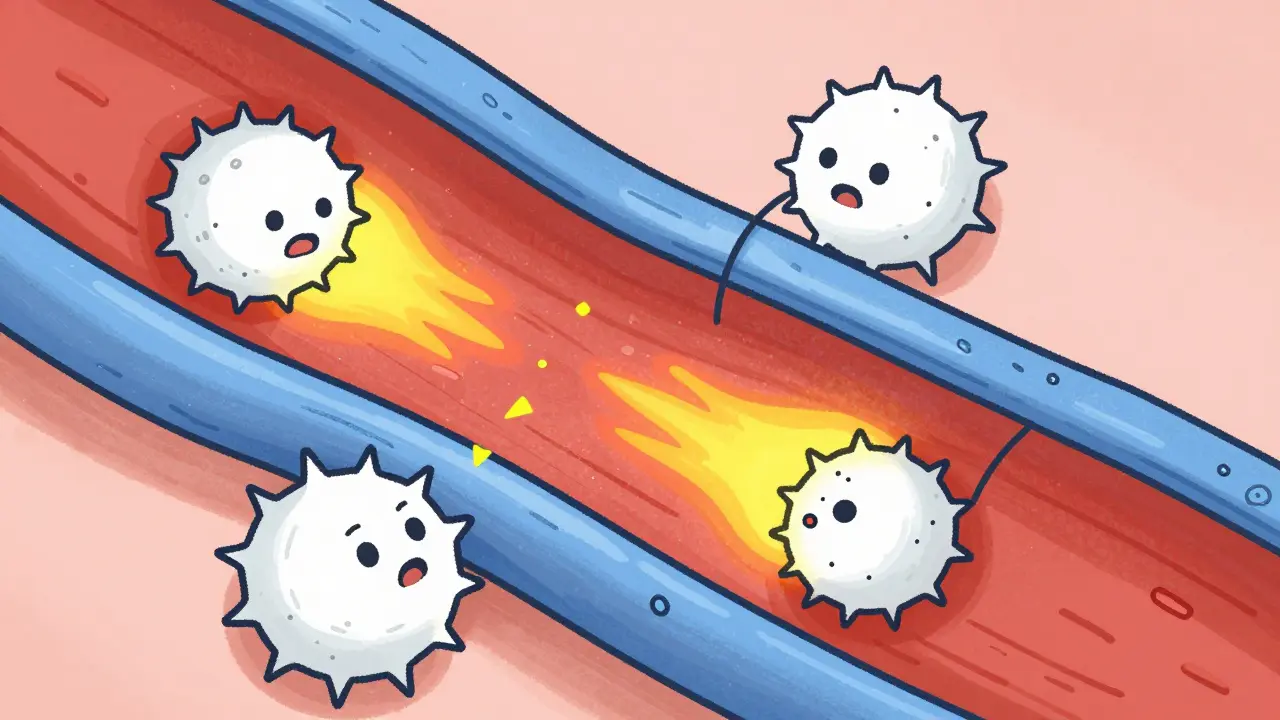
Vasculitis is a rare autoimmune condition where the immune system mistakenly attacks blood vessel walls, causing inflammation that can block blood flow and damage organs. While it affects only about 20 people per 100,000, early detection is critical to prevent serious complications like organ failure or aneurysms. According to the American College of Rheumatology (2023), vasculitis isn't a single disease but a group of disorders, each named based on the size of affected vessels.
What is Vasculitis?
Vasculitis occurs when your immune system gets confused and targets blood vessels as if they're foreign invaders. This leads to inflammation that can narrow or destroy vessels, reducing blood supply to tissues. Organs like kidneys, lungs, or nerves may not get enough oxygen, causing damage. There are over 20 types of vasculitis, each named based on the size of blood vessels involved. For example, Giant cell arteritis affects large arteries in the head, while Microscopic polyangiitis damages tiny capillaries in the kidneys and lungs.
