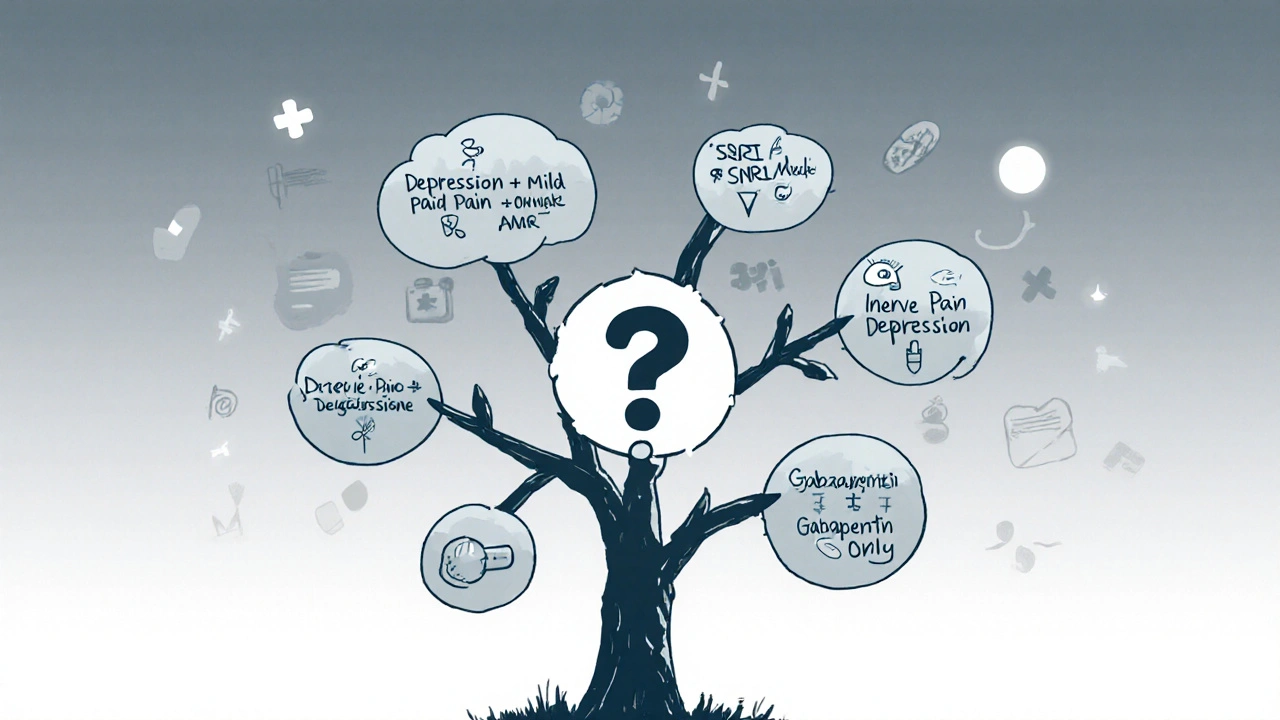
Medication Decision Tool
Your Symptoms
If you’re taking amitriptyline for depression, chronic pain, or trouble sleeping, you’ve probably wondered: is there something better? Maybe the side effects are too much. Maybe it’s not helping enough. Or maybe you’ve heard about newer options and want to know if they’re worth switching to.
Amitriptyline is an old drug-first approved in the 1960s-and it still gets prescribed today. But medicine has changed. We now have treatments that work just as well, with fewer side effects. The question isn’t whether amitriptyline works-it does. The real question is: is it still the best choice for you?
What Amitriptyline Actually Does
Amitriptyline is a tricyclic antidepressant (TCA). It works by boosting serotonin and norepinephrine in the brain-two chemicals tied to mood, pain signals, and sleep. It’s not just for depression. Doctors use it off-label for migraines, fibromyalgia, irritable bowel syndrome, and insomnia.
But here’s the catch: it hits every receptor it can find. That’s why it helps with pain and sleep-but also causes dry mouth, weight gain, drowsiness, constipation, and blurry vision. In older adults, it can raise the risk of falls and confusion. A 2023 Canadian study found that nearly 40% of patients over 65 stopped amitriptyline within six months because of side effects.
