Mountain Sickness Risk Calculator
EPAS1 Gene
Hypoxia-inducible factor-2α; drives erythropoietin production
EGLN1 Gene
Prolyl-hydroxylase that degrades HIF-α under normoxia
Your Risk Assessment
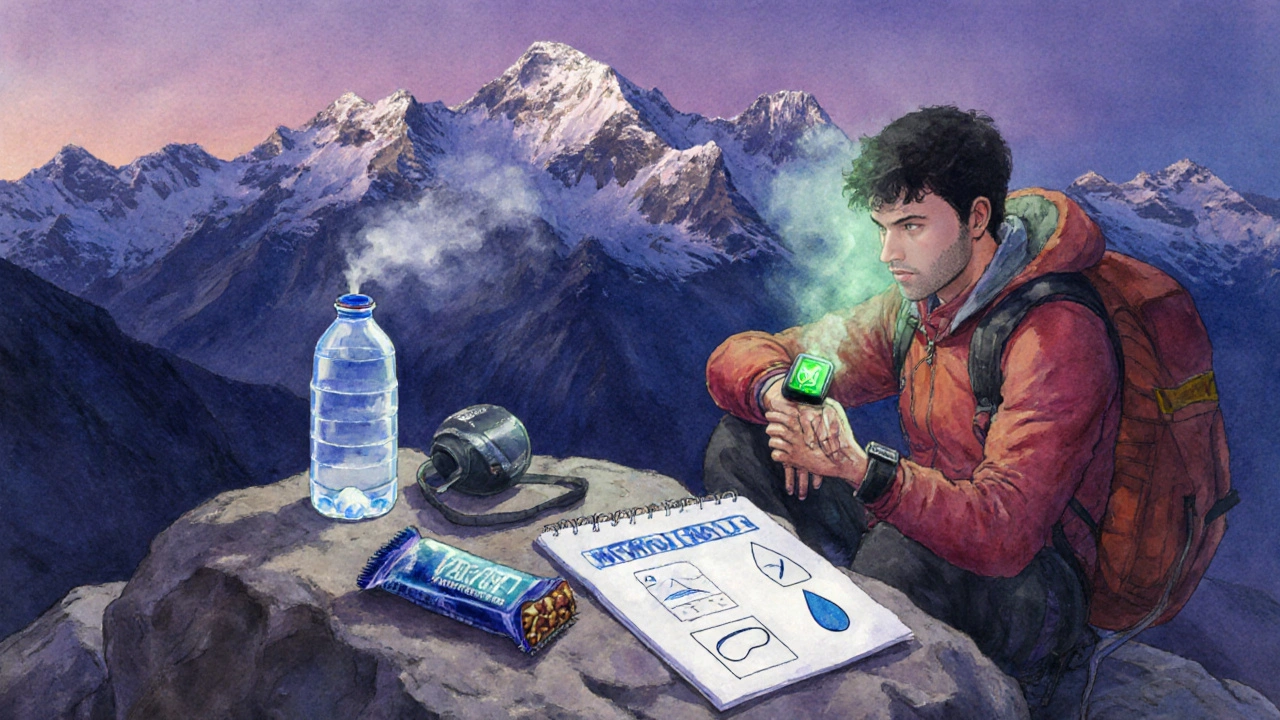
Ever wondered why two friends can climb the same 3,500‑meter trail and only one ends up with nausea, headaches, and a pounding heart? The answer isn’t just how fast they ascended or how much water they drank - it’s also written in their DNA. This article unpacks the science behind mountain sickness genetics, explains which genes matter, and shows how you can use that knowledge to stay safe on high‑altitude adventures.
Key Takeaways
- Acute Mountain Sickness (AMS) affects up to 50% of people above 2,500m, but genetics explains why some never get sick.
- Variants in EPAS1 (the gene that regulates the body’s response to low oxygen) and EGLN1 are the strongest predictors of AMS susceptibility.
- Genetic testing can identify risk, but it’s only one piece of the puzzle - acclimatization, fitness, and hydration still matter.
