Many people say they’re allergic to penicillin-or aspirin, or sulfa drugs-only to find out later they never had an allergy at all. They just had a side effect. And that mix-up isn’t harmless. It can lead to worse antibiotics, longer hospital stays, and even life-threatening infections. The truth is, drug allergy is rare. Only 5 to 10% of reported drug reactions are true allergies. The rest? Side effects, intolerances, or bad luck. Knowing the difference isn’t just helpful-it can save your life.
What Is a True Drug Allergy?
A true drug allergy means your immune system mistakes the medication for a threat. It’s not just your stomach being upset. It’s your body launching an attack. This happens through specific immune pathways-usually involving IgE antibodies for immediate reactions, or T-cells for delayed ones. When that happens, you get symptoms like hives, swelling, trouble breathing, or even anaphylaxis. These aren’t just unpleasant. They’re dangerous.Immediate allergic reactions show up fast-within minutes to an hour after taking the drug. Think: hives breaking out 20 minutes after swallowing amoxicillin. Or your throat closing up after a penicillin shot. Delayed reactions can take days or weeks. A rash that appears two weeks after starting a new antibiotic? That could be a T-cell response. Severe cases like DRESS or Stevens-Johnson Syndrome are immune-driven too. They’re rare, but they demand immediate medical attention.
What Is a Side Effect?
Side effects are predictable. They’re built into how the drug works. If a medication affects your stomach lining, you might get nausea. If it lowers your blood pressure, you might feel dizzy. These aren’t your immune system going haywire. They’re just the drug doing what it’s supposed to do-just in the wrong place.Side effects usually depend on dose. Take more, and the effect gets stronger. Take less, and it fades. Often, they get better over time as your body adjusts. Nausea from antibiotics? It might last a few days, then disappear. Headache from a blood pressure pill? Might go away after a week. That’s not an allergy. That’s pharmacology.
Common side effects include nausea (22% of users), headache (18%), dizziness (15%), and upset stomach (35%). These are so common, they’re listed in every drug’s patient leaflet. But here’s the problem: people hear “adverse reaction” and assume it’s an allergy. That’s where things go wrong.
How to Tell the Difference
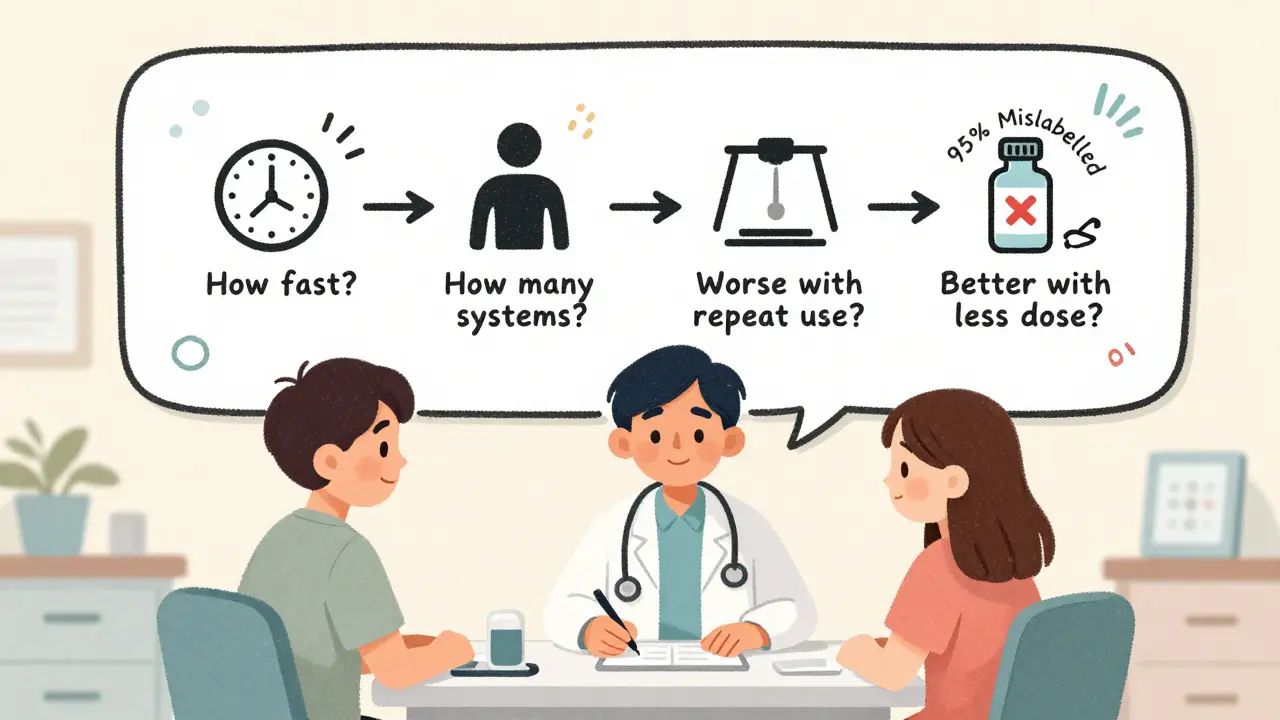
There’s a simple checklist most doctors use. Ask yourself these four questions:- How fast did it happen? If symptoms showed up within an hour-especially hives, swelling, or breathing trouble-it’s likely an allergy. If it took days or weeks, it could still be immune-related, but it’s not IgE-mediated.
