What really causes type 2 diabetes?
Most people think type 2 diabetes is just about high blood sugar. But that’s the symptom, not the cause. The real story starts years before your fasting glucose hits 100 mg/dL - with something called insulin resistance. It’s when your muscle, fat, and liver cells stop listening to insulin, the hormone that tells them to soak up glucose from your blood. Instead of glucose being used for energy, it piles up in your bloodstream. Your pancreas responds by pumping out more insulin. At first, it works. But over time, the beta cells burn out. That’s when you cross the line from prediabetes into full-blown type 2 diabetes.
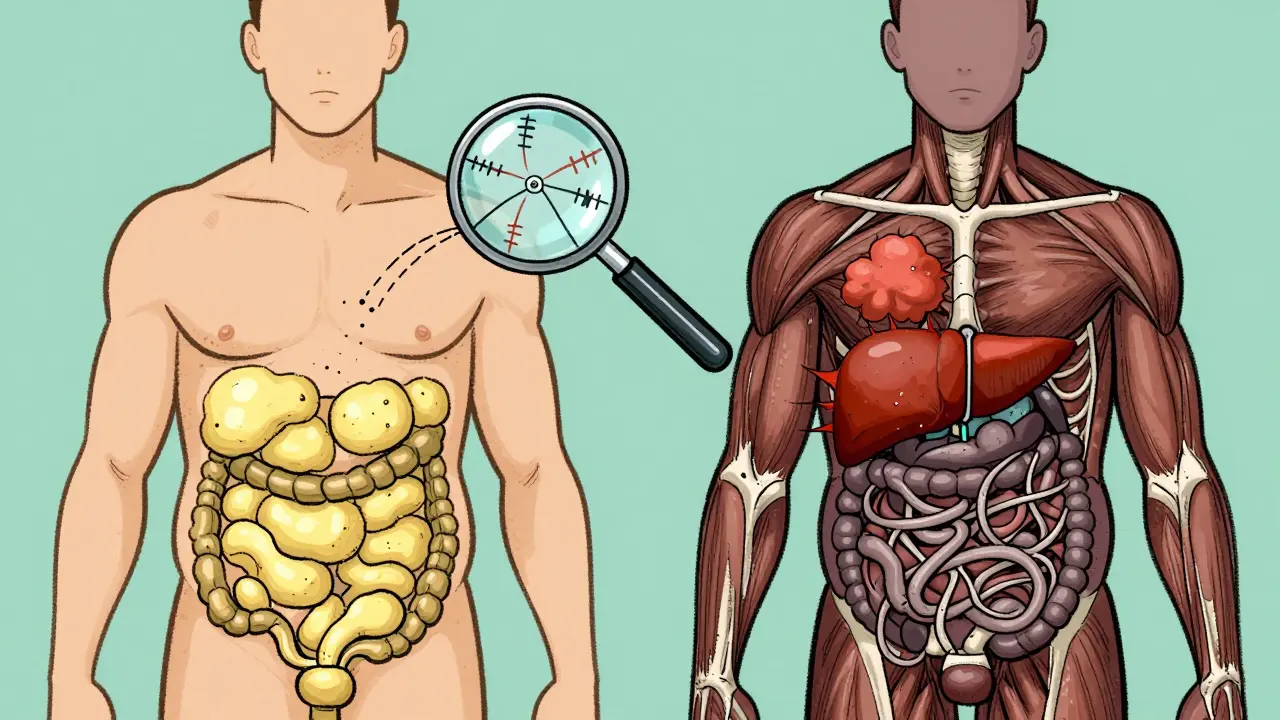
This isn’t just a sugar problem. It’s a whole-system failure. And it’s tied to something called metabolic syndrome - a cluster of conditions that don’t just raise your diabetes risk, but also your chance of heart attack, stroke, and liver disease. The old term “metabolic syndrome” is being replaced by “metabolic dysfunction syndrome” (MDS) in medical circles because it better reflects what’s actually happening: your metabolism is breaking down, not just acting oddly.
Insulin resistance: The silent engine behind the disease
Insulin resistance doesn’t come out of nowhere. It’s fueled by decades of excess. When you eat more calories than your body needs - especially from refined carbs and sugars - your liver and fat cells get flooded with glucose and fatty acids. These overload the cells’ energy systems, triggering inflammation and stress inside the cell. The insulin signaling pathway - the chain reaction that tells cells to take in glucose - starts to break down. Key proteins like IRS-1 and Akt2 stop working properly. Your cells become numb to insulin’s signal.
What’s worse, the fat doesn’t just sit under your skin. It builds up where it shouldn’t - inside your liver (nonalcoholic fatty liver disease), inside your muscles, and around your organs. This is called ectopic fat. And it’s far more dangerous than belly fat alone. That’s why two people with the same BMI can have wildly different diabetes risks. One has fat stored safely under the skin; the other has fat clogging their liver and muscles. The latter is far more likely to develop insulin resistance.
