Most people think of Imodium as a quick fix for a bad stomach. You grab a bottle from the pharmacy shelf, pop a couple of pills, and within hours, the cramps and urgency fade. It’s safe, right? Over-the-counter means harmless. But what if I told you that the same pill you use for a one-day stomach bug can, when misused, stop your heart? This isn’t a scare tactic. It’s happening right now - in homes, in emergency rooms, and in recovery centers across North America.
How a Common Diarrhea Remedy Became a Hidden Opioid Substitute
Loperamide is the active ingredient in Imodium A-D, Diamode, and other OTC brands. It was designed in the 1970s to treat diarrhea without the addictive risks of older opioid-based drugs. At normal doses - 4 mg at first, then 2 mg after each loose stool, max 8 mg per day - it works exactly as intended: it slows down your gut. It barely touches your brain because of a natural body guard called P-glycoprotein. This protein pushes loperamide out of the bloodstream before it can cross into the central nervous system. But here’s the twist: when someone takes 50, 100, or even 400 mg in a single day - yes, that’s real - that guard gets overwhelmed. The loperamide slips through. Suddenly, it starts acting like morphine in the brain. Not as strongly, but enough. People with opioid use disorder began using it to stave off withdrawal symptoms: sweating, shaking, nausea, bone-deep aches. And because it’s sold on store shelves without a prescription, it’s easy to get. No doctor’s visit. No scrutiny. Just a quick trip to the pharmacy or a click online.The Silent Killer: How Loperamide Attacks Your Heart
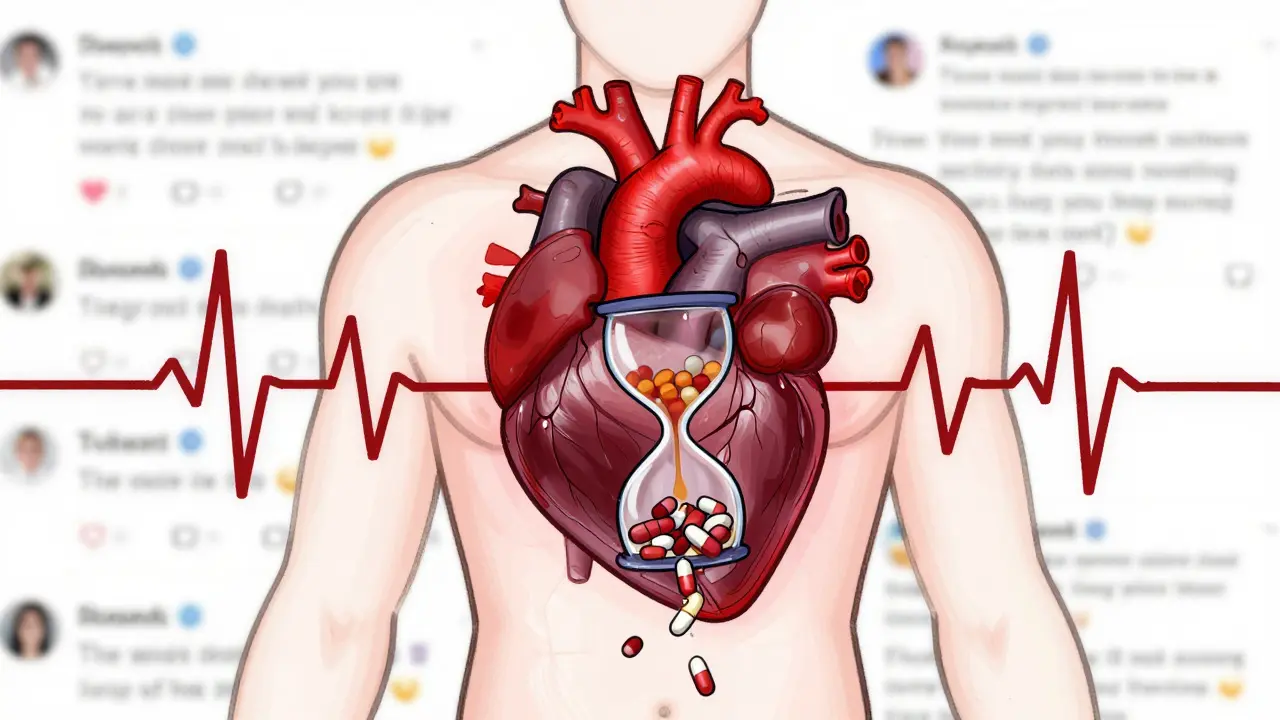
The real danger isn’t just that it mimics opioids. It’s what it does to your heart. At toxic doses, loperamide blocks potassium channels in heart muscle cells - specifically the hERG channel. This disrupts the electrical rhythm that keeps your heart beating regularly. The result? QT interval prolongation. That’s when the heart takes too long to recharge between beats. And when that happens, it can spiral into a deadly arrhythmia called torsades de pointes. It looks like a twisting pattern on an ECG. It can turn into ventricular fibrillation. And then - no pulse. No warning. The FDA reviewed 48 serious cardiac events linked to loperamide abuse. More than half happened after 2010. In one documented case, a 32-year-old man took 80 mg a day - 10 times the maximum recommended dose - to manage opioid withdrawal. He ended up in the ER with polymorphic ventricular tachycardia, a prolonged QTc of 560 ms, and temporary heart failure. He survived. Many don’t. Between 2011 and 2020, at least 17 deaths were directly tied to loperamide toxicity, according to FDA data. In 2020 alone, nearly half of all loperamide exposures reported to poison control centers were intentional overdoses. And 28% of those cases led to moderate to severe outcomes - including seizures, cardiac arrest, and coma.Warning Signs You Can’t Ignore
