Antihistamine Safety Checker for Seniors
Is This Antihistamine Safe for Older Adults?
Check if your antihistamine is safe for seniors based on fall risk and anticholinergic activity. First-generation drugs significantly increase fall risk.
Every year, nearly 36 million falls happen among adults 65 and older in the U.S. About one in four of them will fall. Many of these falls aren’t accidents-they’re side effects of medications people think are harmless. One of the biggest hidden dangers? First-generation sedating antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine. These drugs are sold over the counter, often used for allergies, colds, or sleep. But for older adults, they can be deadly.
Why Sedating Antihistamines Are Dangerous for Older Adults
First-generation antihistamines don’t just block histamine in the nose or throat. They cross the blood-brain barrier and hit the central nervous system hard. This causes drowsiness, slowed reaction time, poor balance, and dizziness-all of which make falls much more likely. Older adults are especially vulnerable because their bodies process these drugs differently. Liver and kidney function slow down with age, so the drugs stick around longer. Diphenhydramine, for example, has a half-life of 8.5 hours in young adults but stretches to 13.5 hours in people over 65. That means drowsiness can last well into the next day, even if they took it the night before. The American Geriatric Society has labeled these drugs as “potentially inappropriate” for older adults in their Beers Criteria. Why? Because they don’t just cause sleepiness. They also trigger dry mouth, blurred vision, constipation, confusion, and even delirium. A 2025 study tracking nearly 200,000 older adults found that 32% filled a prescription for a vestibular suppressant-mostly first-gen antihistamines-and 8% fell within 60 days. That’s not a small risk. That’s a pattern.The Science Behind the Risk: First-Gen vs. Second-Gen
Not all antihistamines are the same. Second-generation options like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed to stay out of the brain. They work just as well for allergies but cause far less sedation. Here’s the key difference:- First-generation (diphenhydramine, chlorpheniramine): Strong anticholinergic activity (score of 3-4 on the Anticholinergic Cognitive Burden Scale). High fall risk.
- Second-generation (fexofenadine, loratadine): Minimal anticholinergic activity (score of 0-1). Low to no increased fall risk.
How Common Is This Problem?
Surprisingly, very common. Despite clear warnings, first-generation antihistamines are still widely used. Sales data from 2024 shows diphenhydramine is the third most purchased OTC sleep aid in the U.S. among people 65+, with over 28 million units sold annually. That’s $142 million in sales-mostly to people who don’t realize they’re putting themselves at risk. Even worse, doctors still prescribe them. A 2019 study found that 12.7% of older adult visits included a prescription for a first-gen antihistamine-almost the same rate as for younger adults. That’s a “one-size-fits-all” approach that ignores how aging changes drug metabolism. Primary care doctors prescribe them more often than dermatologists, even though allergy patients are the main users. The disconnect between evidence and practice is alarming.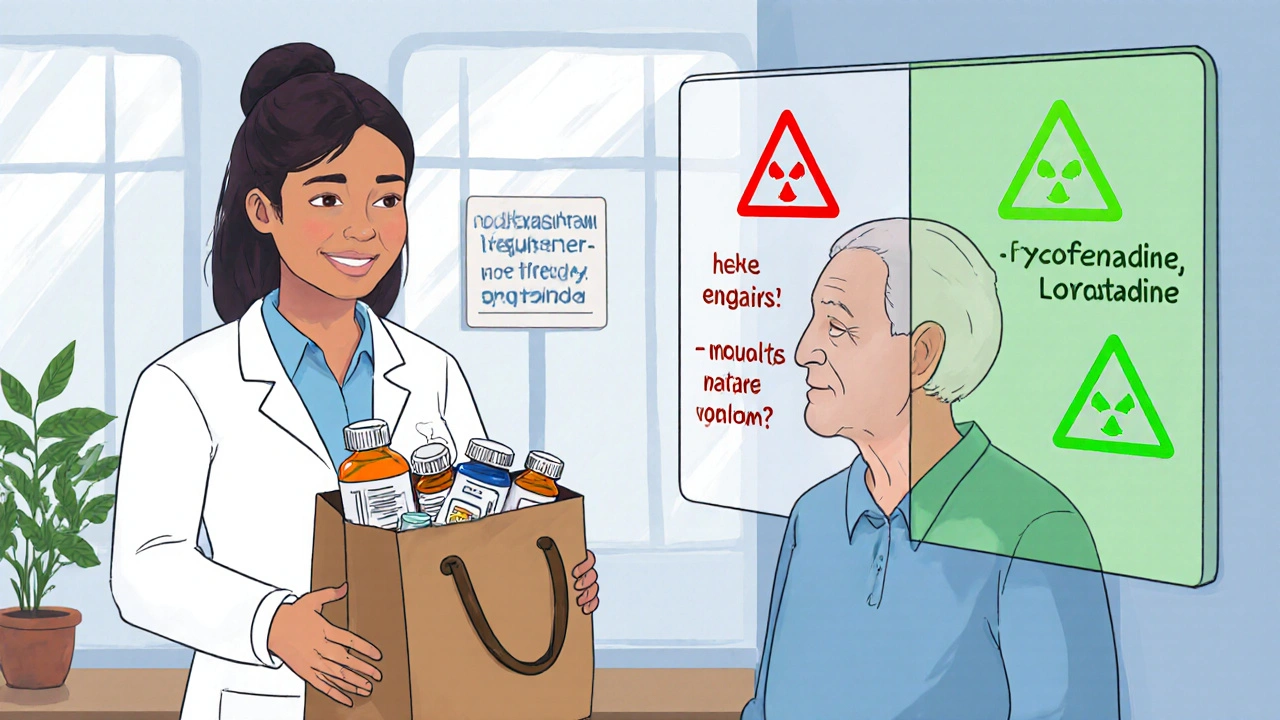
What Can Be Done? Prevention Strategies That Work
The good news? This risk is preventable. The CDC’s STEADI initiative (Stopping Elderly Accidents, Deaths & Injuries) gives a clear three-step plan: STOP, SWITCH, REDUCE.- STOP: If someone is taking diphenhydramine for sleep or allergies, ask if it’s really needed. Many older adults take it out of habit or because they’ve been told it’s “safe.” Often, it’s not.
