Warfarin-TMP-SMX INR Risk Calculator
This tool estimates how much your INR might increase when taking trimethoprim-sulfamethoxazole (Bactrim/Septra) while on warfarin therapy. Based on clinical data from 70,000+ warfarin users.
Estimated INR Increase
1.8 points
Projected INR
4.3 (Current: 2.5)
Recommended Actions
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance - and sometimes, dangerously so. Trimethoprim-sulfamethoxazole, commonly sold as Bactrim or Septra, is one of the most notorious antibiotics for this exact problem. If you're taking warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, mixing it with this antibiotic can cause your INR to spike overnight. That’s not just a lab number change - it’s a real risk of internal bleeding, stroke, or worse.
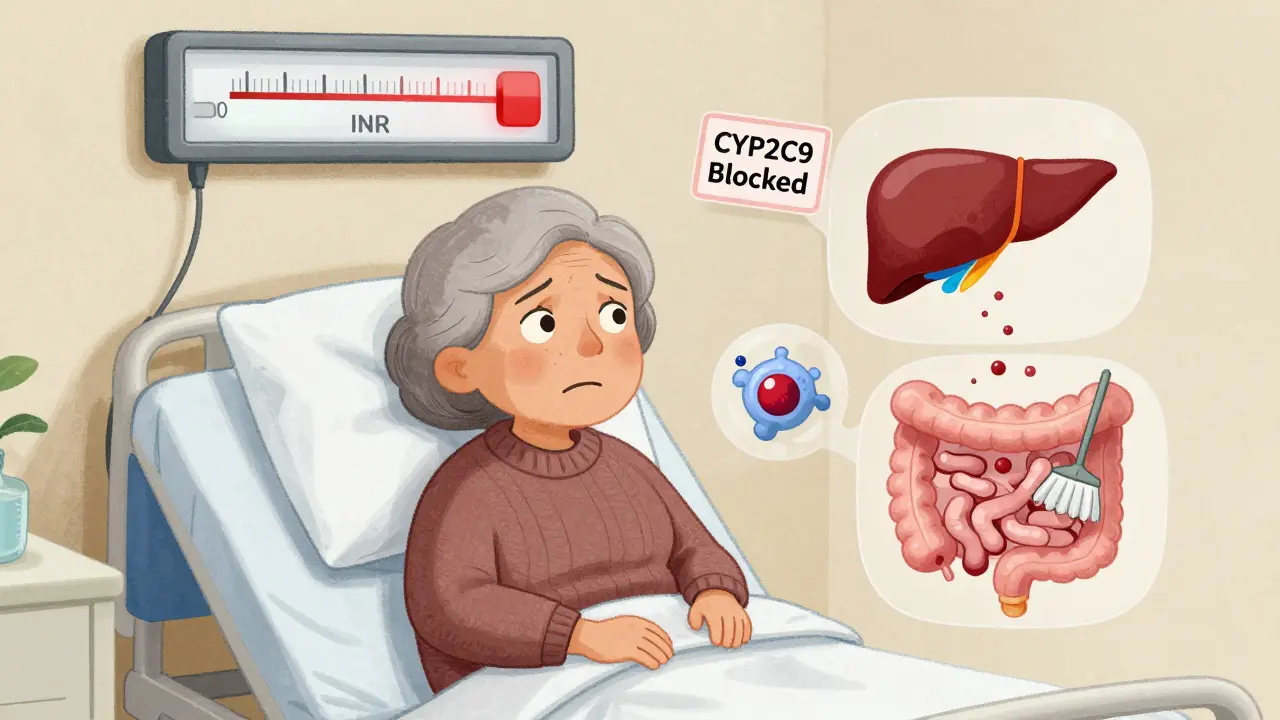
Why This Interaction Happens
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a delicate balance. Too little, and you bleed. Too much, and you clot. Trimethoprim-sulfamethoxazole doesn’t just fight bacteria - it interferes with warfarin in three key ways.First, trimethoprim slows down how fast your liver breaks down the stronger form of warfarin, called S-warfarin. This form makes up most of warfarin’s blood-thinning effect. When CYP2C9, the liver enzyme that processes it, gets inhibited, warfarin builds up in your system. Studies show this alone can raise INR by 0.5 to 1.0 units.
