Switching from brand-name phenytoin to a generic version might seem like a simple cost-saving move-but for patients with epilepsy, it can be a quiet risk. Phenytoin isn’t like most medications. Even small changes in blood levels can lead to breakthrough seizures or dangerous toxicity. And because of how it behaves in the body, phenytoin demands careful monitoring, especially when generics are involved.
Why Phenytoin Is Different
Phenytoin has been used since the 1930s to control seizures, and it still works. But its pharmacology is tricky. It has a narrow therapeutic window: the effective range is only 10 to 20 mcg/mL. Go below that, and seizures can return. Go above it, and you risk confusion, loss of coordination, or even coma. What makes it worse is its non-linear pharmacokinetics. If you increase the dose by 25-50 mg, the blood level might jump by 50% or more. That’s not how most drugs work. For most, doubling the dose doubles the level. With phenytoin, the system gets saturated. It can’t process the extra drug efficiently, so levels spike unpredictably. Add to that: phenytoin is 90-95% bound to proteins in the blood. Only the tiny unbound portion (about 10%) actually works to stop seizures. If a patient has low albumin-common in older adults, liver disease, or malnutrition-the amount of free, active drug can rise even if the total level looks normal.Generic Substitutions: The Hidden Risk
The FDA says generic drugs are bioequivalent to brand-name versions. That means their absorption (AUC) and peak concentration (Cmax) must fall within 80-125% of the original. Sounds fine, right? Not for phenytoin. That 25% variability window is too wide for a drug with a narrow therapeutic index. A patient stable on 300 mg daily of Dilantin might switch to a generic and suddenly hit 22 mcg/mL-above the safe range-without any dose change. Or they might drop to 8 mcg/mL and start having seizures again. Studies show that switching between different generic brands can cause similar swings. One patient might tolerate Generic A fine but react badly to Generic B, even though both are "FDA-approved." The excipients-fillers, dyes, binders-can affect how quickly the drug dissolves and gets absorbed. For phenytoin, that’s enough to change outcomes.When to Monitor Levels
You don’t need to check phenytoin levels every month. But you absolutely must check them after:- Starting phenytoin for the first time
- Changing the dose