- SWITCH: Replace first-gen antihistamines with second-gen ones. Fexofenadine and loratadine are just as effective for allergies and don’t increase fall risk. For sleep, skip the pills entirely-try sleep hygiene instead.
- REDUCE: If a sedating antihistamine must be used, use the lowest dose possible (e.g., 12.5 mg instead of 25 mg of diphenhydramine) and take it at night, not during the day.
Non-Drug Alternatives That Actually Work
You don’t need pills to manage allergies or sleep. Here are proven, safer options:- Nasal saline irrigation: Rinsing the nose with salt water reduces allergy symptoms by 35-40%, according to JAMA Otolaryngology.
- Allergen-proof bedding: Covers for pillows and mattresses reduce dust mite exposure by 83%.
- HEPA air filters: Remove 99.97% of airborne allergens like pollen and pet dander.
- Non-drug sleep strategies: Stick to a consistent bedtime, avoid caffeine after noon, keep the bedroom cool and dark, and get morning sunlight to reset your circadian rhythm.
Environmental Changes to Prevent Falls
Even if you can’t stop the medication right away, you can reduce the chance of a fall. Simple home changes make a huge difference:- Install grab bars in bathrooms-reduces fall risk by 28%.
- Improve lighting in hallways, stairs, and bathrooms-cuts falls by 32%.
- Remove tripping hazards: loose rugs, clutter, extension cords.
- Use non-slip mats in the shower and near the sink.

Role of Pharmacists and Care Teams
Pharmacists are often the first to spot dangerous medication use. Many older adults don’t tell their doctors about OTC drugs they take. A “brown bag review”-where patients bring all their pills, supplements, and OTC meds to the pharmacy-can uncover an average of 3.2 high-risk medications per person. Studies show pharmacist-led reviews reduce fall risk by 26%. Doctors and nurses should ask three simple questions during annual check-ups:- Have you fallen in the past year?
- Do you feel dizzy or unsteady when standing up?
- Are you taking any over-the-counter sleep aids or allergy meds?
What’s Next? New Hope on the Horizon
There’s promising research coming. Two new antihistamines-AGS-2025-01 and FEX-AGE-101-are in Phase II trials. Early results show they cause 89% less drowsiness than diphenhydramine while still blocking histamine effectively. These are designed specifically for older adults, with minimal brain penetration. But we don’t have to wait. Right now, we have the tools to prevent thousands of falls. We just need to use them.Are over-the-counter antihistamines safe for seniors?
No, first-generation OTC antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are not safe for older adults. They significantly increase the risk of falls, confusion, and delirium. Second-generation options like fexofenadine (Allegra) and loratadine (Claritin) are much safer alternatives. Always check the active ingredient-many cold and sleep meds contain hidden sedating antihistamines.
Can I stop taking diphenhydramine cold turkey?
If you’ve been taking diphenhydramine regularly for sleep or allergies, don’t stop suddenly. Withdrawal can cause rebound symptoms like worse allergies or insomnia. Work with a doctor or pharmacist to taper off slowly while introducing non-drug alternatives like nasal rinses or sleep hygiene practices. This reduces discomfort and prevents symptom flare-ups.
Why do doctors still prescribe diphenhydramine to older patients?
Many doctors aren’t aware of the latest guidelines or assume the drug is harmless because it’s available without a prescription. Others prescribe it because patients ask for it or because it’s cheap and familiar. But research shows it’s outdated and dangerous for seniors. The American Geriatrics Society has warned against it for over a decade. It’s time for both clinicians and patients to demand safer options.
