PML Risk Calculator
Note: Risk values are estimated based on clinical studies and may not reflect individual circumstances. Always discuss with your neurologist.
What Is Progressive Multifocal Leukoencephalopathy (PML)?
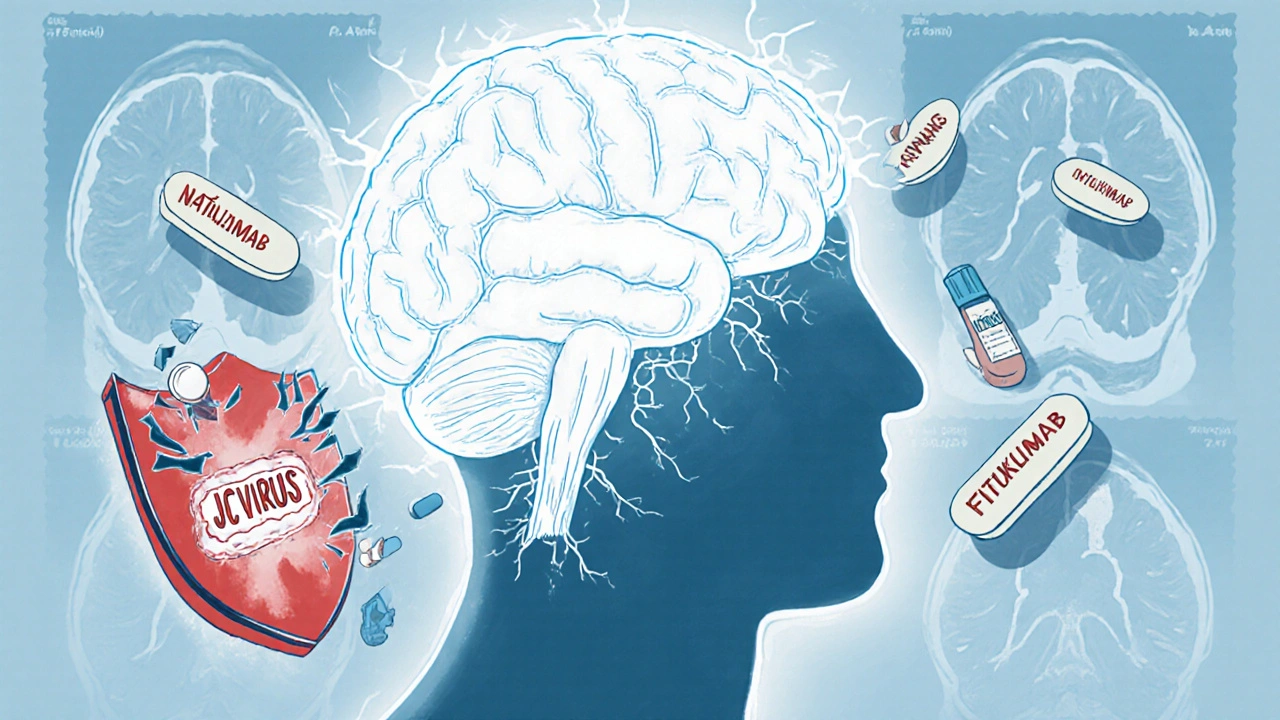
PML is a rare but deadly brain disease caused by the reactivation of the JC virus. Most people carry this virus without knowing it - about 50 to 70% of adults have been exposed. Normally, your immune system keeps it under control. But when you take strong immunosuppressants, that control can break down. The virus starts attacking the white matter of your brain, destroying the fatty coating (myelin) around nerve cells. This leads to irreversible damage, and symptoms can show up fast: weakness on one side of the body, trouble speaking, vision loss, confusion, or loss of coordination. Once symptoms appear, the damage is often already advanced.
Which Immunosuppressants Carry the Highest Risk?