How Vasculitis Affects Different Blood Vessels
Vasculitis types are classified by the size of the blood vessels involved. Large-vessel vasculitis includes conditions like Giant cell arteritis (GCA) and Takayasu arteritis. GCA commonly affects people over 50, causing severe headaches, jaw pain when chewing, and vision problems. Takayasu arteritis often appears in younger adults and can lead to arm pain or weak pulses in the arms.
| Vessel Size | Common Types | Key Symptoms |
|---|---|---|
| Large | Giant cell arteritis, Takayasu arteritis | Headaches, jaw pain, vision issues |
| Medium | Polyarteritis nodosa, Kawasaki disease | Abdominal pain, kidney problems, skin rashes |
| Small | Granulomatosis with polyangiitis, Microscopic polyangiitis, Eosinophilic granulomatosis with polyangiitis | Lung bleeding, kidney damage, nerve issues |
Medium-vessel vasculitis involves Polyarteritis nodosa (PAN) and Kawasaki disease. PAN typically causes abdominal pain, kidney issues, and skin rashes. Kawasaki disease mostly affects children under 5 and can lead to heart complications if untreated.
Small-vessel vasculitis includes ANCA-associated diseases like Granulomatosis with polyangiitis (GPA), Microscopic polyangiitis (MPA), and Eosinophilic granulomatosis with polyangiitis (EGPA). GPA often targets the sinuses, lungs, and kidneys, while MPA primarily damages kidneys and lungs. EGPA is linked to asthma and eosinophil buildup, affecting nerves and skin.
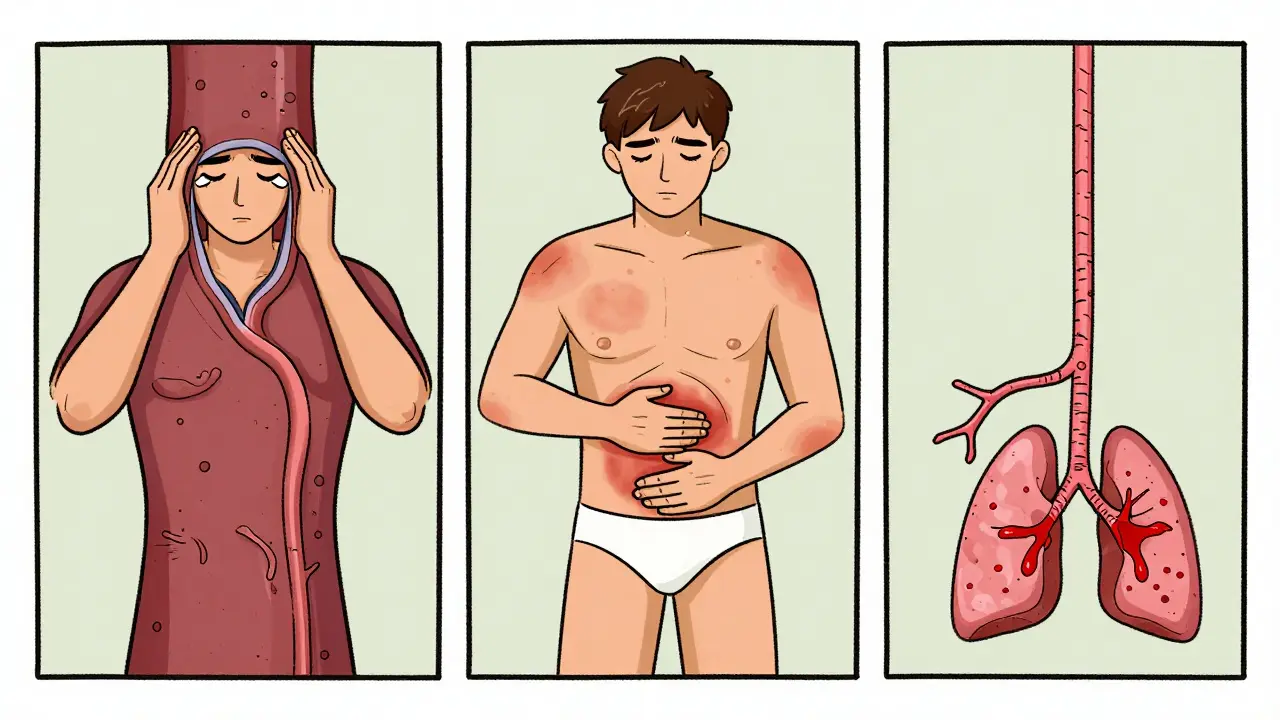
Recognizing Symptoms of Vasculitis
Symptoms vary widely based on which organs are affected. Common signs include:
- Skin changes: purple or red spots, bumps, or bruise-like rashes
- Joint pain and stiffness
- Numbness or tingling in hands/feet from nerve damage
- Shortness of breath or coughing up blood if lungs are involved
- Stomach pain or bloody stools from gastrointestinal issues
- Vision problems or headaches with jaw pain (for giant cell arteritis)
The American College of Rheumatology notes that kidney involvement is often silent-many patients have no symptoms until blood tests show protein or blood in urine. This is why routine urine tests are crucial for early detection.
