What Is Sick Euthyroid Syndrome?
When you’re seriously ill, your body doesn’t just feel tired-it changes how it uses energy. One of the quietest, most misunderstood shifts happens in your thyroid hormone levels. Sick euthyroid syndrome (also called nonthyroidal illness syndrome) is when your thyroid blood tests look abnormal, but your thyroid gland itself is perfectly fine. It’s not a disease. It’s your body adapting.
This isn’t rare. In fact, up to 75% of people in intensive care units show these abnormal thyroid numbers. You might see low T3, low T4, or high reverse T3-and your doctor might think you have hypothyroidism. But if you’re fighting sepsis, recovering from major surgery, or battling severe burns, those numbers are a normal reaction to stress, not a sign your thyroid is broken.
How Illness Changes Thyroid Hormones
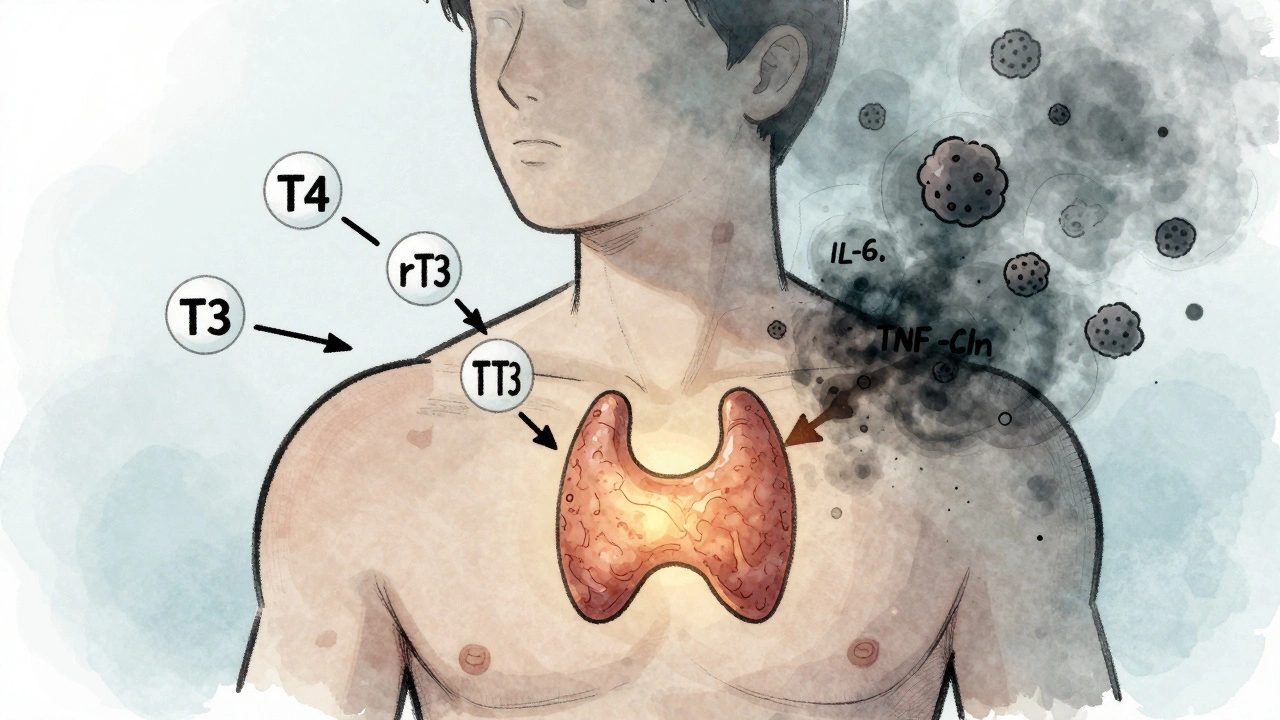
Your thyroid makes two main hormones: T4 (thyroxine) and T3 (triiodothyronine). T4 is mostly a storage form. Your body converts T4 into T3, the active hormone that tells your cells how fast to burn energy. In sick euthyroid syndrome, this conversion breaks down.
During severe illness, your body reduces the activity of an enzyme called type 1 deiodinase. That means less T4 turns into T3. At the same time, your body starts making more reverse T3 (rT3), which is inactive and blocks T3 from working. Studies show rT3 rises in 85-90% of cases. Your T4 levels may also drop, especially if you’ve been sick for days or weeks.