What’s the safest antihistamine for seniors with allergies?
Fexofenadine (Allegra) is the safest choice for older adults. It has the lowest risk of drowsiness and no significant anticholinergic effects. Loratadine (Claritin) is also a good option. Avoid cetirizine (Zyrtec) if possible-it causes drowsiness in about 14% of seniors. Always choose non-sedating versions and avoid combination products with decongestants or pain relievers, which add more risk.
How can I help an older relative who’s taking Benadryl for sleep?
Start by talking to their doctor or pharmacist about switching to a safer sleep strategy. Encourage consistent bedtime routines, limiting screen time before bed, and avoiding caffeine after noon. If they need help falling asleep, melatonin (3 mg or less) is a safer short-term option than diphenhydramine. Never replace one risky drug with another. Focus on habits, not pills.
Next Steps for Families and Caregivers
If you’re caring for an older adult:- Do a “brown bag” medication review-collect every pill, bottle, and supplement they take, and bring it to their pharmacist or doctor.
- Check labels for diphenhydramine, chlorpheniramine, or doxylamine-these are common hidden ingredients in cold, flu, and sleep meds.
- Replace OTC sedating antihistamines with non-drug allergy and sleep solutions.
- Make home safety a priority: install grab bars, remove rugs, add nightlights.
- Ask: “Is this medication still needed?” every time a new one is added.

Dalton Adams
November 21, 2025 AT 22:42Let’s be real-diphenhydramine is a relic from the 1940s, and yet it’s still the go-to for seniors? The anticholinergic burden scale isn’t a suggestion; it’s a warning label written in blood. And don’t get me started on how pharmacists are the only ones who actually read labels anymore. Fexofenadine? 0.5 mg/kg for a 70kg adult? Done. No drowsiness. No confusion. No broken hips. Why is this even a debate? The science has been settled since 2012. Someone’s still selling this poison like it’s candy. #StopTheBenadrylCult
Kane Ren
November 22, 2025 AT 18:17This is such an important post. I’m so glad someone’s finally talking about this. My grandma switched from Benadryl to Allegra last year, and she hasn’t stumbled once since. She sleeps better too-without pills. It’s not magic, it’s just smart. We can do better for our elders. Thank you for sharing the real solutions.
Karla Morales
November 23, 2025 AT 00:38While the data presented here is statistically robust, I must emphasize the methodological limitations of observational studies in pharmacovigilance. Confounding variables such as polypharmacy, cognitive decline, and environmental factors are rarely fully controlled. That said, the consistent association between first-generation antihistamines and fall risk across multiple cohorts is compelling. The 54% increase in injurious falls is not merely correlational-it’s causal in context. Furthermore, the cost-benefit analysis of switching to fexofenadine is overwhelmingly favorable. The only barrier is systemic inertia.
Javier Rain
November 24, 2025 AT 22:17YES. This is the kind of info we need to shout from the rooftops. My aunt was on Benadryl every night for ‘sleep’-turns out she was having mini-strokes from the anticholinergic load. We switched her to melatonin + sleep hygiene, and now she’s hiking with her grandkids again. It’s not about being perfect-it’s about being smarter. Stop treating seniors like they’re just old. Treat them like they’re worth keeping alive. #SwitchToAllegra
Laurie Sala
November 25, 2025 AT 12:59...I just found out my dad has been taking Benadryl for years... I didn't even know... I feel so guilty... I thought it was harmless... I just... I don't know what to do... I'm so scared... Please tell me it's not too late... I love him so much...
Lisa Detanna
November 25, 2025 AT 19:28I come from a culture where elders are treated like living libraries-and we don’t let them be poisoned by ignorance. In my family, we call it ‘medicine respect.’ If it’s not on the label, we don’t assume it’s safe. We ask. We research. We switch. This isn’t just American healthcare failure-it’s a global failure of intergenerational care. Let’s fix it together.
Demi-Louise Brown
November 27, 2025 AT 15:07Matthew Mahar
November 27, 2025 AT 19:07wait wait wait-so benadryl is actually dangerous??? i thought it was just sleepy-time juice??? my mom takes it every night for ‘allergies’ but she’s always falling over the coffee table… i’m gonna check her cabinet right now… oh my god there’s like 5 different bottles with diphenhydramine in them… this is insane…
John Mackaill
November 28, 2025 AT 08:48Thank you for this. I work with older adults in the UK, and the same problem exists here. Many GPs still default to diphenhydramine because it’s cheap and familiar. But when we do a brown bag review, the results are always the same: 3-4 high-risk meds, and Benadryl is always on the list. We’ve started running ‘Medication Safety Cafés’-informal drop-ins where seniors bring their meds and we chat. It’s working. Change is slow, but it’s possible. You’re not alone in this fight.