Nurofen is one of the most recognizable pain relief brands in the world. But when you open your medicine cabinet, you’ll often see other options sitting right next to it: paracetamol, naproxen, aspirin, even topical gels. So what’s the real difference? And more importantly, which one should you reach for when your head hurts, your back aches, or your period cramps hit hard?
Nurofen’s active ingredient is ibuprofen - a nonsteroidal anti-inflammatory drug (NSAID). It doesn’t just mask pain. It cuts inflammation at the source. That’s why it works so well for sprains, arthritis, or menstrual pain. But ibuprofen isn’t the only player. Other painkillers have different strengths, risks, and ideal uses. Choosing the wrong one can mean less relief… or worse, side effects you didn’t expect.
How Nurofen (ibuprofen) actually works
Ibuprofen blocks enzymes called COX-1 and COX-2. These enzymes make prostaglandins - chemicals your body releases when injured or inflamed. Prostaglandins cause pain, swelling, and fever. By stopping their production, ibuprofen reduces all three. That’s why it’s more effective than plain paracetamol for swelling-related pain, like a swollen ankle or inflamed gums.
But here’s the catch: COX-1 also protects your stomach lining. When ibuprofen blocks it, you risk stomach upset, ulcers, or bleeding - especially if you take it on an empty stomach or use it long-term. That’s why Nurofen’s packaging warns against using it for more than 10 days without seeing a doctor.
For most healthy adults, a standard dose of 200 mg every 6-8 hours (no more than 1,200 mg in 24 hours) is safe. But if you’re over 65, have kidney issues, or take blood thinners, even that much can be risky.
Paracetamol (acetaminophen): The gentler option
If you’ve ever taken Tylenol or Panadol, you’ve used paracetamol. It’s the most common painkiller in the world. And unlike ibuprofen, it doesn’t touch inflammation. It works mainly in the brain to lower pain signals and reduce fever.
That makes it ideal for headaches, mild arthritis, or fevers - especially if you can’t take NSAIDs. People with stomach ulcers, asthma triggered by NSAIDs, or kidney disease often switch to paracetamol because it’s easier on the body.
But here’s the danger: paracetamol has a razor-thin safety margin. Taking just 10-15 extra tablets in one day can cause severe liver damage - sometimes fatal. The maximum daily dose for adults is 4,000 mg. But if you drink alcohol regularly, that number drops to 2,000 mg. Many cold and flu meds also contain paracetamol, so it’s easy to accidentally overdose.
Bottom line: Paracetamol is safer for your stomach and kidneys, but harder on your liver. Use it if you need fever control or mild pain without inflammation. Skip it if you drink alcohol daily or have liver disease.
Naproxen: The long-lasting alternative
Naproxen (sold as Aleve or Naprosyn) is another NSAID - like ibuprofen, but slower and longer-lasting. One tablet can work for up to 12 hours. That’s why it’s often recommended for chronic conditions like osteoarthritis or gout.
Studies show naproxen may carry a slightly lower risk of heart attack than ibuprofen, especially at higher doses. That’s why some doctors prefer it for people with heart disease risk factors. But it’s still an NSAID. It can cause stomach bleeding, kidney damage, and high blood pressure just like ibuprofen.
For acute pain like a toothache or muscle strain, naproxen might be overkill. But for all-day joint pain, it’s a solid pick. The standard dose is 220 mg every 8-12 hours. Don’t take it longer than 10 days without medical advice.
Aspirin: Not just for heart health
Aspirin is the oldest painkiller on this list. It’s an NSAID too, but it has one unique trick: it permanently blocks platelets from clumping. That’s why low-dose aspirin (75-100 mg daily) is used to prevent heart attacks and strokes.
For pain relief, you need a higher dose - usually 300-600 mg every 4-6 hours. But here’s the problem: aspirin increases bleeding risk more than ibuprofen or naproxen. It’s not safe for children under 16 due to Reye’s syndrome. It’s also risky if you have peptic ulcers, gout, or are pregnant.
