When you take two medications together, you might not think about your muscles. But some combinations can cause your muscle tissue to literally start breaking down - a condition called rhabdomyolysis. It’s rare, but when it happens, it can land you in the hospital, damage your kidneys, or even be fatal. And the scariest part? Many people don’t know they’re at risk until it’s too late.
What Happens When Muscles Break Down
Rhabdomyolysis isn’t just soreness after a tough workout. It’s a medical emergency where muscle cells die and spill their contents into your bloodstream. The main culprit? A protein called myoglobin. Normally, it helps muscles store oxygen. But when it floods your blood from damaged tissue, your kidneys try to filter it out - and get overwhelmed. That’s when kidney failure kicks in.Most people think of rhabdomyolysis as something that happens after extreme exercise or trauma. But in reality, up to 10% of cases come from medications - and nearly all of those are caused by drug interactions. Statins, the cholesterol-lowering drugs millions take daily, are responsible for about 60% of medication-related cases. But it’s not the statin alone. It’s what you take with it.
The Most Dangerous Drug Combos
Some drug pairs are ticking time bombs. Here are the worst offenders, backed by real clinical data:- Simvastatin + Gemfibrozil: This combo increases rhabdomyolysis risk by 15 to 20 times compared to statin alone. Gemfibrozil blocks the enzyme that clears simvastatin from your body, letting it build up to toxic levels.
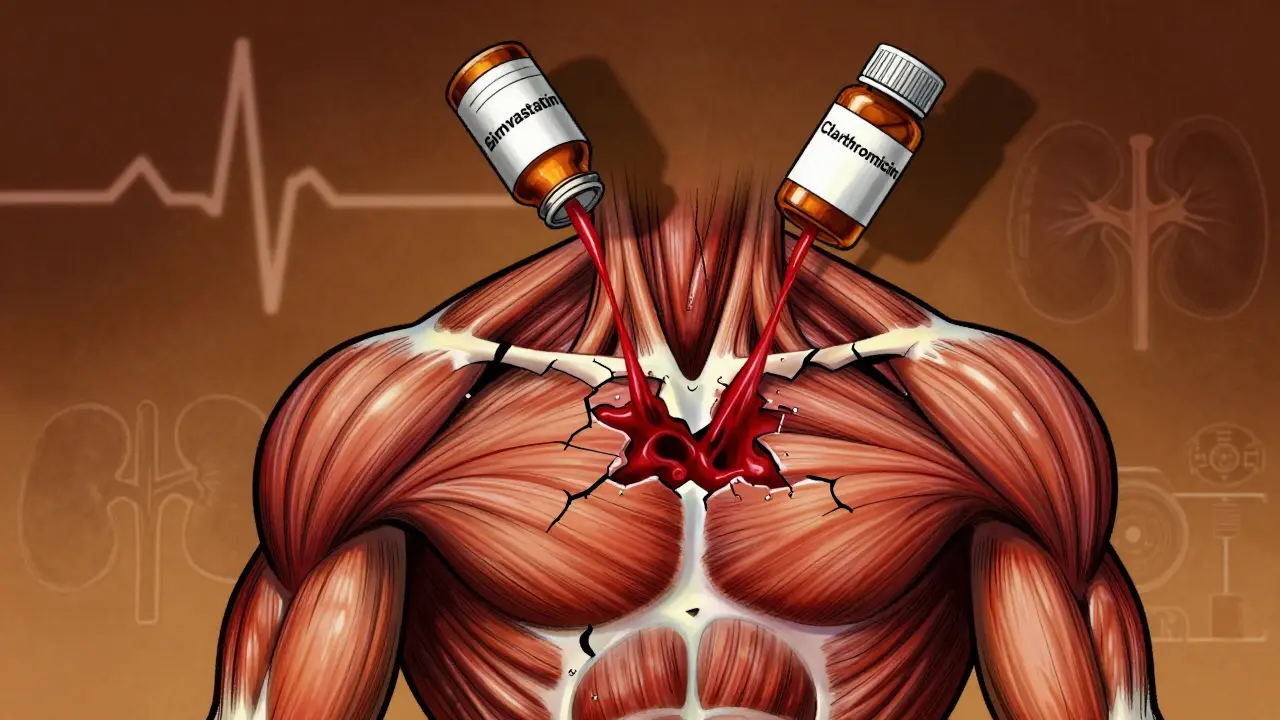
- Simvastatin + Erythromycin or Clarithromycin: These antibiotics inhibit CYP3A4, the liver enzyme that breaks down simvastatin. One study found this interaction raises risk by 18.7-fold.