- Switching from brand to generic, or between generic brands
- Starting or stopping another medication
- Signs of toxicity (nystagmus, dizziness, slurred speech)
- Signs of underdosing (new or worsening seizures)
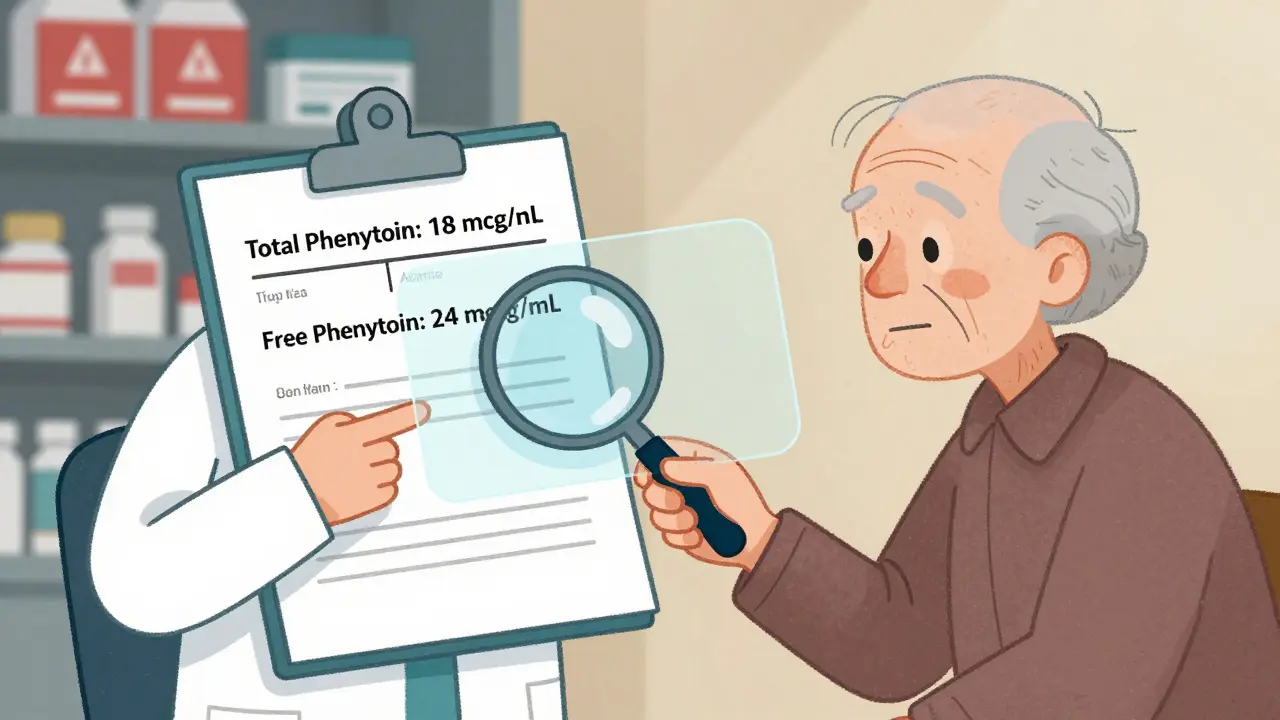
How to Interpret the Results
Most labs report total phenytoin levels. But if a patient has low albumin-say, below 3.5 g/dL-that number can be misleading. Use this formula to estimate the corrected level:Corrected phenytoin = Measured level ÷ [(0.9 × albumin ÷ 42) + 0.1]
But here’s the catch: this is just an estimate. It’s based on population averages. If a patient is critically ill, has kidney failure, or is on multiple interacting drugs, the formula may not reflect reality. In those cases, measure the free phenytoin level directly. It’s more accurate and tells you what’s actually active in the brain.Drug Interactions That Change Everything
Phenytoin is metabolized by liver enzymes (CYP2C9 and CYP2C19). Many common drugs interfere with those enzymes:- Increase phenytoin levels: Amiodarone, fluconazole, cimetidine, metronidazole, valproate, sulfonamides
- Decrease phenytoin levels: Rifampin, carbamazepine, phenobarbital, alcohol, theophylline
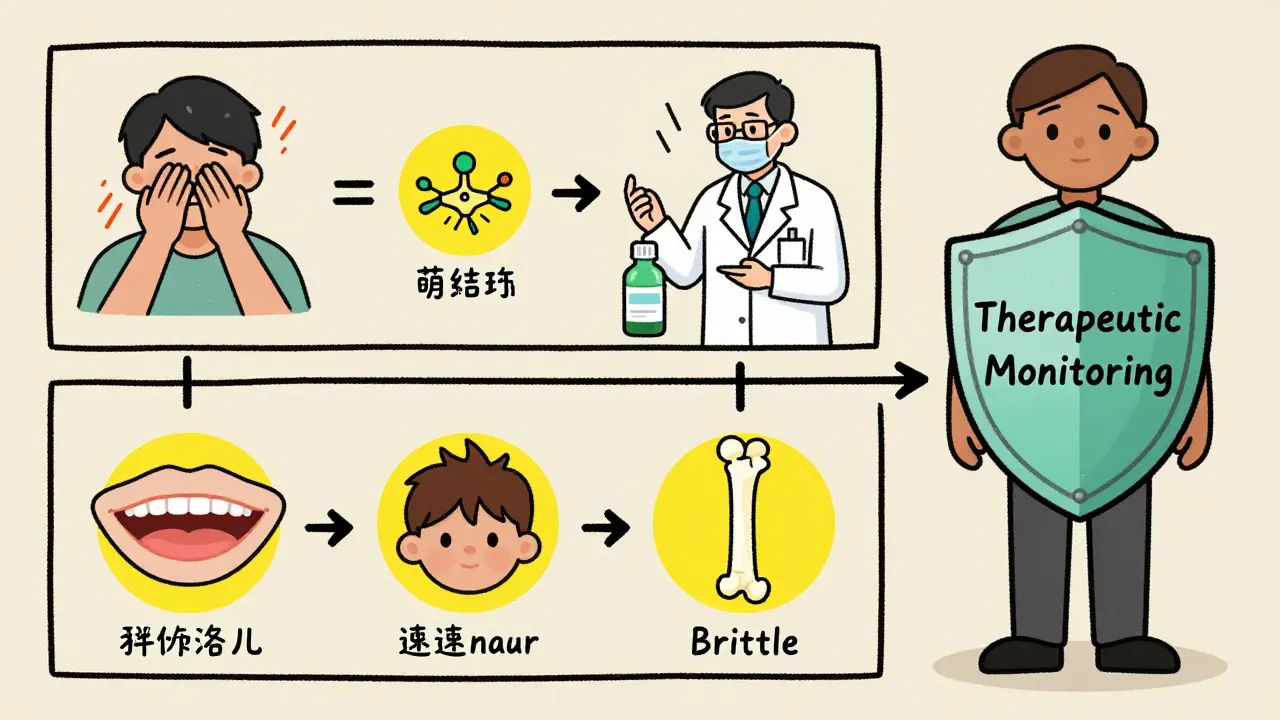
Long-Term Monitoring Beyond Blood Levels
Phenytoin doesn’t just affect the brain. Long-term use can cause:- Gingival hyperplasia (swollen gums)
- Hirsutism (excess hair growth)
- Thickened facial features
- Vitamin D deficiency
- Bone loss (osteomalacia)
- Folic acid deficiency
- Peripheral neuropathy
- Before starting: CBC, liver function, electrolytes, vitamin D, HLA-B*1502 testing (for patients of Han Chinese or Thai descent)
- Every 6-12 months: CBC, liver enzymes, electrolytes
- Every 2-5 years: Bone density, calcium, phosphate, vitamin D
What Clinicians Should Do
When switching phenytoin formulations:- Check a trough level just before the switch.
- Document the exact product name and manufacturer.
- Advise the patient to watch for new dizziness, tremors, confusion, or seizure activity.
- Recheck the level 5-10 days after the switch.
- If the level is outside 10-20 mcg/mL, consider switching back or adjusting the dose.
- If the patient is symptomatic, check free phenytoin, not just total.
Bottom Line