If someone you know is taking more than 8 mg of loperamide a day - or buying multiple bottles at once - pay attention. Here’s what to look for:- Heart symptoms: Unexplained chest pain, palpitations, dizziness, fainting, or sudden collapse. These are red flags, especially if there’s no history of heart disease.
- Gut issues: Severe constipation, bloating, or even a paralyzed intestine (ileus). This isn’t just "feeling backed up." It’s a medical emergency.
- Behavioral changes: Someone with opioid dependence suddenly starts hoarding Imodium. They’re secretive about it. They buy it in bulk online. They’re avoiding doctors.
- Drug mixing: Some users take loperamide with other substances like diphenhydramine (Benadryl), cimetidine (Tagamet), or quinidine to boost absorption. That’s a recipe for disaster. These drugs block the very system that normally protects you.
These signs don’t always show up together. Sometimes, the only symptom is a sudden cardiac arrest. That’s why doctors are now trained to ask: "Have you been taking any OTC diarrhea medicine?" - especially if the patient has a history of substance use.
Why People Risk It - And Why It’s a Trap
It’s not about getting high. Most users don’t feel euphoria. In fact, many describe the experience as unpleasant: nausea, dizziness, confusion. But for someone in the grip of opioid withdrawal, even a faint sense of relief is worth the risk. Reddit threads from recovery communities are full of heartbreaking stories. One user wrote: "Tried 50 mg of Imodium to get through withdrawal. Woke up in the ER with my heart racing. Never again." Another said: "I thought if I took enough, it would replace my prescription. I didn’t know I was killing myself slowly." The trap? The more you take, the more your body needs to feel the same effect. And the more you take, the higher the chance of heart damage. It’s a vicious cycle. You don’t get high. You don’t get relief for long. But you do get closer to cardiac arrest.What’s Being Done - And What You Can Do
In 2016, the FDA issued a safety alert. In 2019, major manufacturers started putting loperamide in single-dose blister packs for bottles over 45 mg. That makes it harder to swallow 20 pills at once. Sales dropped 12% between 2016 and 2020. But abuse hasn’t stopped. People still buy it in bulk online. Some import it from overseas. Others crush pills and dissolve them to bypass the slow-release form. The solution isn’t taking loperamide off the shelf. It’s still vital for millions who genuinely need it for diarrhea. The answer is awareness.- If you’re using loperamide for more than 48 hours, talk to a doctor. Chronic diarrhea needs diagnosis - not just a pill.