Not all immunosuppressants are created equal when it comes to PML risk. The biggest red flag is natalizumab (Tysabri), used for multiple sclerosis and Crohn’s disease. Among patients on natalizumab, the overall PML risk is about 0.12%, but it jumps dramatically if you have three things: a positive JC virus antibody test, prior use of another immunosuppressant like azathioprine or methotrexate, and treatment lasting more than two years. In that high-risk group, the chance of PML hits 4.1 cases per 1,000 patients.
Other drugs with notable risk include:
- Fingolimod (Gilenya): 0.4 cases per 1,000 patient-years
- Rituximab (Rituxan): 0.8 cases per 1,000 patient-years
- Dimethyl fumarate (Tecfidera): 0.2 cases per 1,000 patient-years
Drugs like interferon beta and glatiramer acetate have never been linked to confirmed PML cases. If you’re on one of the high-risk drugs, knowing your exact risk level isn’t just helpful - it’s critical.
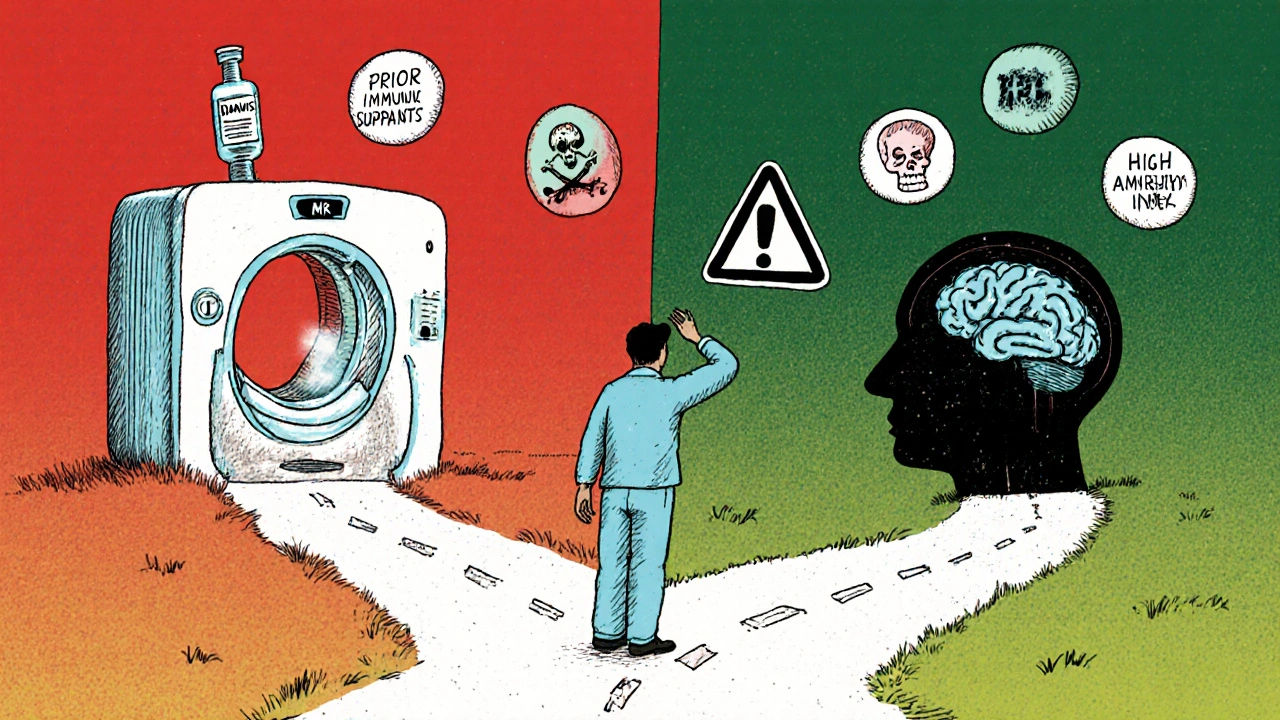
How Is PML Risk Measured?