Second, sulfamethoxazole pushes warfarin off the proteins in your blood that normally hold it in check. Warfarin is 97-99% bound to albumin. When another drug like sulfamethoxazole - which is also highly protein-bound - shows up, it kicks warfarin loose. Now there’s more free warfarin circulating, and it’s actively thinning your blood.
Third, the antibiotic wipes out good bacteria in your gut that make vitamin K. Less vitamin K means warfarin works even harder. It’s like turning up the volume on a song you didn’t realize was already loud.
Together, these effects can push your INR from a safe 2.5 up to 6.0 or higher in just 2-3 days. That’s not theoretical. Real patients - elderly, frail, on long-term warfarin - have ended up in the ER with bleeding into their brains, guts, or joints because of this combo.
How Much Does INR Really Rise?
Not every patient sees the same spike. But the data is clear: this interaction is among the strongest of any antibiotic-warfarin pair.A study of over 70,000 warfarin users found that TMP-SMX raised INR by an average of 1.8 points. Compare that to amoxicillin, which barely moved the needle - only 0.4 points. Even ciprofloxacin, another common antibiotic, only bumped INR by about 0.9 points. TMP-SMX isn’t just a risk - it’s the highest-risk offender.
Some people are more vulnerable. If you’re over 75, have heart failure, liver disease, or poor nutrition, your INR can jump by 2.5 units or more. Men are slightly more likely to have a big spike than women - about 9% more risk, according to the same study. And if you’ve had a previous INR spike with antibiotics, you’re at higher risk again.
One nurse practitioner in Toronto told me about a case: a 79-year-old woman on warfarin for AFib got a UTI. She was prescribed Bactrim. Three days later, her INR hit 7.1. She didn’t bleed externally, but her hemoglobin dropped 3 points. She needed vitamin K and a hospital stay. She didn’t need to be hospitalized for the infection - but she did for the interaction.
What Happens When INR Goes Too High?
INR targets depend on why you’re on warfarin. For atrial fibrillation, it’s usually 2.0-3.0. For mechanical heart valves, it’s 2.5-3.5. Anything above 4.0 increases bleeding risk. Above 5.0? Risk jumps sharply. Above 10? It’s an emergency.Here’s what happens at different levels:
- INR 4.0-5.0: No bleeding? Hold 1-2 warfarin doses. Restart at 70-80% of your normal dose. Check INR in 2-3 days.
- INR 5.0-9.0 with minor bleeding: Give 1-2.5 mg of oral vitamin K. Monitor closely. Avoid IV unless needed.
- INR >10 or major bleeding: IV vitamin K (5-10 mg) + 4-factor prothrombin complex concentrate (PCC). Don’t wait for fresh frozen plasma - PCC works faster and safer.
Never just increase your warfarin dose to ‘fix’ a high INR. That’s like pouring gasoline on a fire. You’re not correcting the problem - you’re setting yourself up for the next crash.