- How many systems are involved? Allergies often hit more than one. Skin rash + vomiting + wheezing? That’s a red flag. Side effects usually stick to one system-like just nausea, or just dizziness.
- Did it get worse with repeat use? Allergic reactions tend to get stronger each time you take the drug. Side effects often improve or stay the same.
- Can you take less to make it better? If lowering the dose helps, it’s probably a side effect. If even a tiny amount triggers a reaction, it’s likely an allergy.
For example: If you took ibuprofen and got a rash and swollen lips within 30 minutes, that’s an allergy. If you took it and felt a little nauseous, that’s a side effect. If you took it every day for a month and the nausea never went away, it’s still a side effect-not an allergy.
Why It Matters: The Penicillin Myth
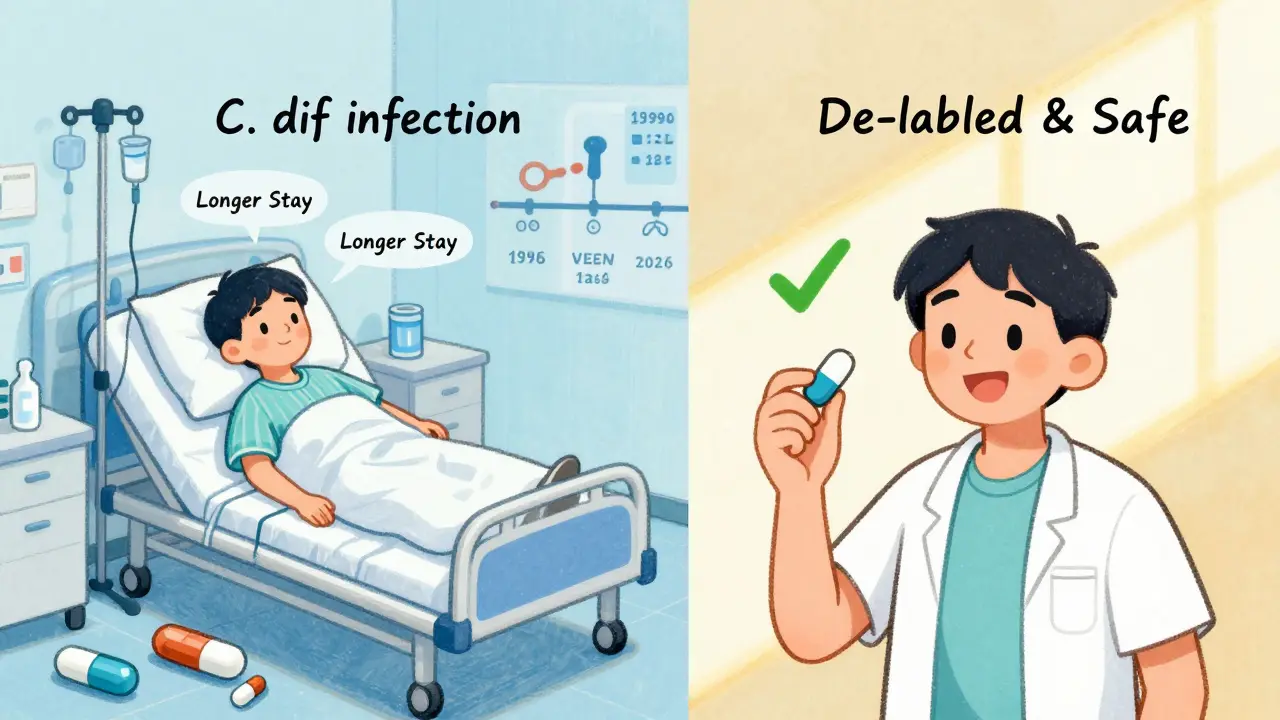
About 7% of Americans say they’re allergic to penicillin. That sounds serious. But here’s the shocking part: 90 to 95% of them aren’t. When tested properly-through skin tests or supervised challenges-most can take penicillin without a problem.Why does this happen? Because decades ago, someone got a rash after taking penicillin. They called it an allergy. Maybe it was a viral rash. Maybe it was a side effect. Either way, the label stuck. Now they avoid penicillin and get broader-spectrum antibiotics instead. Those drugs are more expensive, more toxic, and more likely to cause C. diff infections. A 2022 JAMA study found people with mislabeled penicillin allergies had a 69% higher chance of getting C. diff-and stayed in the hospital 30% longer.