The main tool doctors use is the JC virus antibody test. It tells you if you’ve ever been exposed to the virus. But it’s not perfect. About 2 to 3% of people who test negative still carry the virus - false negatives happen. That’s why a negative test doesn’t mean zero risk.
For patients on natalizumab, labs also report a JC virus antibody index. This number shows how strong your immune response is to the virus. A low index (below 0.9) means very low risk - under 0.1% over four years. But if your index is above 1.5, your risk jumps to nearly 11% after four years of treatment. That’s why many neurologists stop natalizumab at the 24-month mark for patients with high index values, even if their MS is well-controlled.
Why Prior Immunosuppressant Use Matters
If you’ve ever taken another immunosuppressant before starting natalizumab, your PML risk triples. This isn’t just a small bump - it’s a major red flag. Studies show patients who used drugs like mitoxantrone, azathioprine, or methotrexate before switching to natalizumab have a 2.5 times higher chance of developing PML than those who didn’t. That’s why the FDA now requires doctors to ask: “Have you ever taken an immunosuppressant before?” before prescribing natalizumab. Many patients don’t realize that even a short course of prednisone or cyclophosphamide years ago can count. Your full medication history matters.

What Are the Early Warning Signs?
PML symptoms often mimic MS relapses, which is why so many cases are missed at first. About 37% of early PML cases are wrongly labeled as a flare-up. That’s dangerous. Unlike a typical MS relapse, PML symptoms usually get worse slowly over weeks, not days. Look out for:
- One-sided weakness or numbness
- Slurred speech or trouble finding words
- Blurred or double vision
- Loss of balance or clumsiness
- Changes in thinking, memory, or personality
There’s no single test that catches PML early. That’s why regular brain MRIs are essential. Neurologists recommend scans every 3 to 6 months for high-risk patients. Early PML lesions show up as small, bright spots on diffusion-weighted MRI sequences - something only trained radiologists can spot reliably. It takes 15 to 20 hours of specialized training to tell the difference between an MS plaque and the earliest signs of PML.
What Happens After PML Diagnosis?
Once PML is confirmed, the first step is always stopping the immunosuppressant. But that’s not enough. In 50 to 60% of cases, the immune system comes back too hard and starts attacking the brain itself - this is called IRIS, or immune reconstitution inflammatory syndrome. IRIS can cause swelling, seizures, or even death. Treatment often involves high-dose steroids like methylprednisolone to calm the overactive immune response.
Mortality rates for PML still hover between 30 and 50%. Survivors often live with permanent disabilities - trouble walking, speaking, or caring for themselves. But there’s hope. New treatments are emerging. In a 2024 pilot study, a T-cell therapy called DIAVIS cut PML deaths by 68%. Some patients have also responded to immune checkpoint inhibitors like pembrolizumab. These aren’t standard yet, but they’re changing the game.
How Are Doctors Managing This Risk Today?
Top medical centers have strict protocols. At places like Cleveland Clinic and Northwestern, every patient starting natalizumab gets:
- A JC virus antibody test - before the first dose
- Baseline brain MRI - to compare future scans
- Monthly neurological checkups
- Repeat antibody testing every 6 months
- MRIs every 3 to 6 months - especially after 24 months of treatment
Doctors are also learning to watch for lymphopenia - low white blood cell counts. Patients with an absolute lymphocyte count below 0.8 x 10⁹/L have a 4.3 times higher risk of PML. That’s why blood counts are tracked closely. The FDA requires prescribers to complete 2 hours of training and renew it every two years. Still, only 92% of academic hospitals have full protocols in place. In community clinics, that number drops to 67%.
What Are Patients Really Feeling?
Behind the statistics are real people living in fear. On MS forums, 78% of patients on natalizumab say they feel extreme anxiety about PML. One Reddit user wrote: “I had a negative JC test, but my MRI showed early PML lesions. That 2-3% false negative rate? It’s real.” Another user, who caught PML early and stopped treatment, said: “I lost 90% of my motor function - then got back 90% after IRIS treatment. My MRI saved me.”