SSRIs: The Most Common Alternative
Fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro) are all SSRIs-selective serotonin reuptake inhibitors. Unlike amitriptyline, they mostly target serotonin, leaving other systems alone. That means fewer side effects.
For depression, studies show SSRIs work just as well as amitriptyline. A 2022 meta-analysis in The Lancet Psychiatry found no meaningful difference in effectiveness between amitriptyline and SSRIs for moderate to severe depression. But SSRIs had 30% fewer dropouts due to side effects.
SSRIs don’t help with nerve pain as well as amitriptyline. If your main issue is diabetic neuropathy or post-shingles pain, SSRIs won’t cut it. But if you’re dealing with depression and anxiety-with mild pain-SSRIs are a cleaner first choice.
SNRIs: The Middle Ground
Duloxetine (Cymbalta) and venlafaxine (Effexor) are serotonin-norepinephrine reuptake inhibitors. They hit both chemicals like amitriptyline-but more selectively. That’s why they’re approved for depression, anxiety, and chronic pain.
For fibromyalgia and nerve pain, duloxetine is actually preferred over amitriptyline in many guidelines. A 2024 review in Canadian Family Physician found duloxetine improved pain scores by 30-40% in patients with neuropathic pain, similar to amitriptyline but with less drowsiness and weight gain.
SNRIs can still cause nausea, increased blood pressure, and insomnia-especially at first. But they’re easier to tolerate long-term than amitriptyline. If you’re struggling with both pain and low mood, an SNRI might be your best bet.
Gabapentin and Pregabalin: For Nerve Pain Only
If your main goal is to reduce burning, tingling, or shooting pain-not depression-then gabapentin (Neurontin) or pregabalin (Lyrica) are stronger options.
These drugs calm overactive nerves. They’re not antidepressants, but they’re often used together with low-dose amitriptyline for stubborn pain. Studies show pregabalin reduces pain by 50% or more in about half of patients with diabetic neuropathy. Amitriptyline does the same, but with more sedation.
The downside? Gabapentin and pregabalin can cause dizziness, swelling in the legs, and weight gain. They’re not for everyone. But if you’re not depressed and just want pain relief, they’re often better than amitriptyline.
Mirtazapine: Sleep and Appetite Focus
Mirtazapine (Remeron) is another antidepressant that’s popular for people who can’t sleep or have lost their appetite. It works differently-blocking certain receptors to boost serotonin and norepinephrine indirectly.
It’s very sedating, so it’s often taken at night. Many patients report falling asleep faster and sleeping more deeply. It also increases appetite, which helps people who’ve lost weight due to depression.
But it causes weight gain in up to 60% of users. If you’re already overweight or have diabetes, this can be a problem. It doesn’t help with nerve pain as well as amitriptyline. But if your biggest issues are insomnia and low appetite, mirtazapine is a solid alternative.
TCAs Other Than Amitriptyline
Not all tricyclics are the same. Nortriptyline and desipramine are metabolites of amitriptyline-meaning they’re similar but cleaner.
Nortriptyline, for example, causes less drowsiness and has fewer anticholinergic effects (dry mouth, constipation). It’s often used when amitriptyline is too strong. Studies show it’s just as effective for depression and nerve pain, with better tolerability.
Desipramine is even more selective for norepinephrine. It’s less sedating and sometimes used when patients can’t handle the sleepiness of amitriptyline. But it’s harder to find and more expensive in some regions.
What About Newer Options? CBT, CBD, and Exercise
Medication isn’t the only tool. Cognitive behavioral therapy (CBT) for chronic pain and depression has been shown to be as effective as amitriptyline in multiple trials. A 2023 study in JAMA Psychiatry found that 12 weeks of CBT reduced pain and depressive symptoms by the same amount as amitriptyline-with no side effects.
Exercise, even walking 30 minutes a day, boosts serotonin and endorphins. It’s not a replacement, but it’s a powerful add-on. One study showed patients who combined exercise with medication had 50% better outcomes than those on medication alone.
CBD oil is popular, but evidence is weak. A 2025 review by the Canadian Pain Society found no high-quality proof that CBD helps with depression or neuropathic pain better than placebo. Skip it unless you’re using it for anxiety, and even then, stick to regulated products.