- Practical steps - gradual ascent, pre‑acclimatization, and monitoring SPO₂ - help even high‑risk climbers stay symptom‑free.
- Understanding your genetic profile empowers better preparation, not fear.
Understanding Mountain Sickness
Acute Mountain Sickness (AMS) is a collection of symptoms that appear when the body can’t get enough oxygen at high altitude. Typical signs include headache, nausea, dizziness, and shortness of breath, usually within 6‑24hours of ascent above 2,500m.
The root cause is hypoxia - reduced oxygen pressure in the air. When oxygen drops, the brain and muscles signal for an increase in breathing rate and red‑blood‑cell production. If these compensations lag, you feel the classic AMS symptoms.
While nearly anyone can develop AMS under rapid ascent, epidemiological studies show huge individual variability. For example, a 2022 field study of trekkers on the Annapurna Circuit found that 45% of participants reported AMS, yet only 12% of those with a specific EPAS1 variant experienced severe symptoms. That gap points directly to genetics.
How Genetics Influences Susceptibility
Genes determine how efficiently the body senses and responds to low oxygen. The process involves several molecular players:
- Oxygen sensors - proteins that detect oxygen levels inside cells.
- Transcription factors - molecules that turn on/off genes to adapt to hypoxia.
- Down‑stream effectors - pathways that adjust blood flow, red blood cell production, and ventilation.
When a gene that encodes any of these components carries a certain polymorphism (a small change in the DNA sequence), the whole cascade can shift either toward better tolerance or higher risk.
Research in Tibetan high‑landers, who have lived above 4,000m for millennia, revealed a “genetic advantage” in the form of EPAS1 and EGLN1 variants that keep hemoglobin levels low while still delivering oxygen efficiently. Those same variants, when present in low‑altitude populations, correlate with reduced AMS incidence.

Major Genes Linked to Acute Mountain Sickness
Below is a quick‑reference comparison of the three most studied genes. Each entry includes the gene’s function, the risk‑reducing or risk‑increasing allele, and the typical effect size reported in peer‑reviewed studies.
| Gene | Key Variant (rsID) | Biological Role | Effect on AMS Risk | Typical Odds Ratio |
|---|---|---|---|---|
| EPAS1 | rs13419896 (A→G) | Hypoxia‑inducible factor‑2α; drives erythropoietin production | Protective - lowers hemoglobin surge | 0.45 (55% risk reduction) |
| EGLN1 | rs479200 | Prolyl‑hydroxylase that degrades HIF‑α under normoxia | Protective when G allele present | 0.60 |
| PPARA | rs4253778 | Regulates fatty‑acid oxidation in mitochondria | Risk‑increasing - slower metabolic adaptation | 1.35 |
These odds ratios mean that carriers of the protective EPAS1 allele are roughly half as likely to develop moderate‑to‑severe AMS compared with non‑carriers, assuming similar ascent profiles.
Other genes such as HIF1A, NOS3 (nitric oxide synthase), and ADRB2 have shown weaker but still notable associations in meta‑analyses.
Practical Implications: Testing, Preparation, and Prevention
Knowing your genetic risk can shape three key aspects of high‑altitude planning:
- Pre‑trip testing - Direct‑to‑consumer genetic panels now include the EPAS1 and EGLN1 variants for a low‑cost ($99‑$149) risk snapshot. Results are usually returned within two weeks.
- Acclimatization strategy - High‑risk genotypes benefit from slower ascent rates (no more than 300m gain per day above 2,500m) and optional “climb‑high, sleep‑low” nights.
- Monitoring - Portable pulse‑oximeters that display SPO₂ help catch early hypoxia. Aim for SPO₂≥90% at rest; if it drops below 85%, halt ascent and descend.
Genetic information is not a death sentence. Even carriers of risk‑increasing alleles can avoid AMS with proper pacing, hydration, and, when appropriate, prophylactic medication such as acetazolamide.