- If you or someone you know is using it to manage opioid withdrawal, get help. Medications like buprenorphine or methadone are safer, supervised, and effective. Call SAMHSA’s helpline at 1-800-662-HELP.
- Keep loperamide locked up if someone in your home has a history of substance use.
- Know the signs. If someone collapses or complains of chest pain after taking loperamide, call 911. Tell them it’s suspected loperamide overdose. That changes how they treat it.

What Happens in the ER
When someone arrives with suspected loperamide toxicity, doctors don’t just check for drugs. They check the heart. Standard drug screens don’t detect loperamide. So if the ECG shows a prolonged QT interval - and the patient has no heart history - loperamide abuse becomes the prime suspect. Treatment includes:- Stopping all loperamide immediately
- Continuous heart monitoring for at least 24 hours
- IV magnesium sulfate to stabilize the heart rhythm
- Potentially, activated charcoal if taken recently
- In severe cases, temporary pacing or even ECMO (a heart-lung machine)
Naloxone (Narcan) won’t reverse the cardiac effects - and it doesn’t always work on loperamide’s opioid action, either. That’s why just giving Narcan and sending someone home is dangerous. This isn’t a typical opioid overdose. It’s a cardiac emergency with opioid roots.
It’s Not Just a "Drug Problem" - It’s a Public Health Blind Spot
Loperamide abuse flies under the radar because it’s not illegal. It’s not a controlled substance. It’s not even listed as a drug of abuse in most addiction programs. But it kills. A 2018 study found that 15.3% of people with opioid use disorder had used loperamide to self-treat withdrawal. That’s one in six. And yet, most doctors don’t screen for it. Most pharmacists don’t ask questions. Most families don’t know what to look for. This isn’t about judgment. It’s about survival. People are using loperamide because they’re desperate. They don’t have access to treatment. Or they’re afraid of stigma. Or they’ve been told, "Just take Imodium - it’s safe." We need to change that message.Can you overdose on Imodium if you take too much for diarrhea?
Yes. The maximum safe daily dose for OTC use is 8 mg. Taking more than that - even if you think you need it for severe diarrhea - increases your risk of serious side effects like constipation, bowel paralysis, and dangerous heart rhythm changes. If diarrhea lasts longer than 48 hours, see a doctor. Don’t keep increasing the dose.
Is loperamide addictive like heroin or oxycodone?
Loperamide isn’t addictive in the same way. It doesn’t cause the same intense euphoria. But when taken in massive doses, it can create physical dependence. People who use it daily to manage opioid withdrawal often find they need more and more to feel relief - a classic sign of tolerance. Stopping suddenly can trigger withdrawal symptoms like anxiety, sweating, and muscle pain.
Can you die from taking too much loperamide?
Yes. Between 2011 and 2020, at least 17 deaths were confirmed in the U.S. due to loperamide toxicity. The cause is usually a fatal heart rhythm called torsades de pointes, triggered by the drug’s effect on heart cells. Many of these deaths happened in people who took 100 mg or more in a single day.
Why don’t pharmacies limit how much loperamide you can buy?
The FDA hasn’t restricted sales because loperamide is still very effective and safe when used correctly for diarrhea. Instead, manufacturers now package larger bottles in single-dose blister packs to discourage bulk abuse. Some pharmacies also ask questions if someone buys multiple bottles. But there’s no legal limit - which is why education and awareness are so important.
What should I do if I think someone is abusing loperamide?
Don’t confront them with anger. Approach with concern. Say something like, "I noticed you’ve been taking a lot of Imodium. Are you okay?" Then connect them with resources: SAMHSA’s helpline (1-800-662-HELP), a doctor, or a substance use counselor. If they’re showing signs of heart trouble - chest pain, fainting, irregular heartbeat - call 911 immediately. Tell the ER staff it’s suspected loperamide overdose.