Most people don’t use aspirin for routine headaches anymore. But if you’ve been prescribed low-dose aspirin for heart protection, don’t stop it without talking to your doctor - even if you’re taking ibuprofen for pain. Ibuprofen can interfere with aspirin’s heart-protective effect.
Topical pain relievers: Localized relief without the gut risk
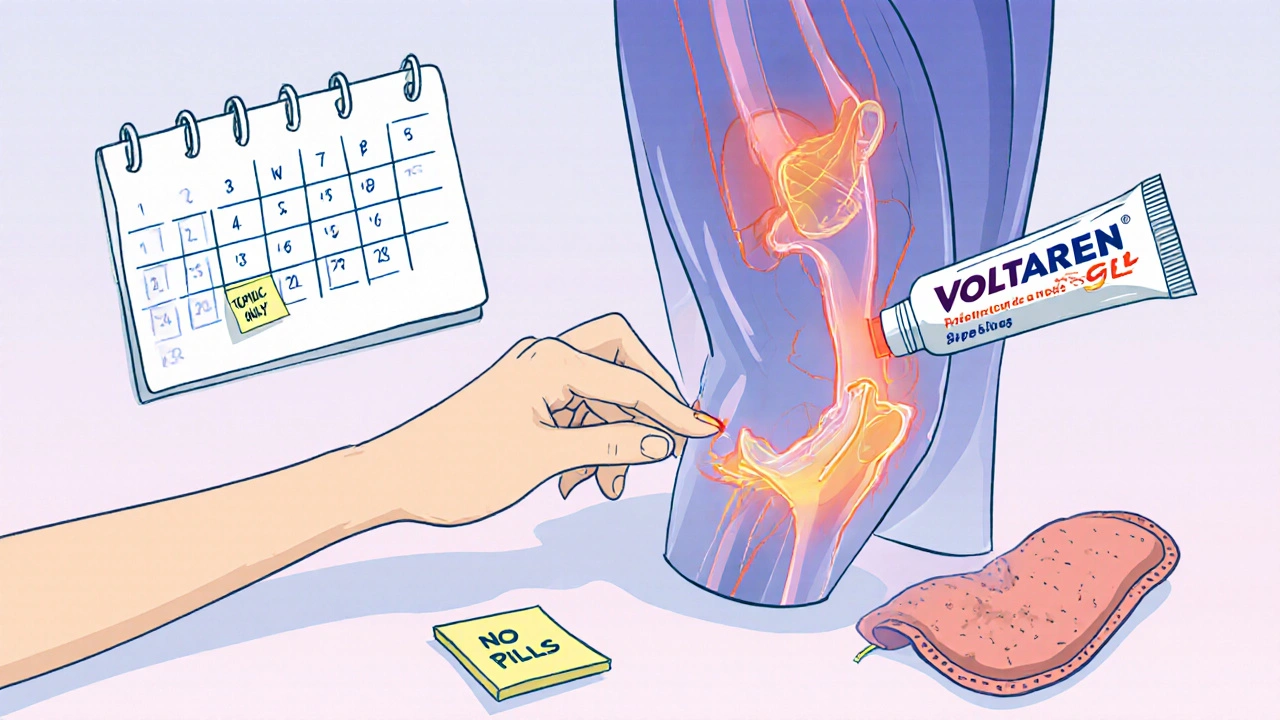
What if you don’t want to swallow anything? Topical gels and patches can deliver pain relief directly to the skin. Products like Voltaren Gel (diclofenac) or Bengay (menthol + camphor) work well for sore muscles, arthritis in the knees or hands, or minor sprains.
They bypass the digestive system entirely. That means far less risk of stomach upset or internal bleeding. But they’re not strong enough for full-body pain like migraines or period cramps. And they won’t reduce fever.