Generic phenytoin is not the same as generic ibuprofen. For most drugs, bioequivalence means you can swap freely. For phenytoin, bioequivalence doesn’t guarantee clinical safety. The stakes are too high. Therapeutic drug monitoring isn’t just a routine test here-it’s a safety net. Whether you’re a neurologist, a family doctor, or a pharmacist, if you’re managing phenytoin, you’re managing risk. And that means checking levels when you switch brands, when you add new drugs, and when the patient doesn’t feel right. It’s not about being overly cautious. It’s about knowing that for some drugs, the numbers on the lab report are the difference between control and crisis.Do I need to monitor phenytoin levels if I’m on a generic version?
Yes, especially if you’ve switched from the brand-name version or between different generic brands. Even though generics are approved as bioequivalent, phenytoin’s narrow therapeutic window and non-linear metabolism mean small differences in absorption can cause seizures or toxicity. Always check levels 5-10 days after switching.
Can I trust the lab’s total phenytoin level if I have low albumin?
No. Low albumin means more phenytoin is unbound and active, even if the total level looks normal. Use the corrected level formula as a rough guide, but if you’re unsure-especially in older adults or those with liver disease-ask for a free phenytoin level. That’s the only way to know the real amount of drug affecting your brain.
What if my phenytoin level is 22 mcg/mL but I feel fine?
Even if you feel okay, a level above 20 mcg/mL increases your risk of side effects like nystagmus, ataxia, or confusion. These may develop slowly. Don’t wait for symptoms. Talk to your doctor about reducing the dose. Toxicity can become dangerous fast-especially if you’re on other drugs that raise phenytoin levels.
Why does my doctor check my vitamin D and bone density if I’m on phenytoin?
Phenytoin speeds up the breakdown of vitamin D, which leads to low calcium and weak bones over time. This can cause osteomalacia-softening of the bones-which increases fracture risk. Checking vitamin D, calcium, and bone density every few years helps prevent this. It’s not about seizures-it’s about long-term health.
Can I switch back to brand-name phenytoin if I have problems with generics?
Yes. If you’ve had seizures or side effects after switching to a generic, you can request the brand-name version. Many insurance plans will cover it if you document clinical instability or toxicity linked to the switch. Keep a log of symptoms and levels-it helps your doctor make the case.