Studies show that 80 to 90% of people with type 2 diabetes have significant insulin resistance before diagnosis. Dr. Ralph DeFronzo, who first mapped this mechanism in the 1970s, calls it the “single most important defect” leading to diabetes. Even people who aren’t overweight can have it - especially those of South Asian descent - because genetics influence where fat gets stored.
Metabolic syndrome: When the body starts to unravel
Metabolic syndrome isn’t a diagnosis you get from one lab test. It’s a pattern. The International Diabetes Federation says you have it if you have at least three of these five things:
- Waist size over 94 cm for men in Europe, 90 cm for South Asian and East Asian men, and 80 cm for women of all these groups
- Triglycerides above 150 mg/dL
- HDL cholesterol below 40 mg/dL for men or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
These aren’t random numbers. They’re signs of the same underlying problem: insulin resistance. High triglycerides? Your liver is dumping fat into your blood because it can’t process glucose properly. Low HDL? Insulin messes with the enzymes that make good cholesterol. High blood pressure? Insulin makes your kidneys hold onto salt and water. And that elevated fasting glucose? That’s your pancreas losing the battle.
Having metabolic syndrome doesn’t just mean you’re at risk for diabetes. It means your heart is already under attack. Mayo Clinic data shows people with metabolic syndrome have 2 to 3 times the risk of heart disease compared to those without any of the five components. And if you have nonalcoholic fatty liver disease (NAFLD) on top of it? Your chance of developing type 2 diabetes doubles.
Prediabetes vs. type 2 diabetes: The tipping point
Prediabetes is when your blood sugar is high, but your pancreas is still trying to keep up. Fasting glucose is between 100 and 125 mg/dL. You’re insulin resistant, but your beta cells are still producing enough insulin to keep you out of diabetes. That’s why many people with prediabetes feel fine - no symptoms, no diagnosis, no treatment.
But over time, the beta cells wear out. They lose about 4 to 5% of their function every year. That’s not a slow decline - it’s a countdown. Once they can’t produce enough insulin to overcome resistance, your blood sugar spikes past 126 mg/dL fasting or 200 mg/dL after eating. That’s type 2 diabetes. The transition isn’t sudden. It’s a slow leak. And by the time you’re diagnosed, you’ve already lost 50 to 70% of your beta cell function.
The Diabetes Prevention Program (DPP) proved this. People with prediabetes and metabolic syndrome had a 5 to 6 times higher risk of developing type 2 diabetes than those without. But those who lost just 7% of their body weight and walked 150 minutes a week cut their risk by 58% over three years. That’s not magic. That’s reversing insulin resistance.
What actually works to reverse insulin resistance
There’s no pill that fixes insulin resistance. But lifestyle changes do - if they’re specific and sustained.
Weight loss matters - but not how you think. Losing 5 to 7% of your body weight is enough to dramatically improve insulin sensitivity. For someone weighing 200 pounds, that’s 10 to 14 pounds. It doesn’t have to be dramatic. The Look AHEAD trial showed that people who lost 10% of their weight at one year had a 51% chance of partial diabetes remission. Twelve percent were still in remission eight years later.
Exercise isn’t optional - it’s medicine. Just one session of moderate activity - like brisk walking - can make your muscles more sensitive to insulin for up to 48 hours. That’s why 150 minutes a week is the minimum. Strength training helps, too. Muscle is the biggest consumer of glucose. More muscle = better glucose control.
Diet isn’t about cutting carbs - it’s about quality. Refined carbs and sugary drinks spike blood sugar and insulin, worsening resistance. Whole grains, vegetables, legumes, nuts, and lean proteins don’t. The Mediterranean diet, rich in olive oil, fish, and fiber, has been shown to improve insulin sensitivity better than low-fat diets. You don’t need to go keto. You need to stop eating food that makes your body scream for insulin.
Medications help, but they’re not the answer. Metformin - the first-line drug for prediabetes - reduces diabetes risk by 31%. GLP-1 agonists like semaglutide and tirzepatide are game-changers. They don’t just lower blood sugar - they reduce appetite, promote weight loss (up to 15% on average), and even protect beta cells. In the SELECT trial, 66% of people on semaglutide achieved diabetes remission. But these drugs work best when paired with lifestyle change. They’re tools, not replacements.

The future: New science, new hope
Researchers are no longer treating diabetes as a single disease. They’re seeing it as a spectrum - with insulin resistance at the core. The European Association for the Study of Diabetes plans to officially adopt “metabolic dysfunction syndrome” by late 2025. That means doctors will start diagnosing the problem earlier - before blood sugar rises.
Stem cell therapies are showing promise. Vertex Pharmaceuticals’ VX-880 replaces destroyed beta cells with lab-grown ones. In early trials, 71% of patients stopped needing insulin after one year. Continuous glucose monitors (CGMs) like the Dexcom G7 are now FDA-approved for non-diabetic use. People with prediabetes can track how their meals affect their blood sugar in real time - making lifestyle changes personal and immediate.