These are great as a supplement to oral meds - or as the first line of defense for localized pain. Just don’t use them on broken skin, and avoid combining them with heat wraps or heating pads. That can cause burns.
Who should avoid NSAIDs entirely?
Not everyone can take ibuprofen, naproxen, or aspirin. Avoid NSAIDs if you:
- Have a history of stomach ulcers or GI bleeding
- Have kidney disease or are on dialysis
- Have uncontrolled high blood pressure
- Are pregnant after 20 weeks (NSAIDs can affect fetal circulation)
- Have asthma worsened by painkillers
- Take blood thinners like warfarin or apixaban
- Are over 65 with multiple health conditions
If any of these apply to you, paracetamol is usually the safest starting point. But even then - check with your doctor or pharmacist. Some conditions require completely different treatments.
When to switch from Nurofen to something else
Here’s a simple rule: if Nurofen doesn’t help after two doses (about 12 hours), don’t keep taking more. You’re not getting stronger relief - you’re just increasing your risk.
Switch to paracetamol if:
- Your pain is mild and not linked to swelling
- You have stomach sensitivity
- You need something safe for short-term fever
Switch to naproxen if:
- Your pain lasts all day
- You have chronic joint pain
- You’re looking for longer-lasting relief
Try a topical gel if:
- Your pain is in one spot - knee, shoulder, wrist
- You want to avoid pills
- You’re already taking other medications that interact with NSAIDs
And if nothing works after 48 hours? See a doctor. Persistent pain isn’t normal. It could be a sign of something deeper - like an infection, nerve issue, or autoimmune condition.
Real-life examples: What works for what
Case 1: Sarah, 32, has a migraine. She takes Nurofen, but it only takes the edge off. She switches to paracetamol with caffeine (like Excedrin) - and gets full relief. Why? Migraines respond better to central pain relief than inflammation reduction.
Case 2: Raj, 58, has osteoarthritis in his knee. He used to take Nurofen daily. But his stomach started burning. His doctor switched him to naproxen once a day, plus a topical diclofenac gel. His pain is better, and his stomach is fine.
Case 3: Maria, 28, has period cramps. She used to take two Nurofen tablets every 6 hours. She started getting dizzy and nauseous. She switched to paracetamol with a heating pad. The cramps didn’t vanish, but the nausea did. She now uses a low-dose NSAID only on her heaviest days.
There’s no universal best painkiller. What works for one person can backfire for another.
What to look for on the label
Always check the active ingredient - not the brand name. Nurofen, Advil, Motrin, and generic ibuprofen all contain the same drug. But dosages vary. Some products combine ibuprofen with caffeine or antihistamines.
Look for:
- Active ingredient (e.g., ibuprofen 200 mg)
- Dosage instructions (how many pills, how often)
- Maximum daily dose
- Warnings (e.g., "Do not use if you have kidney disease")
- Expiration date
Never assume "natural" or "herbal" pain relievers are safer. Some can interact with prescription meds or cause liver damage. Stick to regulated pharmaceuticals unless your doctor approves otherwise.
Final tip: Don’t mix painkillers without checking
Many people think taking ibuprofen and paracetamol together is fine - and often it is. But only if you space them out. Don’t take them at the same time. Use one, wait 4-6 hours, then try the other. Keep a log of what you took and when.
And never combine NSAIDs. Taking ibuprofen and naproxen together doesn’t give you double the pain relief - it doubles your risk of bleeding and kidney damage.
Is Nurofen stronger than paracetamol?
Nurofen (ibuprofen) is stronger for pain caused by inflammation - like swollen joints, sprains, or period cramps. Paracetamol is better for fever and mild, non-inflammatory pain like headaches. Neither is universally "stronger." It depends on the cause of your pain.
Can I take Nurofen and paracetamol together?
Yes, you can take them together safely, but not at the same time. Space them 4-6 hours apart. For example, take ibuprofen at 8 a.m., paracetamol at 2 p.m., then ibuprofen again at 8 p.m. This gives you continuous relief without overdosing on either.