That’s not just personal risk. It’s a public health problem. The CDC estimates incorrect penicillin allergy labels cost the U.S. healthcare system over $1 billion a year. And it’s all because people don’t know how to tell the difference.
What About Delayed Reactions?
Not all allergies happen right away. Some show up days or weeks later. A rash that appears 10 days after starting an antibiotic? That’s often a T-cell reaction. It’s still an allergy-even if it’s not hives or swelling.These delayed reactions can be serious. DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) causes fever, rash, swollen lymph nodes, and organ inflammation. It’s rare, but it can damage your liver or kidneys. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are even rarer-about 1 to 6 cases per million prescriptions-but they’re life-threatening. If you get a blistering rash, mouth sores, or peeling skin after starting a new drug, get help immediately. These are immune-driven, not side effects.
Diagnosing these isn’t simple. Skin tests won’t help. Doctors use patch tests or blood tests like lymphocyte transformation tests. That’s why seeing an allergist matters-if you’ve had a delayed reaction, you need expert evaluation.
What Should You Do?
If you think you have a drug allergy, don’t just assume. Don’t avoid the drug forever. Talk to your doctor. Ask: “Could this have been a side effect?”Here’s what to do next:
- Write down exactly what happened: What drug? When? What symptoms? How long did they last?
- Did you have more than one symptom at once? Skin + breathing + stomach? That’s a red flag.
- Did it happen once, or every time you took it?
- Did you need emergency care? If yes, that’s a strong sign it was an allergy.
If you’re unsure, ask for a referral to an allergist. Many hospitals now have drug allergy clinics. They can do skin tests for penicillin or other common drugs. The Penicillin ImmunoCAP test, approved by the FDA in 2023, can detect IgE antibodies with 97% accuracy.
And if you’ve been told you’re allergic but never had a real allergic reaction? Ask about de-labeling. It’s safe, fast, and changes your future care. Over 87% of people who get tested and de-labeled never have another reaction.
What’s Changing in 2026?
The medical world is catching up. In 2024, the American College of Allergy, Asthma, and Immunology will officially start using three terms:- Allergy = immune system reaction
- Intolerance = unpleasant but non-immune reaction
- Side effect = expected pharmacological effect
That’s huge. It means doctors will stop calling nausea an allergy. Electronic health records now require clear labels-true allergy vs. side effect-by January 2025. Pharmacies and hospitals are rolling out decision tools to flag risky mislabels.
And it’s working. Hospitals with formal allergy assessment programs have cut inappropriate antibiotic use by 27%. That’s fewer infections, shorter stays, lower costs.
Final Thought: Don’t Guess. Get Checked.
You don’t need to be a doctor to know the difference. But you do need to ask the right questions. If you’ve ever said, “I’m allergic to this drug,” but never had hives, swelling, or trouble breathing-you might be wrong. And that’s okay. You’re not alone. But now you know what to do next.Write down your history. Talk to your doctor. Get tested if needed. One simple step could open up better, safer, cheaper treatment options for the rest of your life.
Can you outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a penicillin allergy in childhood lose it over time-even if they never got tested. The immune system can forget the drug is a threat. That’s why it’s never too late to get evaluated, even if the reaction happened decades ago.
Is a rash always a sign of a drug allergy?
No. Many rashes are caused by viruses, especially in kids. If you develop a rash while taking antibiotics for a sore throat or ear infection, it could be the infection, not the drug. Doctors look at timing: if the rash appears after 5-10 days on the drug, it’s more likely an allergic reaction. If it shows up right away with fever or other symptoms, it’s more likely viral. Never assume a rash is an allergy without evaluation.
Can you have a drug allergy without knowing it?