- Colchicine + Clarithromycin: Used for gout, colchicine becomes deadly when paired with this antibiotic. The European Medicines Agency reported a 14.2-fold spike in cases.
- Erlotinib + Simvastatin: This cancer drug and statin combo has caused CK levels over 20,000 U/L in under 72 hours - enough to trigger dialysis.
- Propofol + Long-term ICU use: Though rare, this anesthesia drug can cause mitochondrial failure in muscle cells, leading to one of the deadliest forms of rhabdomyolysis with 68% mortality when it occurs.
These aren’t theoretical risks. Real patients have posted about them. One user on Mayo Clinic’s forum wrote: “After adding clarithromycin to my colchicine for gout, my urine turned cola-colored within 48 hours and CK hit 28,500 U/L.” Another said: “My oncologist didn’t warn me about the simvastatin-erlotinib interaction - CK peaked at 42,000 and I needed 3 days of dialysis.”
Who’s Most at Risk?
Not everyone who takes these drugs will have problems. But certain people are far more vulnerable:- People over 65: Risk is 3.2 times higher than in younger adults.
- Women: They’re 1.7 times more likely than men to develop drug-induced rhabdomyolysis.
- Those with kidney problems: If your eGFR is below 60, your risk jumps 4.5 times.
- People on five or more medications: Polypharmacy raises risk by 17.3 times. The more pills you take, the higher the chance of a hidden interaction.
- Those with the SLCO1B1*5 gene variant: This genetic quirk - common in Europeans - makes simvastatin 4.5 times more likely to cause muscle damage.
And here’s the problem: many doctors don’t screen for these risks. A Reddit thread analyzing 147 statin-related rhabdomyolysis cases found that 92% of patients said their provider never mentioned the danger of interactions.
What Are the Warning Signs?
The classic triad - muscle pain, weakness, and dark urine - only shows up in about half the cases. That’s why so many people miss it.Other red flags include:
- Unexplained muscle soreness that doesn’t go away
- Dark brown or tea-colored urine
- Nausea, vomiting, or fever without infection
- Swelling or tightness in arms or legs
- Feeling unusually tired, even after rest
CK levels - a blood test measuring muscle damage - are the diagnostic key. Normal levels are under 200 U/L. Anything over 1,000 U/L is a warning. Severe cases often hit 5,000 to 100,000 U/L. If your CK is above 5,000 and you’re on a high-risk combo, you need urgent care.
How Doctors Treat It
The moment rhabdomyolysis is suspected, the first step is stopping the offending drug. Then, aggressive hydration kicks in.The Cleveland Clinic’s protocol for moderate to severe cases is:
- 3 liters of IV saline in the first 6 hours
- Then 1.5 liters per hour to keep urine output above 200-300 mL/hour
- Add sodium bicarbonate to keep urine pH above 6.5 - this prevents myoglobin from clogging kidney tubules
Some patients need dialysis. Others develop dangerous electrolyte imbalances: high potassium (which can cause cardiac arrest) or low calcium (which leads to muscle spasms and seizures). About 5% of severe cases develop compartment syndrome - where swollen muscles cut off blood flow, requiring emergency surgery.
For rare cases like leflunomide-induced rhabdomyolysis (from an arthritis drug), plasma exchange may be needed. Why? Because leflunomide sticks around in your body for weeks. You can’t just stop it and wait.
What Happens After Recovery?
Survivors aren’t out of the woods. A 10-year Mayo Clinic study found that 43.7% still had muscle weakness six months later. Recovery takes time:- Without kidney damage: 12.3 weeks on average
- With dialysis: 28.6 weeks on average
And it’s not just physical. Many patients report lasting anxiety about taking any new medication. One patient told researchers: “I used to think statins were safe. Now I’m scared every time I get a prescription.”
How to Protect Yourself
You don’t need to avoid all medications. But you do need to be smarter about them:- Ask your doctor: “Could this new drug interact with anything I’m already taking?”
- Know your statin: Simvastatin and lovastatin are the riskiest. Atorvastatin and pravastatin are safer with most drugs.
- Avoid grapefruit juice with statins - it blocks the same enzyme as antibiotics.
- Use a medication list: Keep a printed or digital list of every pill, supplement, and OTC drug you take. Bring it to every appointment.
