When you pick up a prescription for a generic combination drug, you expect the same results as the brand name version. After all, the active ingredients are identical. But what if the problem isn’t what’s in the pill-it’s what’s not in it? Many patients don’t realize that generic combination drugs can differ dramatically in their inactive ingredients, and those differences can have real consequences.
Why Generic Combinations Aren’t Always the Same
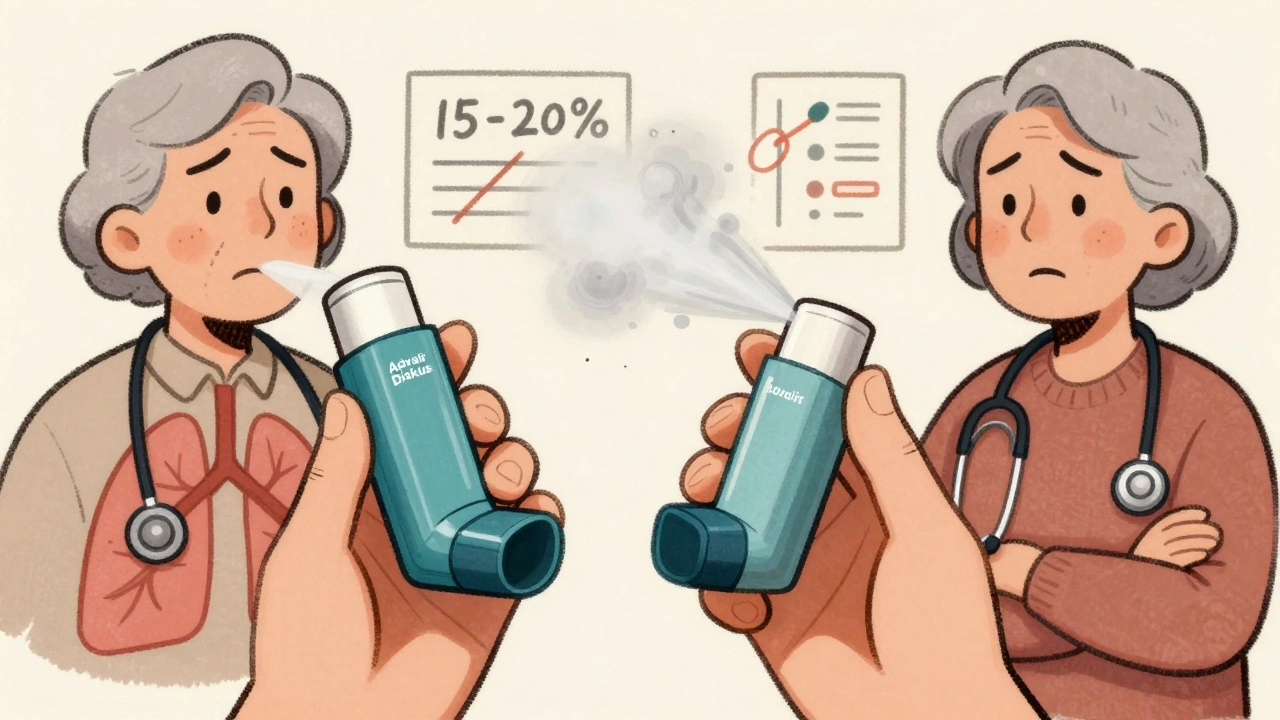
Generic drugs are required to have the same active ingredients, strength, and dosage form as the brand name. That’s the law. But when it comes to fillers, binders, coatings, and preservatives? Those can change completely. The FDA allows this flexibility because the focus is on bioequivalence: does the drug get into your bloodstream at a similar rate and amount? The answer is usually yes-within a 80-125% range for absorption. But that’s not the whole story. For drugs with a narrow therapeutic index-where even a small change in blood levels can cause harm-those tiny differences in inactive ingredients matter. Take levothyroxine, for example. A 2020 study of nearly 90,000 Medicare patients switching from brand to generic levothyroxine found that over 12% needed a dose adjustment because their thyroid levels shifted. That’s not a glitch. That’s a formulation issue. Combination drugs like Advair Diskus (fluticasone/salmeterol) add another layer of complexity. The inhaler device itself is part of the drug delivery system. In 2021, independent tests showed some generic versions delivered 15-20% less medication to the lungs. That’s not just a difference-it’s a clinical risk for asthma patients.What’s Really in Your Generic Pill?