What’s the safest painkiller for long-term use?
No oral painkiller is truly safe for long-term daily use. But if you must take something regularly, paracetamol at the lowest effective dose (usually 650-1,000 mg up to four times a day) is the least risky for most people - as long as you don’t drink alcohol. Always talk to your doctor before using any painkiller daily for more than a few weeks.
Why does Nurofen sometimes make me feel sick?
Ibuprofen reduces protective stomach lining chemicals, which can lead to nausea, heartburn, or even ulcers. Taking it with food helps. If you feel sick often, switch to paracetamol or ask your doctor about a stomach-protecting medication like omeprazole.
Are there natural alternatives to Nurofen?
Some people find relief from turmeric, ginger, or omega-3s for mild inflammation. But these aren’t proven replacements for NSAIDs in moderate to severe pain. They work slowly, inconsistently, and may interact with blood thinners. Don’t use them instead of prescribed pain relief without medical advice.
What should I do if Nurofen doesn’t work?
If Nurofen doesn’t help after two doses (about 12 hours), stop taking it. Try paracetamol or a topical gel. If pain continues past 48 hours, or gets worse, see a doctor. Persistent pain could signal an infection, nerve issue, or other condition that needs different treatment.
If you're managing chronic pain, keep a simple log: what you took, when, how much, and how you felt 30 minutes later. Over time, you’ll spot patterns. You might discover that paracetamol works better for your headaches, while naproxen handles your back pain. The right painkiller isn’t about brand names - it’s about matching the drug to your body and your pain.

Jeff Moeller
November 19, 2025 AT 07:52ibuprofen ain't magic it's just chemistry
Tyrone Luton
November 21, 2025 AT 05:04you ever think about how we've turned pain into a consumer choice? like buying a new phone instead of fixing your spine? we treat discomfort like a software bug you just patch with pills. but the body ain't an app. it's a messy, ancient system that remembers every pill you ever swallowed. ibuprofen? it's just a bandaid on a broken bone you refuse to acknowledge.
we don't want to sit with pain. we want to erase it. and that's the real problem.
Herbert Scheffknecht
November 23, 2025 AT 02:29paracetamol is the silent assassin of the medicine cabinet. you think you're being safe but you're just slowly turning your liver into a brick. i used to take it like candy after nights out. then one morning i woke up with jaundice and a doctor telling me i had zero margin for error. no more casual dosing. no more "just one more". your liver doesn't care if you're a good person. it just counts the milligrams.
and don't get me started on combo meds. cold pills with acetaminophen? that's like hiding a grenade in a teddy bear. you don't even know you're holding it until it blows.
Sherri Naslund
November 23, 2025 AT 18:47you know who really profits from this? big pharma. they want you hooked on pills because pills are repeat customers. natural stuff? herbs? they can't patent turmeric. so they make you believe ibuprofen is the only way. but i've been taking ginger tea and cayenne rubs for years. my arthritis? gone. not cured. gone. and no liver damage. no stomach bleeding. just my grandma's old wisdom and a little patience.
they don't want you to know this. they want you buying bottles. not learning your body.
Bette Rivas
November 24, 2025 AT 18:16important clarification: naproxen's lower cardiovascular risk compared to ibuprofen is only observed in long-term, high-dose use for chronic conditions like osteoarthritis. for acute pain like a sprain, there's no meaningful difference in cardiac risk between the two. also, naproxen's longer half-life means it accumulates more in elderly patients or those with renal impairment - so while it may seem convenient to take once daily, it's not automatically safer. always consider renal function, age, and concurrent medications before switching.
topical diclofenac is underutilized. studies show it's as effective as oral NSAIDs for knee osteoarthritis with 90% less systemic exposure. but most people don't know how to use it properly - apply a 4g dose (about a strip the size of a finger) four times daily, and wait 30 minutes before covering with clothing. also, avoid sun exposure on treated areas - diclofenac can cause phototoxicity.