Thyroid-stimulating hormone (TSH), the signal from your brain telling your thyroid to produce more hormones, usually stays normal. That’s the biggest clue. If your TSH is normal but your T3 and T4 are low, it’s almost certainly sick euthyroid syndrome. Sometimes TSH dips slightly or even rises a little during recovery-but it rarely goes high enough to suggest primary hypothyroidism.
Why Your Body Does This
This isn’t a malfunction. It’s a survival tactic. When you’re critically ill, your body needs to conserve energy. Slowing down your metabolism helps redirect resources to healing, fighting infection, and keeping your heart and brain running.
Studies show that lowering T3 reduces metabolic rate by 15-20%. That might sound bad, but in sepsis or major trauma, it can actually help you survive. Inflammation plays a big role here. Cytokines like interleukin-6 and tumor necrosis factor-alpha surge during illness and directly suppress the thyroid axis. These aren’t side effects-they’re intentional signals.
Think of it like putting your car in neutral during a breakdown. You’re not fixing the engine, but you’re not wasting fuel either. Your body is doing the same thing.
Which Illnesses Trigger It?
Sick euthyroid syndrome shows up in almost every major illness that stresses the body. The most common triggers include:
- Sepsis (80-85% of cases)
- Major surgery (65-70%)
- Severe burns (75-80%)
- Heart attack (50-55%)
- Diabetic ketoacidosis (60-65%)
- Chronic liver disease like cirrhosis (70-75%)
- Chronic kidney failure (60-65%)
- Severe anorexia nervosa (up to 90%)
It can develop within 24 to 48 hours after the illness starts. That’s why you might see abnormal thyroid labs early in your hospital stay-even if you’ve never had thyroid problems before.

Symptoms That Look Like Hypothyroidism (But Aren’t)
If you’re sick and your labs show low T3 and T4, you might feel like you have hypothyroidism: tired, cold, constipated, weak. Those symptoms are real-but they’re caused by your illness, not your thyroid.
The key difference? People with true hypothyroidism have signs like dry skin, puffy face, slow reflexes, or elevated thyroid antibodies. In sick euthyroid syndrome, those signs are absent. You won’t have myxedema (swelling under the skin) or a goiter. Your antibodies will be normal. Your symptoms improve as you recover from the main illness-not because you took thyroid pills, but because your body healed.
In the most severe cases, patients can develop hypothermia (body temp below 35°C), slow breathing, low blood pressure, or even coma. These aren’t thyroid problems-they’re signs of multi-organ failure. Treating them with thyroid hormone won’t help.
Why You Shouldn’t Take Thyroid Pills for This
This is the most important point: you do not need thyroid hormone replacement for sick euthyroid syndrome.
Doctors sometimes mistake it for hypothyroidism and prescribe levothyroxine. But multiple studies show this does nothing-and might even hurt you. A 2022 trial with 450 ICU patients found no difference in death rates or ICU stay length between those given thyroid hormone and those given a placebo.
Another study in JAMA Internal Medicine found that 12% of ICU patients were incorrectly treated with thyroid meds because their labs were misread. Those patients had worse outcomes. Why? Extra thyroid hormone forces your body to burn energy faster when it should be conserving it. It can raise heart rate, increase oxygen demand, and stress an already weakened heart.
The American Thyroid Association and Endocrine Society both say: don’t treat ESS. Treat the illness.
How Doctors Tell the Difference
Getting the diagnosis right is critical. Here’s how they do it:
- Normal TSH + low T3/T4 → Likely sick euthyroid syndrome
- Low TSH + low T3/T4 → Could be central hypothyroidism (rare, needs treatment)
- High TSH + low T4 → Primary hypothyroidism (needs treatment)
- High TSH + normal T4 → Subclinical hypothyroidism (watch, may need treatment)
They also look at your clinical picture. If you’re recovering from pneumonia, your low T3 is probably ESS. If you’ve had a thyroidectomy and now have low T3 and high TSH, that’s different.
Some labs check reverse T3 or thyroid antibodies to help confirm. But in most cases, context is enough.