- Watch for early signs: If your muscles feel unusually sore after starting a new drug, get a CK test. Don’t wait for dark urine.
- Ask about genetic testing: If you’re on high-dose simvastatin and have family history of muscle problems, SLCO1B1 testing might be worth it.
Regulators are catching up. The EMA now requires all statin labels to list specific CYP3A4 inhibitors as contraindications. The FDA’s Sentinel system is tracking new risks - like the 22.4% spike in rhabdomyolysis reports after remdesivir was introduced for COVID-19.
The Bigger Picture
Rhabdomyolysis from drug interactions isn’t just a medical oddity. It’s a symptom of a broken system. We give people more and more pills without checking how they work together. We assume patients will read the fine print. We assume doctors remember every interaction.But the numbers don’t lie. Over 27,000 Americans are hospitalized each year for this. The average cost? Nearly $29,000 per admission. And the trend is rising - with polypharmacy growing, incidence could increase 8.2% per year through 2030.
The solution isn’t to stop taking meds. It’s to take them smarter. Ask questions. Demand clarity. Know your risks. Because your muscles aren’t just tired - they’re telling you something’s wrong.
Can rhabdomyolysis happen from one medication, or only from interactions?
Rhabdomyolysis can happen from a single drug - especially high-dose statins, colchicine, or antivirals like zidovudine. But the most dangerous and common cases involve interactions. About 89% of fatal cases occur when a statin is combined with another drug that blocks its metabolism, like certain antibiotics or antifungals. So while one drug can cause it, two together are far more likely to trigger a crisis.
Is it safe to take statins with ibuprofen or acetaminophen?
Yes, ibuprofen and acetaminophen are generally safe with statins. They don’t interfere with the liver enzymes (CYP3A4) that break down statins. But if you’re taking high doses of NSAIDs like ibuprofen long-term, they can stress your kidneys - which adds another layer of risk if rhabdomyolysis develops. Always check with your pharmacist if you’re on multiple medications, even common ones.
How long after starting a new drug does rhabdomyolysis usually appear?
Most cases show up within 30 days of starting a new medication or changing a dose. Statin-related cases typically appear around 28 days after beginning treatment. But in high-risk combos - like simvastatin with clarithromycin - symptoms can hit in as little as 48 hours. That’s why it’s critical to monitor for muscle pain or dark urine right after starting a new drug.
Can I check my CK levels at home?
No, CK levels require a blood test done in a lab or hospital. There are no reliable at-home tests for muscle breakdown. If you suspect rhabdomyolysis - especially if you’re on a high-risk drug combo - go to an urgent care or ER. Don’t wait. Early detection can prevent kidney failure.
Are there any natural supplements that increase rhabdomyolysis risk?
Yes. Some supplements can be dangerous with medications. Red yeast rice contains natural statins and can cause rhabdomyolysis on its own - especially when taken with prescription statins. High-dose niacin (vitamin B3) can also increase muscle damage risk. Creatine is generally safe, but if you’re dehydrated or have kidney issues, it may add stress. Always tell your doctor what supplements you take - they’re not harmless.
If I had rhabdomyolysis once, can I ever take statins again?
It depends. Many people can safely restart statins after recovery - but not the same one. Switching to pravastatin or fluvastatin, which aren’t metabolized by CYP3A4, lowers the risk of recurrence. Some doctors may also prescribe a much lower dose with strict monitoring. Genetic testing for SLCO1B1*5 can help guide the decision. Never restart a statin without talking to your doctor and getting baseline CK levels checked.
Sally Dalton
January 26, 2026 AT 09:11OMG I had no idea grapefruit juice was a no-go with statins 😱 I’ve been drinking it every morning for years with my simvastatin… time to switch to orange juice ASAP.
Geoff Miskinis
January 27, 2026 AT 01:53Let’s be real - this isn’t about ‘drug interactions,’ it’s about pharmaceutical companies prioritizing profit over patient safety. The CYP3A4 inhibition data has been public since the 90s, yet we still see these combos prescribed like they’re harmless. It’s institutional negligence dressed up as ‘clinical practice.’
The FDA’s Sentinel system? A PR stunt. Real pharmacovigilance would require mandatory EHR integration of interaction alerts - not passive reporting.
And don’t get me started on ‘natural supplements.’ Red yeast rice is literally a statin. Selling it as ‘natural’ is predatory. The FTC should shut down those Amazon sellers.