Lauren Hale
November 25, 2025 AT 18:28i used to be the person who took two nurofen at the first sign of a headache. then i started getting stomach cramps and dizziness. switched to paracetamol - still got the headache, but at least i wasn't throwing up. then i tried a heating pad and some deep breathing. guess what? the headache faded faster than when i took pills. not because of magic. because stress was the real trigger.
we're so quick to reach for a pill that we forget pain is often a signal. not a problem to be erased. sometimes your body's trying to tell you to rest. to drink water. to stop scrolling. to sit down. pills don't fix that. awareness does.
try this: next time you feel pain, wait 20 minutes. breathe. stretch. hydrate. then decide if you really need it. you might be surprised.
Greg Knight
November 26, 2025 AT 00:47look, i'm not a doctor but i've been managing chronic lower back pain for 8 years and here's what i learned: consistency beats intensity. taking one naproxen every 12 hours for three days straight? way better than three ibuprofen every 4 hours on a bad day. your body doesn't like spikes. it likes rhythm.
also - always pair oral meds with movement. even if it's just 10 minutes of walking. blood flow helps reduce inflammation better than any pill. i used to think rest was the answer. turns out, gentle motion is.
and yes, i use the diclofenac gel. but i don't use it with heat wraps. learned that the hard way. third-degree burn on my hip. not fun. don't be me.
keep a log. even if it's just a note on your phone. over time you'll see patterns. like how coffee makes your headaches worse. or how sleeping on your side kills your shoulders. pills help. but understanding your body? that's the real win.
rachna jafri
November 26, 2025 AT 10:24they tell you ibuprofen is safe but they don't tell you the truth - every time you take it, you're doing a little damage to your gut lining. it's like sandpaper on your insides. and no one talks about how the pharmaceutical industry funds the studies that say it's fine. who do you think pays for those "clinical trials"? corporations that profit when you keep buying bottles.
paracetamol? it's worse. your liver doesn't scream when it's dying. it just quietly shuts down while you're watching netflix. and they say "don't drink" but they don't say - even one beer a day cuts your safe limit in half.
they want you dependent. they don't want you healed. they want you buying.
and don't get me started on "natural" alternatives being dismissed. have you ever heard of boswellia? or curcumin with piperine? they work. just slower. because nature doesn't move on corporate timelines.
prasad gali
November 27, 2025 AT 17:48the data is clear: NSAIDs carry a class-wide risk of acute kidney injury, especially in volume-depleted states. dehydration + ibuprofen = renal vasoconstriction. simple pharmacokinetics. yet people take it before workouts or in hot weather like it's water. this isn't anecdotal - it's in the FDA's adverse event reporting system. every year, thousands end up in ERs because they thought "it's just a pill."
and the aspirin-cardio interaction? that's not a myth. ibuprofen competes with aspirin for the COX-1 binding site. if you take them within 8 hours, you neutralize aspirin's antiplatelet effect. this is documented in the New England Journal of Medicine. yet pharmacists still sell them side by side. negligence.
if you're over 50 and on daily aspirin for cardiac protection, never take ibuprofen without spacing it 2+ hours apart. and if you're unsure? ask for a pharmacist consult. they're trained for this. not just to ring you up.
darnell hunter
November 27, 2025 AT 18:48the assertion that "paracetamol is safer for the stomach" is statistically accurate but clinically misleading. while it lacks direct gastric mucosal toxicity, its hepatic metabolism generates NAPQI, a reactive metabolite that depletes glutathione. in individuals with low glutathione reserves - alcoholics, malnourished, elderly - this creates a high-risk scenario for fulminant hepatic failure. the 4g/day limit is arbitrary and not physiologically grounded. individual variability in CYP2E1 activity means some patients reach toxic thresholds at 2.5g/day.
furthermore, the widespread inclusion of acetaminophen in OTC combination products creates a significant public health blind spot. the CDC estimates that 40% of acute liver failure cases in the U.S. are attributable to unintentional overdose from polypharmacy. this is not a failure of individual judgment - it is a failure of regulatory oversight and product labeling.
recommendation: cease use of all combination analgesics. insist on single-ingredient formulations. and never assume "natural" means safe. ephedra, comfrey, and kava have all been banned for similar reasons.