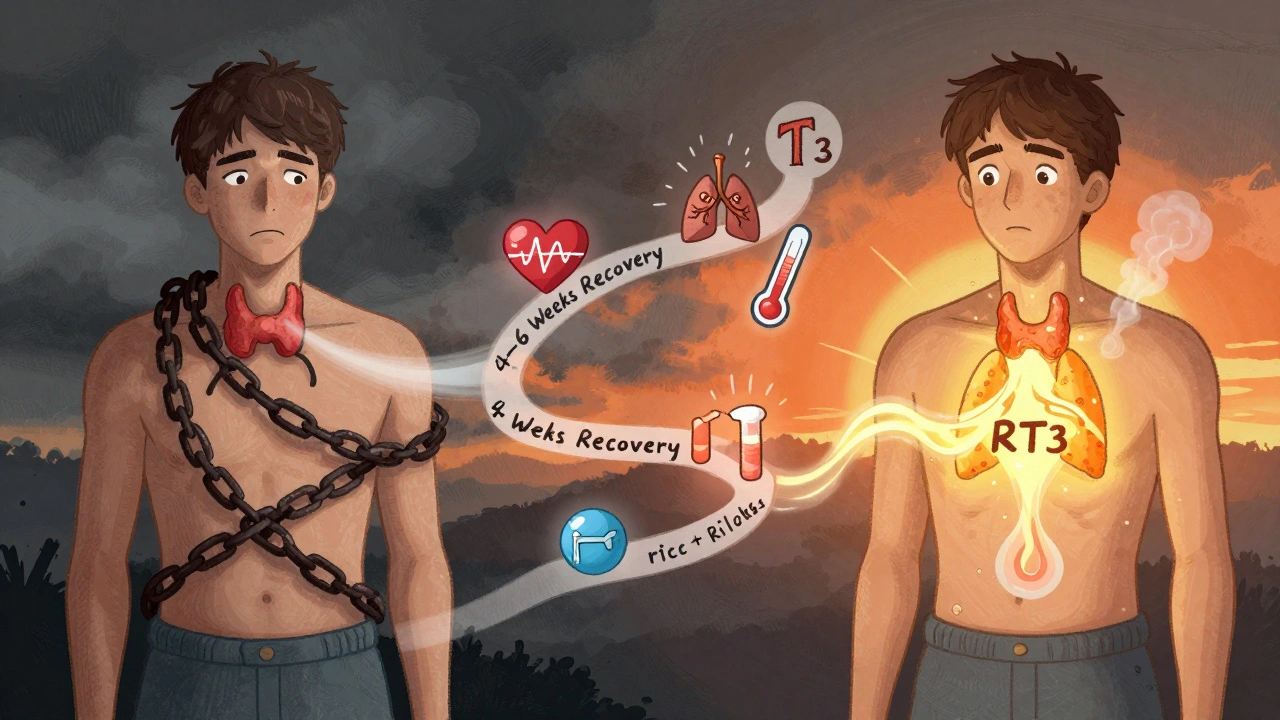
What Happens After You Recover?
Once the illness resolves, your thyroid numbers usually bounce back on their own. That’s why experts recommend waiting 4 to 6 weeks after you’re well before retesting thyroid function.
If your T3 and T4 are still low after recovery, that could mean you have an underlying thyroid problem that was masked by illness. That’s rare-but important to catch. Follow-up testing is the only way to know for sure.
What’s New in Research?
Scientists are now looking at whether the degree of T3 drop can predict how sick you’ll get. One study found that patients with T3 below 40 ng/dL had a 45% chance of dying in the ICU. Those with T3 above 80 ng/dL had only a 15% risk. That’s not a diagnostic tool yet-but it might one day help doctors spot high-risk patients faster.
A large study called EUTHYROID-ICU, running from 2023 to 2025, is tracking 2,500 critically ill patients to see if specific patterns in thyroid hormones can predict recovery. Early data suggests certain hormone shifts might help identify who will improve quickly and who needs more aggressive care.
Bottom Line
Sick euthyroid syndrome isn’t a thyroid problem. It’s your body’s smart way of surviving a crisis. Your labs might look broken, but your thyroid isn’t. Taking thyroid pills won’t fix it-and could make things worse.
If you’re hospitalized or recovering from a serious illness and your thyroid tests come back abnormal, ask: "Is this because of my illness, or is my thyroid actually failing?" The answer matters. Trust your doctor to look at the whole picture-not just the numbers.
Emily Haworth
December 14, 2025 AT 08:25Deborah Andrich
December 16, 2025 AT 05:19kevin moranga
December 18, 2025 AT 00:30Yatendra S
December 18, 2025 AT 19:49Himmat Singh
December 20, 2025 AT 10:03Keasha Trawick
December 20, 2025 AT 19:54Webster Bull
December 22, 2025 AT 14:06Jamie Clark
December 24, 2025 AT 09:56Tyrone Marshall
December 24, 2025 AT 11:39Bruno Janssen
December 25, 2025 AT 12:29Emma Sbarge
December 27, 2025 AT 01:05Tom Zerkoff
December 27, 2025 AT 13:57