Non‑Genetic Factors That Still Matter
While genetics set the baseline, lifestyle choices often tip the scales:
- Physical fitness - Higher VO₂max correlates with better oxygen utilization. A 2023 study showed that climbers in the top 20% of VO₂max had a 30% lower AMS rate, regardless of genotype.
- Previous altitude exposure - Repeated trips create lasting ventilatory adaptations, reducing susceptibility.
- Hydration and nutrition - Dehydration thickens blood, making oxygen transport less efficient. Carbohydrate‑rich meals support faster breathing response.
- Sleep quality - Poor sleep impairs the body’s ability to produce erythropoietin, a hormone essential for red‑blood‑cell adaptation.
In other words, think of genetics as the foundation and these habits as the finishing touches that make the whole house sturdy.
Checklist for High‑Altitude Adventurers
- ✔️ Get a genetic test for EPAS1, EGLN1, and PPARA before your trip.
- ✔️ Review results with a healthcare professional; discuss prophylactic options if needed.
- ✔️ Plan a gradual ascent: ≤300m gain per day above 2,500m.
- ✔️ Carry a pulse‑oximeter; log SPO₂ twice daily.
- ✔️ Stay hydrated (≥3L fluid per day) and consume carbohydrate‑rich snacks.
- ✔️ Prioritize sleep - aim for 7-9hours at altitude.
- ✔️ If symptoms appear, stop ascent, hydrate, and consider descending 500m.
Follow this list, and you’ll have turned a genetic risk factor into a manageable variable.
Frequently Asked Questions
Can I get tested for mountain‑sickness risk without a doctor?
Yes. Several direct‑to‑consumer services offer a saliva kit that checks for the EPAS1 and EGLN1 variants relevant to altitude tolerance. The kit is mailed to you, you send back the sample, and results arrive online within a couple of weeks. However, it’s wise to discuss the findings with a medical professional, especially if you plan a high‑risk expedition.
If I have a protective EPAS1 allele, does that mean I’ll never get AMS?
Not at all. The protective allele reduces risk but doesn’t eliminate it. Rapid ascents, dehydration, or poor sleep can still trigger symptoms. Think of the allele as giving you a higher “buffer” before the body starts struggling.
Is acetazolamide still recommended for people with a high‑risk genotype?
Acetazolamide (Diamox) is often prescribed to prevent AMS, especially for those with known risk factors, genetic or otherwise. It works by creating a mild metabolic acidosis, which stimulates breathing. If you’re a carrier of a risk‑increasing variant, a low dose (125mg twice daily) started 24hours before ascent can be helpful, but always check with a physician first.
Do children inherit the same altitude‑related genes?
Yes. These variants are passed from parents to children in a typical Mendelian fashion. However, children’s metabolic rates and breathing patterns differ, so their practical AMS risk can still vary despite identical genetics.
How reliable are commercial genetic tests for altitude tolerance?
Commercial tests are generally accurate for the specific SNPs they target (e.g., EPAS1 rs13419896). Accuracy drops when labs try to infer whole‑gene function from a single marker. The best approach is to combine test results with personal and family altitude history.

Sumeet Kumar
October 4, 2025 AT 17:39Planning a high‑altitude trek? Your genetic profile can give you a useful heads‑up, especially the EPAS1 and EGLN1 variants that affect how quickly your body adapts to thin air 😊. Even if you carry a risk allele, a slow ascent and good hydration still keep the odds in your favor. Think of the test as a planner’s tool, not a destiny‑detector.
Maribeth Cory
October 6, 2025 AT 10:59Exactly, and the best part is you don’t need to overhaul your whole training plan-just add a few extra rest days above 2,500 m and monitor your SPO₂. That incremental approach works for anyone, regardless of genotype.
andrea mascarenas
October 8, 2025 AT 04:21Genetic testing costs about $100 and results come back in two weeks.