Meanwhile, patients are left to self-educate via Reddit threads because their doctors are too rushed to check a drug interaction database. This isn’t medicine. It’s triage capitalism.
eric fert
January 27, 2026 AT 23:36Okay, so let me get this straight - we’re telling people that taking a statin with an antibiotic might kill them, but we’re fine with prescribing 7 different meds to an 82-year-old with 5 chronic conditions? That’s not medicine, that’s Russian roulette with a prescription pad.
And the fact that 92% of patients said their doctor never warned them? That’s not ignorance. That’s malpractice by omission. If your doctor can’t remember the top 5 dangerous combos, they shouldn’t be writing scripts.
Also, ‘CK over 20,000’? That’s not a lab result - that’s a death sentence waiting to happen. And yet, we still let people walk out of the ER with a ‘follow-up in 2 weeks’ after a 42,000 CK? What the actual f.
And don’t even get me started on the ‘genetic testing’ suggestion. You want people to pay $500 for a gene test so they can be told ‘sorry, you’re a walking time bomb’? That’s not prevention. That’s financial exploitation with a side of fear.
Meanwhile, the real solution? Stop prescribing so many damn pills. But that would require doctors to think - and we all know how much that costs.
Napoleon Huere
January 28, 2026 AT 13:25There’s something deeply human here - we treat our bodies like machines that can be fine-tuned with pills, but we forget they’re living systems with cascading vulnerabilities.
Rhabdomyolysis isn’t just a biochemical accident. It’s a metaphor for our medical system: fragmented, reactive, and blind to the interconnectedness of things.
We give you a statin to fix cholesterol, an antibiotic to fix an infection, a painkiller to fix inflammation, a diuretic to fix fluid, and a sleep aid to fix the stress from all the above - and then we’re shocked when your muscles start dissolving.
Maybe the real question isn’t ‘which drugs interact?’ but ‘why are we giving so many drugs at all?’
There’s a philosophy here: if healing is about restoring balance, then piling on chemicals is the opposite of healing. It’s domination.
And yet, we call this progress.
Aishah Bango
January 30, 2026 AT 06:26People need to stop being so lazy about their health. If you’re on five medications, you should be reading the pamphlets, not just trusting your doctor. This isn’t rocket science - it’s basic responsibility.
And if you’re taking red yeast rice because you think it’s ‘natural,’ you’re not being healthy - you’re being stupid. Natural doesn’t mean safe. Poison ivy is natural too.
Stop acting like your doctor is your babysitter. You’re an adult. Know what you’re putting in your body.
Faisal Mohamed
January 30, 2026 AT 20:59Bro… the SLCO1B1*5 variant is like a genetic landmine. If you’re European and on simvastatin, you’re basically playing Russian roulette with your myocytes 🤡
And the fact that 14.2x spike with colchicine + clarithromycin? That’s not a side effect - that’s a homicide waiting to happen. EMA should’ve blacklisted that combo years ago.
Also, propofol in ICU? That’s not ‘rare.’ That’s ‘silent killer.’ We’re putting people in chemically induced comas and calling it care. The mitochondria don’t care if you’re ‘stable.’
And don’t even get me started on the ‘dialysis for 3 days’ cases. We’re not treating disease. We’re managing failure.
Also, emojis are the new medical alert system. 🚨
SWAPNIL SIDAM
February 1, 2026 AT 19:19This is very important. Many people in India take statins with antibiotics for infections. No one tells them about this risk. I hope doctors here start warning patients.
My uncle had muscle pain after taking statin and azithromycin. He thought it was just tiredness. He didn’t go to hospital until he couldn’t walk. Now he uses pravastatin. Thank you for this post.
Betty Bomber
February 2, 2026 AT 08:58I’m just here to say I didn’t know any of this. I’ve been on simvastatin for 8 years with no issues, but now I’m terrified to take anything new. I’m gonna make a list of all my meds and bring it to my next appointment. Thanks for the wake-up call.
Shawn Raja
February 3, 2026 AT 17:27So let me get this straight - we’ve got a system where your muscles can melt if you take two common pills together… and the solution is to ‘ask your doctor’?
Bro, your doctor has 8 minutes per patient and is on a 12-hour shift. They’re not reading the interaction tables. They’re clicking ‘yes’ to the EHR pop-up that says ‘continue?’
The real hero here? The pharmacist. The one who actually reads the damn script. But they’re the last line of defense - and they’re underpaid, overworked, and ignored.