Are there any other drugs I should avoid while on phenytoin?
Yes. Avoid alcohol, St. John’s wort, and certain antibiotics like metronidazole or fluconazole without talking to your doctor. Also, be careful with seizure medications like valproate or carbamazepine-they interact strongly. Always review all your medications (including OTC and supplements) with your pharmacist or doctor before starting anything new.

Sam Davies
January 11, 2026 AT 05:46Oh wow, a post that doesn’t treat phenytoin like it’s just another pill you pop with your morning coffee. Shocking. I swear, if I had a dollar for every time a pharmacist swapped my meds without a second thought…
My cousin’s been on Dilantin since ’09. Switched to some generic because insurance said so. Three days later, she had a seizure in a Target parking lot. No one blamed the pharmacy. Everyone blamed her for ‘not taking it right.’
Phenytoin isn’t a drug. It’s a high-wire act with a side of math.
Alex Smith
January 12, 2026 AT 01:20Let me get this straight - the FDA says two drugs are bioequivalent if their absorption varies by up to 25%? That’s like saying two different sizes of shoes are ‘equivalent’ because they’re both ‘size 10.’
And yet we let this happen with a drug where 2 mcg/mL can mean the difference between seizure control and ICU admission. We’re not managing epilepsy here. We’re playing Russian roulette with lab reports.
Also, the protein binding thing? Yeah, that’s why older folks on phenytoin look fine on paper but are walking zombies. Albumin’s not a suggestion. It’s a biological fact.
Michael Patterson
January 13, 2026 AT 13:00ok so i read this whole thing and its like 90% common sense but also 10% like why is this even a debate? like if you have epilepsy and your drug is like a time bomb that goes off if the dose is off by 5mg then why are we even letting generics be swapped like its a pack of gum?
also the formula for corrected level? i tried it on my aunt and it gave me 23.4 and her actual free level was 18. so like… the formula is basically a guess with extra steps.
and dont get me started on the bone loss. my uncle broke his hip at 68 because he was on phenytoin for 20 years and no one ever told him to get his vit d checked. now he walks with a cane and blames the doctors. but really? the system failed him.
also typos are my thing so sorry if i spelled something wrong i was typing on my phone while eating a burrito
Matthew Miller
January 13, 2026 AT 22:20Anyone who thinks generics are interchangeable for phenytoin is either a pharmacist who’s never seen a patient die or a bureaucrat who thinks ‘bioequivalent’ means ‘clinically identical.’
Let me break this down for you: if you’re a neurologist and you don’t check levels after a switch, you’re not just negligent - you’re a liability. And if you’re a patient who got switched without warning? You’re not ‘noncompliant.’ You’re a victim of a broken system.
And yes, I’ve seen the charts. I’ve seen the spikes. I’ve seen the ER visits. This isn’t theory. It’s murder by formulary.
Madhav Malhotra
January 13, 2026 AT 22:32Back home in India, we use phenytoin all the time - mostly generics because that’s all we can afford. But our neurologists? They’re obsessive. They check levels, they ask about gums, they check vitamin D. They know this isn’t just another drug.
My uncle’s been on it for 15 years. No seizures. No broken bones. Why? Because his doctor never treated it like a commodity.
Maybe the West needs to learn from places where resources are scarce but care isn’t.
Priya Patel
January 15, 2026 AT 00:06OMG I just read this and I’m crying 😭 I’ve been on phenytoin for 8 years and I switched generics last year and had this weird dizzy spell for 3 weeks and no one would believe me because my ‘levels were fine’… until I begged for a free level test and it was 21.5. I felt so alone.
Thank you for writing this. I’m sharing this with my entire support group. We need to talk about this.
Jennifer Littler
January 16, 2026 AT 21:55Therapeutic drug monitoring for phenytoin is a classic example of pharmacokinetic complexity intersecting with real-world clinical practice. The non-linear metabolism, coupled with high protein binding and narrow therapeutic index, renders standard bioequivalence thresholds inadequate.
Moreover, the CYP-mediated interactions are not merely theoretical - they manifest clinically as acute toxicity or therapeutic failure. The use of corrected serum levels in hypoalbuminemic states is an evidence-based approximation, but free drug measurement remains the gold standard in complex cases.