Moses Odumbe
December 19, 2025 AT 00:01Bro. I saw a guy at the gas station buy 3 boxes of Imodium last week. Asked him if he was okay. He just laughed and said, "Just fixing my gut." 🤡 I knew then. This isn't just diarrhea anymore. We're in the era of DIY opioid replacement. And no one's talking about it. 😔
Meenakshi Jaiswal
December 20, 2025 AT 23:04As a pharmacist in Mumbai, I've seen this happen more than once. People come in asking for "the strongest Imodium" because they're "trying to quit pills." I always hand them a pamphlet on SAMHSA and quietly call the clinic next door. It's not about policing - it's about seeing the pain behind the purchase. 🙏
bhushan telavane
December 22, 2025 AT 19:41India has the same problem. People buy loperamide from street vendors because they think it's "legal weed." No one tells them it can stop their heart. We need more awareness in villages. Not just in cities. This is a silent epidemic. 🇮🇳
Mahammad Muradov
December 24, 2025 AT 19:10People who abuse this are just lazy addicts who don't want to go through real detox. If you can't handle withdrawal, maybe you shouldn't have started using opioids in the first place. This isn't a public health crisis - it's a personal failure. Stop enabling them with sympathy. Just say no.
Connie Zehner
December 25, 2025 AT 09:41OMG I knew someone like this!! My cousin took 200mg in one day and ended up in the ICU!! I was SO worried!! She said she just wanted to "feel normal" but then she started crying and said she didn't even feel high?? Like what even is this?? I'm still traumatized. 😭💔 I told her to call the helpline and she blocked me. I hate this so much.
holly Sinclair
December 26, 2025 AT 17:06It’s fascinating, really, how a molecule designed to act locally on the gut can, under the right (or wrong) pharmacokinetic conditions, become a systemic opioid agonist. The P-glycoprotein efflux pump is a brilliant evolutionary safeguard - but it’s not infallible. What’s more tragic is that we’ve built a healthcare system where the most vulnerable turn to over-the-counter drugs not because they’re reckless, but because the system failed them. We’ve turned medicine into a commodity and compassion into a liability. And now people are dying because the only thing accessible is the thing that kills them. The real question isn’t whether loperamide should be regulated - it’s why we let people reach for it in the first place.
Monte Pareek
December 27, 2025 AT 01:37Look I've been in recovery for 7 years and I've seen this exact thing play out a dozen times. Loperamide isn't the problem. The problem is the lack of access to MAT. The problem is insurance denying buprenorphine. The problem is stigma. You don't need to ban Imodium. You need to fund clinics. You need to train ER staff to ask "Have you been taking diarrhea meds?" instead of assuming it's cocaine or heroin. You need to stop treating addiction like a moral failure. This isn't a drug problem. It's a justice problem. And if you're not fighting for that, you're part of the problem.
Kelly Mulder
December 27, 2025 AT 03:12It is, regrettably, a phenomenon of alarming proportions. The casual, almost flippant, accessibility of loperamide - a substance with documented, life-threatening cardiotoxic potential - represents a catastrophic failure of pharmaceutical oversight. One cannot help but question the ethics of permitting a compound capable of inducing torsades de pointes to be sold alongside toothpaste. The FDA’s blister-pack initiative is a cosmetic measure. What is required is a reclassification. Immediately.
Tim Goodfellow
December 27, 2025 AT 17:03Man, I thought I was the only one who noticed this. Last month I saw a bloke in a pub in Glasgow buying a 96-pill pack of Imodium like it was a bag of crisps. He looked like hell. Pale. Sweating. Didn't say a word. I asked if he was okay. He just shrugged and said, "Just a bit of tummy trouble." Mate. You were sweating like you'd run a marathon in a sauna. I slipped him a card for a local recovery group. He didn't take it. But I hope he kept it. We gotta look out for each other. This ain't just pills. It's people screaming without sound.
Elaine Douglass
December 28, 2025 AT 11:20My brother did this and I didn't even know until he collapsed at work. He's okay now but he's in rehab. I just want people to know it's not just "taking too much medicine" - it's a cry for help. Please check on the quiet ones. They're the ones doing this. ❤️