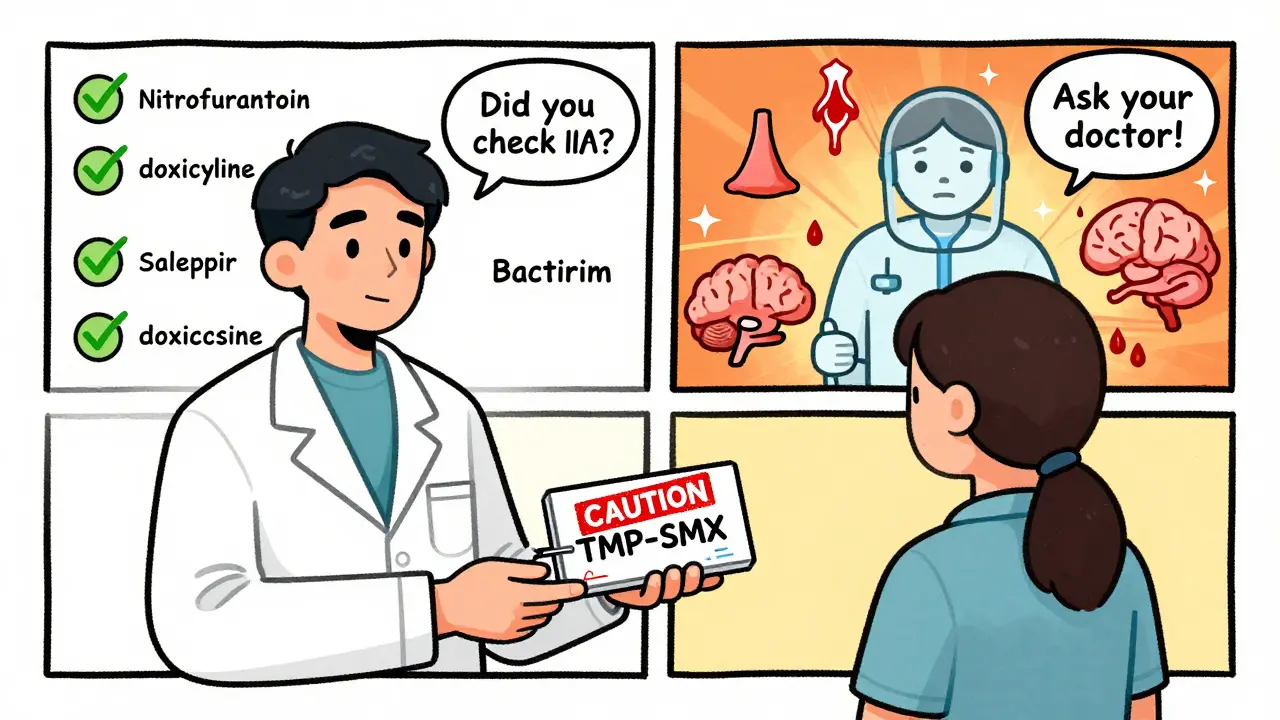
What Should You Do If You Need an Antibiotic?
The best advice? Avoid TMP-SMX entirely if you’re on warfarin. But sometimes, there’s no choice - say, for a severe urinary tract infection or pneumonia.Here’s what to do if you must use it:
- Check your INR before starting. Know your baseline.
- Test again within 48 hours. Don’t wait a week. The spike often hits fast.
- Reduce your warfarin dose by 20-30% preemptively. Especially if you’re older, frail, or have liver issues.
- Check INR every 3-4 days while on the antibiotic. Even if you feel fine.
- Ask your doctor about alternatives. Nitrofurantoin for UTIs? Usually safe. Doxycycline? Low risk. Amoxicillin? Very low risk.
Some pharmacists and doctors still prescribe Bactrim to warfarin patients without adjusting doses. That’s outdated. A 2022 study in JAMA Internal Medicine found nearly 1 in 5 warfarin patients got a risky antibiotic within 30 days - and TMP-SMX made up almost 30% of those cases. That’s not just a mistake - it’s preventable harm.
What About New Blood Thinners?
You might think, “I’ll just switch to Eliquis or Xarelto.” That’s a smart move - and many people should. Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t interact with TMP-SMX the same way. They’re not metabolized by CYP2C9, and they don’t rely on protein binding like warfarin does.But here’s the catch: not everyone can switch. People with mechanical heart valves still need warfarin - no DOAC is approved for them. And some patients with kidney failure, severe obesity, or history of clots can’t use DOACs safely. That means thousands of Canadians and Americans will keep taking warfarin for years to come.
The NIH just launched a $2.4 million study in 2023 to look at how these interactions affect older adults - because we’re aging, and warfarin isn’t going away anytime soon.
What Patients Say
Online forums are full of stories. On Reddit, someone wrote: “My dad’s INR hit 8.2 after Bactrim. They gave him vitamin K and plasma. He was scared to leave the hospital.” Another said: “I took Bactrim for a sinus infection and didn’t feel different. My INR stayed at 2.8. So I thought it was fine - until my doctor said I got lucky.”That’s the problem. Some people don’t react. But you can’t know who’s in that group until it’s too late. The FDA has over 1,800 reports of INR spikes linked to TMP-SMX over five years. Nearly half led to hospitalization. Nearly 4% were fatal.
Patients who got specific counseling about antibiotic risks had 37% fewer emergency visits for bleeding. That’s not a small number. It’s life-saving.
Bottom Line: Don’t Guess. Test.
This isn’t about being scared of antibiotics. It’s about being smart with your meds. If you’re on warfarin and your doctor says you need an antibiotic:- Ask: “Is this the safest option?”
- Ask: “Can we check my INR before and after?”
- Ask: “Should I hold my next warfarin dose?”