The inactive ingredients in generics aren’t just random. They’re chosen for cost, stability, and manufacturability. But they can trigger reactions or alter how the drug behaves. A 2017 study found that nearly half of all generic combination drugs had different inactive ingredients than their brand counterparts. The most common changes?- 38% switched magnesium stearate (a lubricant)
- 29% changed lactose (a filler)
- 22% altered microcrystalline cellulose (a binder)
Who’s at Risk?
Not everyone will notice a difference. For most people, generics work just fine. But certain groups are more vulnerable:- Patients on narrow therapeutic index (NTI) drugs: warfarin, digoxin, levothyroxine, phenytoin, and some anti-seizure meds
- Elderly patients on multiple medications-more chances for interactions
- People with chronic conditions like asthma, epilepsy, or heart failure
- Those who’ve had a bad reaction to a generic before
Authorized Generics: The Middle Ground
There’s a version of generic that’s almost identical to the brand: the authorized generic. These are made by the original brand company but sold under a generic label. For example, Pfizer makes an authorized generic of Lyrica. It has the exact same ingredients, the same manufacturing process, the same everything. The catch? They cost 15-20% more than standard generics. Still, they’re 60-70% cheaper than the brand. For patients who’ve had bad experiences with generics, this is often the best option. But most insurance plans don’t prioritize them. You usually have to ask for them specifically.What You Can Do
You don’t have to accept a bad substitution. Here’s what to do:- Check the FDA’s Orange Book. Look up your drug. If it has an “A” rating, it’s considered therapeutically equivalent. If it has a “B” rating, proceed with caution.
- Ask your pharmacist: “Is this an authorized generic?” If not, ask if they can get one.
- Review the inactive ingredients. The label should list them. If you’re allergic to lactose, gluten, or dyes, cross-check them.
- Track your symptoms. If you feel different after switching-worse side effects, less control over your condition-document it. Bring it to your doctor.
- Don’t be afraid to ask for the brand. Some insurance plans require prior authorization, but if you’ve had a documented issue, they often approve it.

The Bigger Picture
The system was built to save money-and it has. Since 2006, Medicare has saved over $1.6 trillion using generics. That’s huge. But savings shouldn’t come at the cost of safety. The FDA is starting to catch up. In 2023, they approved Teva’s generic version of Advair Diskus with new requirements: the inhaler device had to match the brand’s performance. That’s a first. The agency now requires additional dissolution testing for 28 high-risk combination products. And by 2025, generic manufacturers are expected to clearly list all inactive ingredients on packaging. Meanwhile, research is underway. The NIH launched a $12.5 million initiative in early 2023 to build better models for predicting how formulation differences affect real patients. This isn’t just about pills anymore-it’s about personalized medicine.Bottom Line
Generic combination drugs are safe and effective for most people. But they’re not all the same. If you’re on a critical medication, especially one with a narrow therapeutic window, don’t assume the generic is interchangeable. Talk to your pharmacist. Know what’s in your pill. Track how you feel. And if something changes-speak up. Your health isn’t a cost-saving metric. It’s personal.Are generic combination drugs always safe to switch to?
For most people, yes. But for patients on narrow therapeutic index drugs like warfarin, levothyroxine, or certain anti-seizure medications, switching can cause measurable changes in blood levels. Studies show 12-23% of these patients may need a dose adjustment or experience reduced effectiveness after switching. Always check with your doctor or pharmacist before switching.
How do I know if my generic has different ingredients?
Look at the drug label. Inactive ingredients are listed under “Inactive Ingredients” or “Other Ingredients.” You can also ask your pharmacist for the full ingredient list. The FDA’s Orange Book doesn’t list inactive ingredients, but the manufacturer’s website or patient information leaflet usually does.
Can I request the brand-name version instead?
Yes. If you’ve had a bad reaction to a generic, or if your condition is unstable after switching, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription. Insurance may require prior authorization, but they often approve it if there’s documented clinical need.
What’s the difference between a generic and an authorized generic?
A standard generic is made by a different company and may have different inactive ingredients. An authorized generic is made by the original brand company under a different label. It has the exact same active and inactive ingredients, same manufacturing process, and same performance. It’s cheaper than the brand but more expensive than a standard generic.
Why do some pharmacies automatically switch to generics?
Most insurance plans require the cheapest option unless the prescriber blocks substitution. Pharmacists are often legally required to substitute unless the prescription says “Do Not Substitute.” This is designed to save money-but it doesn’t always account for individual patient needs. Always confirm what you’re getting.