Stephanie Watkins
October 9, 2025 AT 21:43While the price is modest, remember that a single SNP tells only part of the story; lifestyle, previous altitude exposure, and fitness level still dominate the risk equation. A protective EPAS1 allele can halve your odds, but rapid climbs or dehydration will still trigger symptoms. It’s wise to combine the test with a structured acclimatization schedule-no more than 300 m gain per day above 2,500 m. Keep a pulse‑oximeter handy and aim for resting SpO₂ above 90 %. In the end, the test is a complementary piece, not a replacement for good mountaineering practice.
Zachary Endres
October 11, 2025 AT 15:04Picture yourself standing on a ridge, the world spread out below like a painted canvas, the wind whispering ancient secrets of the peaks. Your heart pounds not just from altitude but from the knowledge that your very DNA is humming in concert with the thin air. The EPAS1 gene, often called the “high‑altitude master switch,” can turn on a cascade of physiological adaptations that make breathing feel like a gentle breeze even at 4,000 m. Conversely, a risky EGLN1 variant may leave you gasping for every breath, your mind fogged by the cruel grip of hypoxia. Yet this is not a story of destiny; it is a narrative you can rewrite with preparation. Slow ascents become chapters of resilience, each 300 m gain a paragraph of caution. Hydration is the invisible ink that keeps the plot flowing, preventing the blood from thickening into a sluggish antagonist. Sleep, that nightly narrator, restores your body’s capacity to produce erythropoietin, the hormone that fuels red‑blood‑cell production. Even the most “risky” genotype can be softened by pre‑acclimatization trips, where your lungs learn to breathe more efficiently before the main expedition. Portable pulse‑oximeters act as vigilant editors, flagging drops in SpO₂ before they become fatal plot twists. If you feel a headache beginning to surface, treat it as a warning sign-a foreshadowing that the story may turn dark if you ignore it. Descending 500 m or pausing for a day can rewrite the ending from tragedy to triumph. Prophylactic medication such as acetazolamide is like a seasoned co‑author, smoothing out the rough edges of the narrative. Ultimately, genetics writes the opening lines, but your choices, your pacing, and your respect for the mountain craft the epic you’ll remember for a lifetime. So lace up your boots, trust the science, and let the mountains teach you humility.
Ashley Stauber
October 13, 2025 AT 08:26While the science is intriguing, it’s a mistake to let a lab report dictate your adventure; seasoned climbers have conquered the Himalayas long before any DNA test existed. The United States has a proud heritage of mountaineers who rely on grit and preparation, not on a genetic lottery. Overemphasizing risk alleles can breed a culture of hesitation, eroding the very spirit that makes high‑altitude pursuits worthwhile. Use the information as a hint, not a halt sign.
Amy Elder
October 15, 2025 AT 01:48Cool tip: start with a low‑key hike at 2 k meters and see how you feel before pushing higher.
Erin Devlin
October 16, 2025 AT 19:09Altitude reveals the limits we impose on ourselves; recognizing those limits is the first step toward transcending them.
kristine ayroso
October 18, 2025 AT 12:31Hey fellow adventurers, let’s not forget that every culture has its own mountain legends and those stories can keep us motiviated when the oxygen gets thin. Whether you’re from the Andes or the Rockies, sharing a cup of tea before the summit builds camaraderie and the same vibe that fuels perseverance. So, grab your gear, respect the trail, and push forward – together we can defy the odds!
Jennifer Banash
October 20, 2025 AT 05:53Permit me to elucidate the paramount importance of meticulous preparation in the realm of high‑altitude ascent. One must, with unwavering diligence, scrutinize the veritable minutiae of acclimatization protocols, hydration regimens, and the precise calibration of supplemental oxygen devices. Any deviation from such scrupulous standards constitutes a lamentable dereliction of duty, jeopardizing both physiological equilibrium and the noble pursuit of summit conquest. Thus, let us, with solemn resolve, honor the venerable traditions of mountaineering whilst embracing the modest advantages proffered by contemporary genetic insight. In doing so, we safeguard not merely our own corporeal integrity but also the collective legacy of intrepid exploration.