Next time you get a new prescription, walk over to the pharmacy counter. Ask the pharmacist: ‘Is this gonna kill me with my other meds?’
And if they say ‘no,’ ask again. Because if they’re not sweating a little, they’re not doing their job.
Ryan W
February 3, 2026 AT 22:56Why are we even talking about this? The problem is not drug interactions - it’s the fact that Americans are overweight, sedentary, and medicated to the gills. Fix the root cause: stop eating junk, start moving. Then you won’t need 7 pills.
And if you’re too lazy to do that, don’t blame the system. Blame yourself.
Dan Nichols
February 5, 2026 AT 20:46People think rhabdomyolysis is rare so they ignore it - but it’s not rare if you’re on simvastatin + clarithromycin. That’s like driving drunk and saying ‘accidents are rare’
And the genetic thing? SLCO1B1*5 is basically a death sentence if you’re on simvastatin and you don’t know it
Doctors are lazy. They don’t test. They don’t warn. They just prescribe
And now you’re telling me I need to pay for a gene test? No thanks. I’ll just stop taking statins altogether
Renia Pyles
February 7, 2026 AT 19:24Ugh I HATE when people act like this is some new revelation. I’ve been screaming about this since 2018. My mom almost died from this exact combo. No one listens. Doctors act like they’re doing you a favor by prescribing. They’re not. They’re just checking boxes.
And don’t even get me started on ‘natural supplements.’ Red yeast rice? That’s not ‘natural’ - it’s illegal statin. The FDA should ban those sellers. They’re murderers in yoga pants.
I’m done being polite. This system is killing people and everyone’s too scared to say it.
Rakesh Kakkad
February 9, 2026 AT 10:20It is imperative that patients be informed regarding the potential for pharmacokinetic interactions. The prevalence of polypharmacy in geriatric populations necessitates a systematic approach to medication reconciliation. The absence of standardized protocols in primary care is a critical gap in patient safety.
Furthermore, the SLCO1B1*5 polymorphism exhibits a significant odds ratio for statin-induced myopathy, particularly with simvastatin. Genetic screening should be considered in high-risk cohorts.
It is also noteworthy that propofol infusion syndrome, though rare, carries a mortality rate of 68% - a figure that demands immediate clinical attention.
Nicholas Miter
February 10, 2026 AT 08:15I’ve been a nurse for 15 years and I’ve seen this happen way too often. A patient comes in with muscle pain, says ‘it’s just from working out,’ but they just started clarithromycin last week. We run the CK - 32,000. They’re in the ICU by midnight.
Most patients don’t even know what a statin is. They just take the pill because the doctor said so. We need better education - not just for patients, but for the whole medical team.
And honestly? The best thing you can do? Keep a list. Write down every pill, every supplement, every tea you drink. Bring it to every appointment. Even if your doctor doesn’t ask, show it to them. You’re your own best advocate.
Suresh Kumar Govindan
February 12, 2026 AT 05:14This is a controlled demolition of the pharmaceutical-industrial complex. The data is clear: drug interactions are weaponized negligence. The FDA’s passive surveillance is a farce. The genetic risk is suppressed. The system is designed to profit from crisis, not prevent it.
Those who survive are not lucky - they are outliers in a system engineered for mass harm.
And the real conspiracy? No one in power wants you to know how easily your body can be destroyed by two pills you bought at CVS.
Geoff Miskinis
February 12, 2026 AT 07:25Response to @7160: Grapefruit juice isn’t the only offender - pomegranate, Seville oranges, and even starfruit can do the same thing. And no, ‘organic’ grapefruit doesn’t help. It’s the furanocoumarins - same chemicals, same danger.
And @7165: You’re right about pharmacists. But most pharmacies now use automated systems that only flag ‘absolute contraindications.’ The 15-fold risk combos? They get buried under 200 ‘low-risk’ alerts. The system is broken - not the people.
Napoleon Huere
February 13, 2026 AT 11:11Response to @7180: Responsibility isn’t about blame. It’s about empowerment. But when the system doesn’t give you the tools - when your doctor doesn’t warn you, when the label doesn’t say ‘this could kill you,’ and when the pharmacy doesn’t flag it - then responsibility becomes a luxury.
Blaming the patient for not reading the 47-page insert they were handed at 7 a.m. after a 3-hour wait is not accountability. It’s cruelty.
Real responsibility means the system protects you - even when you’re exhausted, overwhelmed, and trusting the people who swore to help.