Standardized protocols for formulation switching, including pre- and post-switch TDM, are not universally adopted - a systemic gap requiring policy intervention.
Jason Shriner
January 18, 2026 AT 20:04so like… phenytoin is basically the goth kid of meds. dramatic, unpredictable, and everyone pretends they understand it but really they just nod and hope it doesn’t explode.
and the formula? yeah its like trying to guess how much alcohol is in a drink when the bartender says ‘it’s fine’ but you know he’s been drinking too.
also i think the real problem is we treat patients like data points. not people. if you had to live with this drug you’d get it.
also i hate when people say ‘it’s just a pill’ like i’m not the one having seizures or falling down stairs because my brain forgot how to work
Sean Feng
January 19, 2026 AT 19:22Generic substitution is fine. People just need to stop being dramatic. If your seizure control went to crap after switching, maybe you’re just not taking it right.
Also why are we even talking about albumin? Just check the level. Done.
Stop overcomplicating everything.
Priscilla Kraft
January 20, 2026 AT 10:17Thank you for this. Seriously. I’m a nurse and I’ve seen too many patients get switched without a word. I always check levels after a switch now - even if the doctor doesn’t ask. I’ve saved at least three people from toxicity just by being the one who says ‘wait, let’s check this.’
And yes, the bone loss thing? I had a patient who broke her femur at 52 because she’d been on phenytoin for 25 years and never had a DEXA scan. She cried and said, ‘I thought the seizures were the only thing I had to worry about.’
Let’s make this standard. Not optional. 💙
Vincent Clarizio
January 21, 2026 AT 05:16Let me ask you this: if a drug’s therapeutic window is so narrow that a 25% variability in absorption can trigger seizures or coma, why are we even allowing it to be treated like a commodity? Why are we letting insurance companies decide who lives and who has a seizure in a grocery store?
This isn’t pharmacology. This is capitalism pretending to be medicine.
Phenytoin doesn’t care about your formulary tier. It doesn’t care if your pharmacy got a better deal on Generic B. It only cares about the unbound fraction in your plasma. And if you’re not measuring that - if you’re not thinking about albumin, if you’re not checking levels after every switch - you’re not treating a patient. You’re running a cost-cutting experiment.
And the worst part? The people paying for it aren’t the ones signing the prescriptions. They’re the ones having seizures. Or breaking bones. Or ending up in the ICU.
We’re not just bad at medicine. We’re morally lazy.
Christian Basel
January 22, 2026 AT 22:38Non-linear pharmacokinetics. Narrow therapeutic index. CYP interactions. Protein binding variability. All valid points. But the data on clinical outcomes after generic substitution is mixed. Some studies show no difference. Others do. The meta-analyses are inconclusive.
So let’s not overstate the risk. We’re talking about a small subset of patients. Most do fine.
Also, the formula for corrected levels? It’s not validated in renal failure. Don’t use it blindly.
Roshan Joy
January 24, 2026 AT 05:47I’m from India too - we use generics for everything, but our doctors here are super careful with phenytoin. My cousin’s neurologist keeps a notebook with every generic brand she’s ever taken. He even calls the pharmacy to confirm the manufacturer before refill.
And yeah, he checks vitamin D every year. I thought it was weird at first - but now I get it. It’s not just about seizures. It’s about living.
Maybe we don’t have fancy labs, but we have common sense. And that’s worth more than a discount.
Adewumi Gbotemi
January 24, 2026 AT 19:03Simple truth: if a drug can kill you when the dose is off by a little, then don’t swap it like you’re changing socks.
People in Nigeria use phenytoin too. We don’t have much, but we know this one isn’t like others. We watch. We check. We don’t guess.
Why can’t the rest of the world do the same?
Michael Patterson
January 25, 2026 AT 18:59wait so if i got switched from dilantin to some generic and my level went from 14 to 21 and i started having tremors and my gums swelled up - that’s not just bad luck? that’s the system failing me?
oh wow. that’s actually kinda horrifying.
so i guess i should’ve demanded a free level test. but i didn’t know that was a thing.
thanks for the info. i’m printing this out and taking it to my doctor tomorrow.