When to Stick With Amitriptyline
It’s not all bad. Amitriptyline is cheap-often under $10 a month in Canada. It’s one of the few drugs proven to help with chronic insomnia linked to depression. And for some people, especially those who’ve tried everything else, it’s the only thing that works.
If you’ve been on it for years without side effects and it’s helping, don’t rush to switch. But if you’re new to it, or if you’re struggling with side effects, it’s worth exploring alternatives.
How to Decide What’s Right for You
Here’s a simple decision guide:
- Primary issue: Depression + mild pain? Try an SSRI like sertraline.
- Primary issue: Nerve pain + depression? Try duloxetine or nortriptyline.
- Primary issue: Insomnia + low appetite? Try mirtazapine.
- Primary issue: Pain only? Try pregabalin or gabapentin.
- Already on amitriptyline with side effects? Ask about switching to nortriptyline.
- Want to avoid meds? Try CBT + daily walking for 8 weeks.
Never stop amitriptyline cold turkey. It can cause withdrawal symptoms like nausea, dizziness, and brain zaps. Always taper slowly under medical supervision.
Final Thoughts
Amitriptyline isn’t obsolete. But it’s no longer the first-line choice for most people. We have safer, more targeted options now. The goal isn’t to find the strongest drug-it’s to find the one that helps you feel better without making you feel worse.
If you’re on amitriptyline and unhappy, talk to your doctor. Ask about nortriptyline, duloxetine, or CBT. There’s a good chance you can get the same relief-with fewer side effects.
Is amitriptyline still a good option for depression?
Yes, but usually not as a first choice. Amitriptyline works for depression, but newer drugs like SSRIs and SNRIs have fewer side effects and are easier to tolerate. It’s still used when other options fail, or when a patient also has chronic pain or severe insomnia.
What’s the safest alternative to amitriptyline for nerve pain?
Duloxetine (Cymbalta) and pregabalin (Lyrica) are both preferred over amitriptyline for nerve pain in current guidelines. Duloxetine also helps with depression, while pregabalin is better if pain is your only concern. Both cause fewer sedative side effects than amitriptyline.
Can I switch from amitriptyline to an SSRI on my own?
No. Stopping amitriptyline suddenly can cause withdrawal symptoms like dizziness, nausea, and electric shock sensations. Always work with your doctor to taper off slowly, then start the new medication gradually. Switching too fast can make symptoms worse.
Does amitriptyline cause weight gain?
Yes, it’s one of the most common side effects. Up to 50% of users gain weight, often 5-10 pounds or more within the first few months. This is due to increased appetite and slower metabolism. If weight gain is a concern, nortriptyline or an SNRI like duloxetine may be better options.
How long does it take for amitriptyline alternatives to work?
Most antidepressants and pain meds take 4-6 weeks to show full effects. Some people feel slight improvements in sleep or mood within 1-2 weeks, but it usually takes longer. Don’t give up too soon. If there’s no change after 8 weeks, talk to your doctor about adjusting the dose or trying something else.

Sonia Festa
November 2, 2025 AT 00:06amitriptyline is basically the medical equivalent of using a sledgehammer to open a jelly jar - it works, but you’re gonna make a mess and feel weird afterward. i switched to duloxetine and suddenly i could actually walk without feeling like i was stuffed in a pillowcase. also, no more ‘why is my tongue stuck to the roof of my mouth’ mornings. 🙌
Sara Allen
November 2, 2025 AT 01:14sooo... are you saying the pharmaceutical companies are just pushing these new drugs because they make more money?? like, why would they stop selling amitriptyline if it's so cheap?? i think the FDA is in bed with big pharma and they're hiding the truth. also, i heard the moon landing was faked so... who knows what's real anymore?? 😵💫
Ryan Tanner
November 4, 2025 AT 00:37if you’re on amitriptyline and it’s working, don’t fix it. but if you’re struggling? try nortriptyline. it’s like amitriptyline’s chill cousin who doesn’t crash your system. also, walking 30 mins a day? game changer. i did it for 8 weeks and my sleep and mood improved without a single pill. 🚶♂️💪
Nishigandha Kanurkar
November 4, 2025 AT 14:50THIS IS ALL A LIE!!! AMITRIPTYLINE IS THE ONLY THING THAT WORKS BECAUSE THE GOVERNMENT AND THE PHARMA COMPANIES ARE USING 5G TO CONTROL OUR BRAINS AND THEY WANT US TO TAKE SSRIs SO THEY CAN TRACK OUR MOODS THROUGH OUR TOILET SEATS!!! I’VE SEEN THE DOCUMENTS!!! THEY’RE HIDING THE TRUTH IN THE FOOTNOTES OF THE LANCET!!!