Dan Cole
December 6, 2025 AT 23:42Let me be crystal clear: this isn't about generics being bad-it's about the FDA letting pharmaceutical corporations off the hook with a 80-125% bioequivalence loophole. That's not medicine, that's roulette with your life. If your thyroid levels swing because some lab in India swapped out microcrystalline cellulose for cheaper corn starch, that's not 'equivalent,' that's negligence dressed up as cost-cutting.
And don't get me started on inhalers. You're not just getting a different pill-you're getting a different delivery system. A 15-20% drop in lung deposition? That's not a variance, that's a death sentence for asthmatics who rely on precision. The FDA's new testing requirements? Too little, too late. We've been screaming about this for a decade.
Authorized generics? Brilliant idea. But why should patients have to beg for the exact same drug the brand makes? That's like buying a Ferrari and getting a knockoff that looks identical but the engine’s made of balsa wood. The system is rigged. And the people paying the price? The sick ones.
It's not about 'saving money.' It's about corporate greed masquerading as public policy. And if you think this is an isolated issue, you haven't been paying attention. Every time a pharmacy swaps your med without telling you, they're playing God with your biology. Wake up.
Max Manoles
December 7, 2025 AT 06:07I’ve been on levothyroxine for 12 years. Switched to a generic in 2020. My TSH went from 1.8 to 6.4 in six weeks. No symptoms at first-just fatigue, weight gain, brain fog. Then I started having panic attacks. Took me three months and three different generics to find one that didn’t make me feel like I was drowning in slow motion.
I checked the inactive ingredients. The one that worked had lactose. The ones that didn’t? Magnesium stearate and talc. I didn’t even know those could affect absorption until I read this. Now I only take the brand or the authorized generic. My insurance hates it. But my thyroid doesn’t care about their budget.
Doctors need to stop assuming ‘equivalent’ means ‘identical.’ It doesn’t. And pharmacists? They’re just following scripts. We need better labeling. Mandatory disclosure. Not optional.
Katie O'Connell
December 8, 2025 AT 08:24One must consider the epistemological implications of pharmaceutical equivalence as a construct. The very notion that bioequivalence-measured through plasma concentration curves-is sufficient to guarantee therapeutic equivalence is a reductionist fallacy rooted in positivist scientism. The human organism is not a closed system; it is a dynamic, context-sensitive biological network wherein excipients may modulate bioavailability through gut microbiome interactions, mucosal permeability, and hepatic first-pass metabolism-all variables unaccounted for in FDA protocols.
Furthermore, the regulatory framework presumes homogeneity across patient populations, neglecting pharmacogenomic variability, polypharmacy interactions, and age-related physiological decline. To assert that generics are ‘safe for most’ is not merely inaccurate-it is ethically indefensible when applied to vulnerable cohorts. The data cited herein, while statistically significant, remains insufficient to mitigate the ontological risk posed to those whose lives depend on molecular precision.
Clare Fox
December 9, 2025 AT 03:08so i switched to a generic for my seizure med last year and honestly? felt like a zombie for 3 weeks. couldn’t focus, kept zoning out in meetings. thought it was stress. then i read the label and saw it had a dye i’m allergic to. switched back to brand. boom. normal again.
why is this even a thing? like, if the pill’s the same, why do i feel like someone swapped my brain for a potato?
pharmacies just do it. no warning. no choice. it’s wild.
Akash Takyar
December 10, 2025 AT 08:50Thank you for sharing this important information. In India, we face similar challenges, but with less awareness. Many patients assume generics are identical, and when side effects occur, they blame themselves. I have personally counseled elderly patients who stopped taking their medications because they felt worse after a switch-only to find out it was an inactive ingredient they were intolerant to.
I urge everyone to always check the label, speak to your pharmacist, and never hesitate to request the authorized generic. Your health is priceless. Small steps today can prevent major crises tomorrow.
Arjun Deva
December 12, 2025 AT 00:23THIS IS ALL A LIE. THE FDA IS IN BED WITH BIG PHARMA. THEY LET THE BRANDS MAKE THE GENERIC VERSIONS AND CALL IT ‘AUTHORIZED’ SO THEY CAN CHARGE MORE. THE REAL GENERIC COMPANIES? THEY’RE CHINESE OR INDIAN LABS THAT USE TOXIC FILLERS. THEY’RE POISONING AMERICA. THE DYES? THEY’RE CARRIER FOR 5G SIGNALS. YOU THINK YOUR BRAIN FOG IS FROM LACTOSE? IT’S FROM THE NANOBOTS IN THE TALC.