Martin Rodrigue
November 28, 2025 AT 15:30the notion that topical NSAIDs are "safer" is only partially true. while systemic absorption is reduced, local irritation, allergic contact dermatitis, and photosensitivity reactions occur in up to 5% of users. diclofenac gel, in particular, has been associated with rare but severe cutaneous reactions including Stevens-Johnson syndrome. furthermore, the efficacy of topical agents is highly dependent on skin integrity, application technique, and the anatomical site. The knee and hand respond well; the lumbar spine does not. Patients should be counseled accordingly.
Additionally, the claim that "topical gels bypass the digestive system entirely" is pharmacologically inaccurate. While oral bioavailability is avoided, dermal absorption still leads to systemic circulation. Plasma concentrations of diclofenac from topical gel reach approximately 5-10% of oral levels - sufficient to exert pharmacological effects and potential adverse events in susceptible individuals.
Therefore, while topical NSAIDs represent a valuable therapeutic option, they are not risk-free and should be considered as adjuncts, not replacements, for systemic therapy when indicated.
Ashley Miller
November 29, 2025 AT 03:58you ever wonder why nurofen is everywhere but no one talks about the fact that ibuprofen was originally developed for the military? they needed soldiers to keep fighting through pain. so they made a drug that masks pain without fixing the cause. now it's in every drugstore like it's a vitamin. but they didn't want you to know it was designed to keep you broken but functional.
they don't want you healing. they want you medicated. always. forever. buying. swallowing. waiting for the next bottle.
the real painkiller? awareness. rest. silence. food that isn't processed. and asking why we're all so damn broken in the first place.
Hannah Machiorlete
November 30, 2025 AT 01:24i took ibuprofen for a week straight for my period cramps. ended up in the ER with gastritis. the nurse asked if i knew it was an NSAID. i said "yeah but it's just nurofen." she laughed and said "it's basically battery acid for your stomach." now i use heat packs and chamomile tea. yeah it's slower. but i'm not puking bile anymore.
also - why do people mix paracetamol and ibuprofen like it's a cocktail? i did that once. woke up with my liver screaming. now i stick to one. and only if i really need it.
Paige Basford
December 1, 2025 AT 21:03my mom took naproxen for 10 years for her arthritis. then one day she got a stomach bleed and almost died. they told her it was "just the price of pain relief." i don't buy it. why wasn't she on a proton pump inhibitor? why wasn't she monitored? why did no one warn her about the long-term risks? because pills are easier than care.
we treat pain like a problem to be solved with a bottle. not a signal to be understood. we're so busy trying to feel nothing that we forget how to feel at all.
Jessica Engelhardt
December 2, 2025 AT 12:06you think americans are the only ones overmedicated? try living in canada. we get the same pills but they charge us 3x more. and then they tell us to "be responsible." like we're not being sold poison in pretty bottles. the whole system is rigged. big pharma owns the doctors, the labels, the ads. they don't care if you live or die - they care if you keep buying.
and don't even get me started on "natural" being dismissed. my cousin in india uses turmeric paste and gets better than half the people on pills. but no, we're too "advanced" for that. right.
Lauren Hale
December 2, 2025 AT 21:02just wanted to add - if you're taking any of these daily for more than a week, talk to your doctor. not a pharmacist. not a Google search. a real human who knows your history. because pain isn't a one-size-fits-all problem. it's your body speaking. listen before you swallow.