The big shift? From treating high blood sugar to fixing insulin resistance. Because once you fix that, everything else follows. Blood pressure drops. Triglycerides fall. HDL rises. Liver fat shrinks. The heart gets a break. And the risk of diabetes? It doesn’t just go down - it can vanish.
What you can do today
If you’re overweight, have high blood pressure, or your last blood test showed elevated fasting glucose - don’t wait. You’re not doomed. You’re in the window where change still works.
- Get your waist measured. If you’re a man over 90 cm or a woman over 80 cm, you’re at risk.
- Ask your doctor for a fasting glucose and HbA1c test. If your HbA1c is above 5.7%, you have prediabetes.
- Start walking 30 minutes a day, five days a week. No gym needed.
- Swap soda for water. Swap white bread for whole grain. Swap fried chicken for grilled fish.
- If you’re on metformin or a GLP-1 agonist, don’t skip the lifestyle work. The drugs amplify your effort - they don’t replace it.
Insulin resistance isn’t your fault. But fixing it? That’s in your hands. And the science is clear: you can reverse it. Not just delay it. Not just manage it. Reverse it. Before it becomes something you can’t undo.
Can you reverse type 2 diabetes?
Yes - in many cases. When insulin resistance is reversed through weight loss, diet, and exercise, the pancreas can recover enough function to bring blood sugar back to normal without medication. This is called remission. Studies show up to 66% of people on GLP-1 agonists and intensive lifestyle changes achieve remission within a year. But it’s not permanent unless the lifestyle changes stick.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome is a group of five risk factors - including high blood sugar - that point to insulin resistance. You can have metabolic syndrome without prediabetes (if you have three other components). And you can have prediabetes without full metabolic syndrome. But they almost always go together.
Why do some thin people get type 2 diabetes?
Because insulin resistance isn’t just about weight - it’s about fat distribution. Thin people can have high levels of visceral fat (around organs) or fatty liver, especially if they have genetic risk factors. This is common in South Asian populations. Even with a normal BMI, if fat is stored inside the liver or muscles, insulin resistance follows.
Does metformin cure insulin resistance?
No. Metformin improves insulin sensitivity by reducing liver glucose production and helping muscles absorb more glucose. It lowers diabetes risk by 31%, but it doesn’t reverse the root cause. Only lifestyle changes - weight loss, exercise, and better food - can truly restore insulin sensitivity. Metformin supports those changes; it doesn’t replace them.
How long does it take to reverse insulin resistance?
You can see improvements in as little as two weeks with consistent exercise and reduced sugar intake. Significant changes - like lower triglycerides, better blood pressure, and improved fasting glucose - usually show up in 3 to 6 months. Full reversal, where medication is no longer needed, can take 1 to 2 years. It’s not fast, but it’s permanent if you keep going.
Are there tests to check for insulin resistance?
There’s no single routine test, but doctors can estimate it. A fasting insulin level above 10 µIU/mL suggests resistance. A high triglyceride-to-HDL ratio (above 3.5) is another clue. HOMA-IR, a calculation using fasting glucose and insulin, is used in research. Most often, doctors diagnose it indirectly - by seeing if you have three or more components of metabolic syndrome.
Holly Robin
January 31, 2026 AT 11:30And don't even get me started on 'exercise' - you think walking 30 minutes fixes decades of corporate lies? Nah. It's the HFCS in your ketchup, your 'low-fat' yogurt, your 'whole grain' bread that's laced with glyphosate. The system is rigged.
KATHRYN JOHNSON
February 2, 2026 AT 02:17Kelly Weinhold
February 3, 2026 AT 22:05You don’t have to be perfect. You just have to show up. And if you’re reading this and feeling overwhelmed? Start with one thing. One meal. One walk. One glass of water instead of soda. You’ve got this. I believe in you.
Kimberly Reker
February 5, 2026 AT 18:43One thing I tell my patients: you don’t need to overhaul your life overnight. Just move more. Eat real food. Sleep better. Those three things alone change everything. And if you’re on metformin? Great. But don’t treat it like a magic pill. It’s a bridge, not a destination.
Also, if you’re thin and have high triglycerides? Yeah, you’re still at risk. Genetics don’t care how you look.
Eliana Botelho
February 6, 2026 AT 00:58Rob Webber
February 7, 2026 AT 23:01calanha nevin
February 8, 2026 AT 15:05For those who feel discouraged: remission is possible. It requires consistency not perfection. Weight loss of 5-7% is sufficient to restore insulin sensitivity in most cases. Exercise improves glucose uptake independent of weight loss. Dietary quality trumps macronutrient ratios.
There is no conspiracy. There is biology. And biology can be influenced.
Lisa McCluskey
February 9, 2026 AT 09:36It wasn’t easy. But it wasn’t impossible either. The hardest part was stopping the guilt. I used to think if I just tried harder, I’d fix it faster. Turns out, progress is slow. And that’s okay. Just keep going.