YOUR ‘AUTHORIZED GENERIC’ IS STILL A TRAP. THEY’RE USING THE SAME MACHINES. THE SAME WORKERS. THE SAME POISON. THEY JUST PUT A DIFFERENT LABEL ON IT. DON’T TRUST ANYTHING. STOP TAKING PILLS. EAT CUCUMBERS.
Inna Borovik
December 12, 2025 AT 21:37Let’s be real: the 12% of patients who needed dose adjustments? That’s a feature, not a bug. It creates repeat prescriptions. More refills. More revenue. The system isn’t broken-it’s optimized. You think they want you stable? No. They want you cycling through generics until you’re desperate enough to pay for the brand. That’s the business model.
And don’t even get me started on the ‘authorized generic.’ That’s just the brand charging $120 instead of $80 and calling it a ‘discount.’ Same pill. Same factory. Same profit margin. The only thing that changed? The label. And your trust.
This isn’t about safety. It’s about monetizing uncertainty.
Jackie Petersen
December 13, 2025 AT 14:39So now we’re supposed to trust some Indian lab to make our heart meds? LOL. I’ve seen the videos. Workers in flip-flops, no gloves, dumping chemicals into vats. This isn’t medicine-it’s a biohazard. We need to ban ALL foreign generics. Make them all in America. Or go back to paying for the brand. I’d rather pay more than die because some guy in Bangalore used expired starch.
Also, ‘authorized generic’? Sounds like a scam to make you feel better while they still screw you. Big Pharma wins either way.
Annie Gardiner
December 13, 2025 AT 20:42Wait-so you’re saying the FDA is lying about generics being ‘equivalent’? But I thought they were the experts? Like, aren’t they the ones who gave us the green light on Vioxx? And OxyContin? And now this? I’m starting to think the whole system is a pyramid scheme where the only winners are the CEOs and the losers are the people who still believe in science.
Also, why is it always ‘some people’ who have problems? Why not just say: ‘This drug doesn’t work the same for everyone, so stop switching it’? That’s what I’d do if I were in charge.
Rashmi Gupta
December 14, 2025 AT 20:52Everyone here is acting like this is new. In India, we’ve been using generics for 30 years. People switch brands every month. No one keeps track. No one complains. You think your body is special? It’s not. You’re just used to paying $200 for a pill. Try living on $2.
Also, ‘authorized generic’? That’s just a marketing trick. The real generic is cheaper for a reason-it works better. Less filler means more active ingredient. You’re not being poisoned. You’re being overdosed by the brand.
Andrew Frazier
December 15, 2025 AT 09:27Ugh. Another ‘poor me’ post. You want the brand? Pay for it. Don’t cry because your insurance saved you $15. The system works. Most people don’t notice a difference. Stop being fragile. You think your thyroid is delicate? My grandma took three different generics for 15 years and still ran marathons. You’re not special.
Also, ‘lactose intolerance’? That’s a made-up trend. You’re just gluten-free and vegan now too, right? Grow up.
Kumar Shubhranshu
December 16, 2025 AT 07:31Switched generic. Felt weird. Asked pharmacist. Said no difference. Checked label. Lactose. Allergic. Switched back. Done.
Simple.
Mayur Panchamia
December 16, 2025 AT 17:40THIS IS WHY AMERICA IS FALLING APART! WE LET CORPORATIONS CUT CORNERS AND NOW OUR KIDS ARE ON 12 PILLS A DAY BECAUSE THE GENERIC MADE THEM SICK! I SAW A MAN IN THE PHARMACY CRYING BECAUSE HIS ASTHMA INHALER DIDN’T WORK! AND THE PHARMACIST JUST SMILED AND SAID ‘IT’S CHEAPER!’
WE NEED A REVOLUTION. NO MORE FOREIGN PILLS. NO MORE ‘AUTHORIZED’ LIES. NO MORE ‘EQUIVALENT’ BULLSHIT. WE DESERVE THE BRAND. WE PAID FOR IT. WE DESERVE THE REAL THING.
IF YOU’RE NOT ANGRY, YOU’RE NOT PAYING ATTENTION.
Karen Mitchell
December 18, 2025 AT 05:38It is imperative to underscore that the current regulatory paradigm is predicated upon an outdated, mechanistic model of pharmacokinetics-one that fails to account for the nuanced, individualized biological variability inherent in human physiology. The conflation of bioequivalence with therapeutic equivalence constitutes a profound epistemic error, one that has been systematically perpetuated by institutional inertia and economic expediency.
Furthermore, the normalization of substitution without patient consent represents a violation of the fundamental tenets of informed autonomy. One cannot consent to a change in formulation if one is unaware that a change has occurred. This is not merely a medical issue. It is a moral failure.