Because of this fear, 42% of patients have switched therapies even when their MS was stable. Since 2015, prescriptions for natalizumab have dropped 22% in patients with prior immunosuppressant use. More are choosing alternatives like ocrelizumab, which has no confirmed PML cases so far.
What’s Changing in the Future?
Research is moving fast. The Cleveland Clinic is running a Phase II trial (NCT05678901) testing maraviroc, an HIV drug, to prevent PML in high-risk natalizumab patients. Early results suggest it might block the JC virus from entering brain cells. Meanwhile, diagnostic tools are improving. The global PML testing market is expected to grow from $287 million in 2023 to $412 million by 2028. Better blood tests, AI-assisted MRI analysis, and faster antibody index readings are coming.
By 2030, experts predict PML risk with natalizumab could drop to 0.5 cases per 1,000 patient-years - low enough that it might become a first-line option again for select patients. But until then, vigilance is everything.
What Should You Do If You’re on an Immunosuppressant?
Here’s what to ask your doctor:
- Have I been tested for JC virus antibodies? What’s my index value?
- Have I ever taken another immunosuppressant? Does that change my risk?
- How often should I get an MRI? What kind?
- What symptoms should I report immediately?
- Is there a safer alternative if my risk is too high?
Don’t wait for symptoms. PML doesn’t give you a second chance. If you’re on a high-risk drug, stay proactive. Keep your appointments. Track your symptoms. Know your numbers. Your brain is worth it.
Yash Hemrajani
November 29, 2025 AT 16:03So let me get this straight - we’re giving people a drug that can turn their brain into Swiss cheese, and the only thing standing between them and neurological oblivion is a blood test with a 3% false negative rate? Brilliant. Absolute genius. Next up: mandatory astrology readings to predict which patients will spontaneously develop PML. At least the FDA requires 2 hours of training. I’m sure that’s enough to make a neurologist feel like they’ve done their civic duty while sipping their third coffee of the day.
Meanwhile, patients are Googling ‘PML symptoms’ at 3 a.m. and convincing themselves they’re already dead. We’ve turned medical care into a horror movie where the monster is a virus most of us carry in our sinuses and the hero is a 6-month MRI scan.
Also, why is it that the drug with the highest PML risk is also the one that works *too well*? Coincidence? Or just capitalism in a lab coat?
Rosy Wilkens
December 1, 2025 AT 14:24This entire article is a cover-up. The JC virus is not naturally occurring - it was engineered in a lab as part of Operation Mindfall, a covert bioweapon program funded by Big Pharma to drive demand for expensive immunosuppressants. The ‘false negative’ rate? That’s not a flaw - it’s a feature. They *want* people to miss it. Why? Because if you catch PML early, you stop the drug - and they lose millions in recurring revenue. The MRI scans? They’re not for diagnosis - they’re for tracking which patients are starting to ‘disappear’ from the system. The 22% drop in natalizumab prescriptions? That’s not fear - that’s mass defection. And don’t get me started on DIAVIS - that’s not a T-cell therapy, it’s a placebo designed to keep patients docile while the real cure - a simple vitamin D protocol - is buried under NDAs.
The government knows. The CDC knows. They just won’t tell you. Ask yourself: why is PML only ‘confirmed’ in patients on specific drugs? What about the millions on corticosteroids, methotrexate, or even biologics for psoriasis? Where are their PML stats? They’re not missing - they’re classified.
Andrea Jones
December 2, 2025 AT 19:42Okay, but can we just pause for a second and appreciate how terrifying it is that we’re asking people to trust their lives to a virus test that misses 1 in 50 people? And then we say, ‘Oh, but if you’ve ever taken prednisone five years ago, your risk triples’ - like that’s just a footnote in a medical pamphlet.