Don’t assume your pharmacist caught it. Don’t assume your doctor remembers your full med list. You’re the only one who knows your body. If you feel off - bruising easily, nosebleeds, dark stools, headaches - get your INR checked. Now.
This interaction is well-documented, predictable, and preventable. But it still happens - because people assume it won’t happen to them. It can. And it does.

Lydia H.
January 19, 2026 AT 23:09Wow, this is one of those posts that makes you realize how little most people know about their own meds. I’ve been on warfarin for five years and never realized Bactrim could do this - my doctor just said "take the antibiotic" and never mentioned INR checks. Scary stuff.
Jacob Hill
January 21, 2026 AT 18:36Exactly. I had a friend who ended up in the ER after a UTI and Bactrim - INR hit 8.9. No bleeding, but they had to give her vitamin K, plasma, and she missed two weeks of work. And the worst part? The pharmacist didn’t flag it either. We all assume someone else is checking. But no one is.
Lewis Yeaple
January 23, 2026 AT 14:46It is imperative to note that the pharmacokinetic interaction between trimethoprim-sulfamethoxazole and warfarin is mediated through multiple, synergistic pathways: inhibition of CYP2C9, displacement of albumin-bound warfarin, and gut microbiota depletion of vitamin K. These are not speculative mechanisms - they are empirically validated in peer-reviewed literature, including studies published in the Journal of Clinical Pharmacology and Thrombosis and Haemostasis. The clinical implications are not marginal; they are significant, predictable, and entirely avoidable with proper monitoring.
Jackson Doughart
January 24, 2026 AT 18:24I’ve seen this play out in clinic - elderly patients, often alone, prescribed Bactrim without a second thought. It’s not negligence, exactly. It’s just... inertia. The system moves fast, and the quiet risks get buried under the noise of daily practice. We need better alerts, better training, better habits. This isn’t about blame. It’s about design.
Malikah Rajap
January 25, 2026 AT 19:07Okay, but like… have you ever thought about how our bodies are just tiny ecosystems?? Like, your gut bacteria? They’re not just… there. They’re working for you! And when you wipe them out with antibiotics, you’re basically telling your liver, "Hey, no more vitamin K, so warfarin? Go wild." It’s like removing the brakes on a car while someone’s driving on ice. And then we wonder why people bleed out? It’s not magic. It’s biology. And we treat it like a footnote.
sujit paul
January 25, 2026 AT 23:56This is not an accident. This is a corporate conspiracy. Pharmaceutical companies know that warfarin is cheap and they profit from the constant monitoring, the ER visits, the hospitalizations. They push Bactrim because it creates recurring revenue. DOACs are expensive, yes - but they are also patented. Who benefits? Not you. Not your grandmother. The system is rigged. Wake up.
Tracy Howard
January 27, 2026 AT 11:17Canadians have been warning about this for decades. In the U.S., it’s still treated like some kind of medical mystery. We have national guidelines. We have pharmacovigilance programs. And yet - American doctors still prescribe Bactrim like it’s aspirin. It’s embarrassing. We don’t need more studies. We need accountability.
Astha Jain
January 28, 2026 AT 18:23so i took bactrim for my sinuses and my inr was fine?? maybe its just me?? or maybe i got lucky??
Phil Hillson
January 29, 2026 AT 14:34Another doctor post pretending they’re a hero when they just read a study. I’ve been on warfarin for 12 years and never had a problem with Bactrim. You’re all overreacting. My uncle died of a stroke from taking too much aspirin. Should we ban aspirin too? Stop fearmongering.
Josh Kenna
January 29, 2026 AT 19:53My mom got prescribed this combo last year and I didn’t catch it until her INR was 7.2. She was fine, but I was terrified. I started checking her INR every 3 days after that - even when she didn’t need to. Now she refuses Bactrim unless I’m in the room. I don’t care if it’s "overkill" - I’d rather be annoying than bury her.
Valerie DeLoach
January 30, 2026 AT 18:47Thank you for writing this. As a nurse who works with older adults, I’ve seen too many patients assume "it’s just a pill" - and then end up in the hospital because no one thought to ask about their meds. This isn’t just about warfarin. It’s about teaching people to be their own advocates. Ask questions. Demand checks. Bring a list. Write it down. And if someone says "it’s fine," ask them to prove it. Your life isn’t a gamble. It’s your responsibility - and your right.