Diagnosing Vasculitis: Tests and Challenges
Diagnosing vasculitis is tricky because symptoms mimic more common conditions like the flu or arthritis. On average, patients wait 6-12 months for a correct diagnosis. Doctors use multiple tests:
- Blood tests: High ESR (>50 mm/hr) or CRP (>5 mg/dL) indicate inflammation. ANCA blood tests detect autoantibodies-c-ANCA for GPA (80-90% specific) and p-ANCA for MPA.
- Imaging: CT scans or MRIs can show vessel inflammation or aneurysms.
- Tissue biopsy: A sample of affected tissue (like skin or kidney) is the gold standard. Pathologists look for inflammation in vessel walls, fibrinoid necrosis, or leukocytoclastic vasculitis.
Hospital for Special Surgery emphasizes that "getting an accurate diagnosis by a rheumatologist is important because, although these diseases are treatable, early intervention may be needed to avoid significant, irreversible organ damage."

Treatment Options for Vasculitis
Treatment depends on the type and severity. For severe cases, doctors usually start with high-dose corticosteroids (like prednisone) combined with immunosuppressants such as cyclophosphamide or Rituximab to quickly control inflammation. Maintenance therapy often continues for 18-24 months with drugs like methotrexate or azathioprine.
Recent advances include Avacopan, a newer drug approved in 2021. The CLEAR trial showed avacopan reduces steroid use by about 2,000 mg over a year while maintaining effectiveness. For giant cell arteritis, tocilizumab (an IL-6 inhibitor) is now used alongside steroids to lower long-term steroid doses.
Buerger's disease (thromboangiitis obliterans) requires complete smoking cessation-no other treatment works if smoking continues. University of Michigan Health specialists confirm that "continued smoking renders all other treatments ineffective."
Living with Vasculitis: Prognosis and Management
With treatment, 80-90% of ANCA-associated vasculitis patients achieve remission. However, relapse rates are high-about 50% within five years. The Five Factor Score helps predict outcomes: patients without major organ involvement have a 95% five-year survival rate, while those with two or more factors (like kidney or heart issues) drop to 50%.
Managing vasculitis involves regular check-ups, blood tests, and monitoring for side effects from medications. Patients often work closely with rheumatologists to adjust treatment as needed. Lifestyle changes like quitting smoking (for Buerger's disease), avoiding infections, and managing stress also play key roles. Cleveland Clinic physicians note that "most people with vasculitis can manage their symptoms with medication," but emphasize "the swelling makes it hard for blood to flow through affected vessels, which can cause organ and tissue damage requiring careful monitoring."
Can vasculitis be cured?
While vasculitis often can't be cured, most people achieve remission with treatment. However, relapses are common-about 50% within five years. Ongoing monitoring and medication adjustments are usually needed to keep the disease under control.
What are the first signs of vasculitis?