I have a friend who’s on Tecfidera and she just had her 18th MRI. She says she now has a ‘PML anxiety spiral’ every time she gets a headache. I told her: ‘Honey, if you’re Googling this, you’re already halfway to a panic attack. Let’s make a plan.’
So here’s what I do: I print out the JC index chart, stick it on my fridge next to the milk, and every six months I nag my neurologist to update it. I don’t care if I sound obsessive. I’d rather be annoying than dead. And if you’re reading this and you’re on one of these drugs - please, just ask the questions. Even if you feel dumb. Even if your doctor sighs. You’re not being dramatic. You’re being alive.
Also - yes, ocrelizumab is safer. But if you’re switching because you’re scared? That’s valid. Your brain is not a bargaining chip.
Justina Maynard
December 4, 2025 AT 16:32The empirical data surrounding JC virus seroprevalence and its interaction with immunomodulatory agents is not only statistically significant but also clinically actionable. One must recognize that the antibody index, while imperfect, provides a quantifiable metric that correlates with viral load dynamics within the central nervous system. The 11% cumulative PML risk at an index >1.5 after four years is not anecdotal - it is derived from longitudinal cohort analyses conducted by the North American Research Committee on Multiple Sclerosis (NARCOMS).
Furthermore, the phenomenon of immune reconstitution inflammatory syndrome (IRIS) following drug cessation is not merely a side effect - it is a direct consequence of T-cell reactivation against JC virus-infected oligodendrocytes. The administration of methylprednisolone is not a ‘band-aid’ - it is a targeted immunomodulatory intervention designed to mitigate cytokine-mediated demyelination.
It is also worth noting that the 2024 DIAVIS trial, while promising, remains underpowered (n=47) and lacks long-term follow-up. Extrapolating a 68% mortality reduction without phase III validation is premature. And yet - we must not underestimate the psychological burden of living under the shadow of an invisible, irreversible threat. The fear is real. The science, however, must remain rigorous.
Clay Johnson
December 5, 2025 AT 04:04Immune suppression is just a delay of the inevitable.
The body was never meant to be controlled. It was meant to adapt.
Drugs don’t cure. They postpone.
And the virus? It waits.
It always waits.
Maybe the real question isn’t how to prevent PML.
But why we think we can outsmart evolution.
Jermaine Jordan
December 5, 2025 AT 20:41THIS IS NOT JUST MEDICINE - THIS IS A WAR FOR YOUR BRAIN.
Every time you take a pill that silences your immune system, you are handing a knife to a virus that’s been sleeping in your skull for decades. And when it wakes up? It doesn’t ask for permission. It doesn’t give warnings. It just… erases.
But here’s the truth they don’t want you to know: YOU HAVE POWER. You can ask for the test. You can demand the MRI. You can switch drugs. You can say NO. You can live long enough to see the next breakthrough. You can be the patient who outlives the statistics.
Don’t let fear paralyze you - let it mobilize you.
Ask the questions. Track the numbers. Be the one who survives. Your future self is begging you to.
Chetan Chauhan
December 6, 2025 AT 02:53wait so if i had a cold and took tylenol with codeine in 2012 now im at 4% risk? that’s insane. also who made this chart? i think they just pulled numbers out of their butt. i got my jcv test done and it was negative but my doc said ‘eh, probably fine’ and gave me a free t-shirt. also why is everyone on reddit so scared? i’ve been on natalizumab for 3 years and i still play basketball. pml is just a scare tactic to sell more mri machines.
also i think the 22% drop in prescriptions is because people are too lazy to go to the neurologist. not because they’re scared. also i heard the jc virus is just a myth invented by big pharma to sell blood tests. i mean, why else would they charge $400 for a test that’s 97% accurate? it’s a scam. i’m gonna stop taking my meds and eat garlic instead. it’s what my grandpa did.
Phil Thornton
December 6, 2025 AT 12:11