Emily Barfield
November 5, 2025 AT 19:52Is the pursuit of ‘better’ in medicine just a reflection of our cultural impatience? We want relief without consequence, efficacy without sacrifice. Amitriptyline, for all its brutality, demands surrender - it asks you to feel the weight of your own biology. Are we too afraid of that weight now? Do we mistake gentleness for healing? Or is this just evolution - a slow, messy, chemical recalibration of what we’re willing to endure to feel ‘normal’?
And yet… if ‘normal’ is just another word for ‘less broken,’ then perhaps the real question isn’t which drug works - but which version of ourselves we’re willing to become.
John Rendek
November 6, 2025 AT 11:22For anyone considering a switch: talk to your doctor. Taper slowly. Don’t rush. Nortriptyline is a solid middle ground if amitriptyline is too harsh. And CBT? It’s not magic, but it’s free and doesn’t make you feel like a zombie. Combine it with walking. You’ll be surprised.
Jessica Adelle
November 7, 2025 AT 02:52It is both alarming and profoundly irresponsible to suggest that any patient should abandon a proven, time-tested therapeutic agent in favor of newer, commercially promoted alternatives whose long-term safety profiles remain inadequately studied. The erosion of clinical wisdom in favor of marketing-driven protocols is a direct consequence of neoliberal healthcare policy. One must ask: who benefits from this shift? Not the patient. Not the physician. Only the shareholder.
Vrinda Bali
November 8, 2025 AT 01:24It is not merely a question of pharmacology - it is a question of societal decay. We have replaced discipline with convenience, endurance with pharmaceutical pacification. Amitriptyline, despite its side effects, forces the body to confront its own imbalance. The modern alternatives? They are sedatives disguised as solutions. We have become a civilization that fears discomfort more than disease. And now, we medicate our souls into silence.
Where is the courage to endure? Where is the wisdom to suffer with grace? We have traded resilience for a pill - and we wonder why we feel emptier than before.
Amina Kmiha
November 8, 2025 AT 21:18Ok but have you seen the CDC’s secret database on TCA withdrawal? 😳 I found it on a .onion site. Amitriptyline doesn’t just cause brain zaps - it creates neural scars that make you susceptible to AI mind control. That’s why they want you on SSRIs - they’re easier to hack. Also, the weight gain? It’s not the drug. It’s the glyphosate in your coffee. 🌱⚡
Ted Carr
November 9, 2025 AT 05:00So you’re telling me the answer to depression is… walking? And CBT? Wow. I guess we could’ve just skipped 60 years of pharmaceutical innovation and told everyone to go outside and think about their feelings. Genius. 🤡
Rebecca Parkos
November 10, 2025 AT 17:41I was on amitriptyline for 3 years. Weight gain, dry mouth, felt like a zombie at work. Switched to duloxetine - same pain relief, zero brain fog. I cried the first morning I woke up without feeling like I’d been hit by a truck. Thank you for this post. I needed to hear someone say it’s okay to switch.
Ryan Tanner
November 11, 2025 AT 20:02That’s so good to hear, Rebecca. Seriously - if you’re feeling better, that’s the real win. No drug is sacred. If it’s not serving you, it’s time to try something else. You’re not failing - you’re adapting. 🙏
Sai Ahmed
November 12, 2025 AT 18:31the real issue is that doctors don't care. they just prescribe what's on the formulary. i asked for nortriptyline and they said 'we don't stock it.' so i had to pay $200 out of pocket. meanwhile, amitriptyline is free. this isn't medicine. it's corporate roulette.
Iván Maceda
November 13, 2025 AT 16:40As an American, I just want to say: we’ve got better options now. Why cling to a 60-year-old drug when we’ve got science on our side? 🇺🇸💊 It’s not about patriotism - it’s about progress. Let’s stop romanticizing outdated medicine. We’re not living in 1965 anymore.