Early symptoms vary but commonly include unexplained fatigue, joint pain, skin rashes (purple spots or bumps), and numbness in hands or feet. Some people experience fever, weight loss, or shortness of breath. If these symptoms persist, see a doctor-especially if you have a history of autoimmune conditions.
How is vasculitis diagnosed?
Diagnosis requires blood tests (like ESR, CRP, ANCA), imaging scans (CT or MRI), and often a tissue biopsy. Biopsies of affected skin, kidneys, or other organs show inflammation in vessel walls. Because symptoms overlap with other conditions, it typically takes 6-12 months to get a correct diagnosis.
Is vasculitis hereditary?
Vasculitis isn't directly inherited, but certain genetic factors may increase risk. For example, some HLA gene variants are linked to higher susceptibility. However, environmental triggers like infections or medications often play a bigger role in causing the condition.
Can children get vasculitis?
Yes. Kawasaki disease is the most common vasculitis in children under 5. It affects blood vessels in the heart and can cause coronary artery aneurysms in 20-25% of untreated cases. Early treatment with IVIG and steroids usually prevents long-term damage.
Joyce cuypers
February 5, 2026 AT 01:37I have a friend with vasculitis. The symptoms started with joint pain and skin rashes. Wait, did they say 'kidne' or 'kidney'? I think it's a typo. Either way, thanks for the info!
Georgeana Chantie
February 5, 2026 AT 04:19In the US, we've got top-notch doctors. 😎 This article is too technical for normal people. Let's keep it simple!
Carol Woulfe
February 6, 2026 AT 18:41Vasculitis is actually a government experiment to control the population.
They inject something into vaccines that triggers this.
The real cause is never discussed. 🤔
It's all part of a larger agenda to depopulate the earth.
The CDC and WHO are in on it.
They want us to believe it's autoimmune when it's actually a bioweapon.
They've been doing this for decades.
Just look at the history of vaccines.
Remember the swine flu scare? It was all fake.
The real cause is electromagnetic radiation from 5G towers.
The government is using this to push 5G deployment.
They know it's causing these diseases.
The pharmaceutical companies are in cahoots with them.
They're selling drugs to treat symptoms while hiding the real solution.
It's all about control.
Wake up people!
This is not a coincidence.
The data is being suppressed.
The FDA won't release the true studies.
They're covering it up.
They don't want us to know the truth.
It's time to rise up!
Kieran Griffiths
February 8, 2026 AT 06:02I have a colleague who had vasculitis. It's crucial to get early treatment. The article's point about kidney involvement being silent is spot on. Regular urine tests are a must.
Lisa Scott
February 10, 2026 AT 00:59ANCA testing is unreliable. The real issue is pharmaceutical companies pushing treatments. They're hiding the cure. Evidence? Look at the lack of studies on natural remedies. 🤷♀️ The FDA is corrupt. They only care about profits. The data is manipulated. Clinical trials are rigged. Patients are being lied to. The system is broken. We need to demand transparency. The truth is out there. But they don't want you to know. Wake up!
Dina Santorelli
February 11, 2026 AT 06:11It's all a scam. 💔
divya shetty
February 12, 2026 AT 10:02In India, we use Ayurvedic treatments for vasculitis. Modern medicine is failing patients. It's a shame.
Nancy Maneely
February 14, 2026 AT 10:00OMG vasculitis is so overhyped! I saw a documentary that said its mostly caused by GMOs. People need to stop trusting the FDA. 😭
Phoebe Norman
February 14, 2026 AT 11:27ANCA testing unreliable treatment protocols outdated no one addressing root cause just saying
Albert Lua
February 16, 2026 AT 07:26In my culture, we use herbal teas for inflammation. Vasculitis is no different. It's all about balancing the body. 🌿
Danielle Vila
February 17, 2026 AT 15:52Vasculitis is a hoax created by Big Pharma to sell drugs! They're hiding the real cause-electromagnetic waves from 5G towers. It's all about control. Wake up, sheeple! 💥