Absolutely. Some people have mild reactions they never connected to the drug-like a headache after taking ibuprofen or a stomach ache after antibiotics. They don’t report it. But if you take the same drug again, the reaction could be worse. That’s why documenting every unusual symptom matters. Even if it seems minor, write it down.
Are over-the-counter drugs like ibuprofen or acetaminophen common causes of allergies?
Rarely. Most reactions to NSAIDs like ibuprofen are side effects-stomach upset, dizziness, or headache. True IgE-mediated allergies to these drugs are extremely uncommon. However, some people have non-allergic hypersensitivity-like asthma flare-ups after taking aspirin. That’s not an allergy, but it still requires avoidance. If you react to OTC pain relievers, see an allergist to find out why.
What should I do if I think I had a drug allergy?
Stop the drug immediately. If you have trouble breathing, swelling of the face or throat, or feel faint, call 911. For less severe symptoms, contact your doctor. Don’t just note it as “allergy” in your records-describe exactly what happened. Ask if you should see an allergist. Bring your medication list and symptom timeline. This could prevent future harm.

Rob Deneke
January 15, 2026 AT 12:52Man I used to think I was allergic to penicillin cause I got a rash once after taking it for a sore throat
Turns out it was just a virus
Got tested last year and now I can take it without worry
Best decision ever
Riya Katyal
January 16, 2026 AT 22:39Oh wow so now we’re supposed to believe every person who says ‘I’m allergic’ is just bad at remembering their own body?
Next you’ll tell me people who say they’re lactose intolerant are just bad at counting milk cartons
evelyn wellding
January 18, 2026 AT 17:55THIS IS SO IMPORTANT!!! 🙌
I used to avoid all antibiotics because I thought I was allergic to everything 😅
Got tested last year and now I can actually get treated properly
My doctor was like ‘you’ve been lucky to survive this long’ lol
Y’all need to get checked!! Your future self will thank you 💖
Chelsea Harton
January 19, 2026 AT 19:47Immune system is dumb
It forgets things
Or remembers wrong
Like that one ex who still texts you
But drugs? No
Just test it
Corey Chrisinger
January 20, 2026 AT 13:14It’s wild how we treat medicine like it’s magic
We don’t question why a pill makes us dizzy but we panic if it gives us a rash
Maybe we need to stop thinking of side effects as failures
And start seeing them as feedback
Our bodies are just trying to tell us something
Not betray us
Bianca Leonhardt
January 21, 2026 AT 03:59People who say they’re allergic to everything are the same ones who think ‘gluten’ is the root of all evil
Stop self-diagnosing and go see a real doctor
You’re not special
You’re just lazy
Travis Craw
January 22, 2026 AT 20:55My mom was told she was allergic to penicillin in the 70s
Turns out she just got a rash from the virus she had
She avoided it for 40 years
Got tested last year
Turns out she’s fine
Now she’s like ‘why didn’t anyone tell me this sooner?’
So yeah… if you’re unsure, just ask
Christina Bilotti
January 23, 2026 AT 23:46Oh wow so the medical system is just… wrong? Shocking.
Let me guess, next you’ll tell me ‘I’m allergic to peanuts’ is just a bad case of indigestion?
How quaint.
Maybe if people bothered to learn actual medicine instead of googling symptoms at 2am this wouldn’t be a problem
But no, let’s just keep blaming doctors while you self-diagnose from TikTok
brooke wright
January 23, 2026 AT 23:47Wait so if I got a headache after ibuprofen but it went away after a week… that’s not an allergy?
But if I got hives in 10 minutes? That is?
So it’s all about timing?
And how many body parts are involved?
Wait so what if I got a rash AND nausea but it took 3 days?
Is that still an allergy?
What if I only took it once?
What if I’m 72 and it happened when I was 22?
So… what do I do now?
vivek kumar
January 25, 2026 AT 05:10Most people don’t realize that mislabeling a drug reaction as an allergy is like calling a broken leg a sprain and then refusing to walk for 20 years.
It’s not bravery. It’s ignorance with consequences.
And yes, the economic cost is staggering - but the human cost is worse.
People die because they’re given worse drugs.
Not because the right one failed.
Because it was never tried.
Nick Cole
January 26, 2026 AT 05:41I had a friend who had a rash after amoxicillin as a kid
She avoided all penicillins for 15 years
Then she got a life-threatening infection and the only effective drug was penicillin-based
She was terrified
But she got tested
Turns out she was never allergic
She got treated
She’s fine now
So if you’ve been avoiding a drug because of something that happened decades ago…
Just ask your doctor
It’s not scary
It’s just smart