When you buy a pill, a medical device, or even a children’s toy, you assume it’s safe. But behind many of these products is a complex, often hidden chain of overseas manufacturing - and not all of it meets the standards you expect. In 2024, foreign manufacturing accounted for 62% of all drug recalls in the U.S., even though these facilities only produced 43% of the total volume. That’s not a coincidence. It’s a symptom of a deeper problem: quality control is breaking down in places where oversight is weak, incentives are misaligned, and pressure to cut costs is crushing integrity.
Why Quality Fails Overseas
It’s not that factories overseas are inherently bad. Many are modern, well-equipped, and staffed by skilled workers. The problem isn’t location - it’s systems. When a U.S. company outsources production to China, India, or Vietnam, they often rely on third-party agents, distant audits, and paperwork instead of real-time oversight. That’s a recipe for disaster. Take material substitution. According to Brookings Institution’s 2025 analysis, 68% of inspected Chinese manufacturing sites were found to swap out approved raw materials for cheaper alternatives. One case from Wuhu Nuowei Chemistry Co., Ltd. - cited in an FDA warning letter in February 2025 - involved a batch of generic medication contaminated with impurities because the company didn’t even set proper limits for them. The FDA’s own data shows that 47% of Chinese drug facilities received Form 483 observations in 2024 - far higher than the 29% for U.S. sites. And here’s the kicker: 78% of those inspections in China were announced in advance. That means factories had days, sometimes weeks, to clean up, fake records, or hide violations. In the U.S., only 5% of inspections are announced. The playing field isn’t just uneven - it’s rigged.The Hidden Cost of Cheap Production
You might think saving 30-45% on labor costs is a win. But when a batch of pills fails biocompatibility testing - like the 12,000 units from a Shenzhen supplier that used industrial-grade silicone instead of medical-grade - you don’t just lose the batch. You lose trust. You lose customers. You face lawsuits. And if the product is something life-critical, like insulin or antibiotics, you risk lives. Harris Sliwoski’s 2025 report found that unaddressed quality issues add 15-25% to total manufacturing costs when you factor in recalls, rework, legal fees, and lost sales. That’s more than the savings you thought you got. And it’s not just about money. The FDA says quality failures in foreign drug plants contributed to 37% of U.S. drug shortages in 2024. That’s not just an inconvenience - it’s a public health crisis.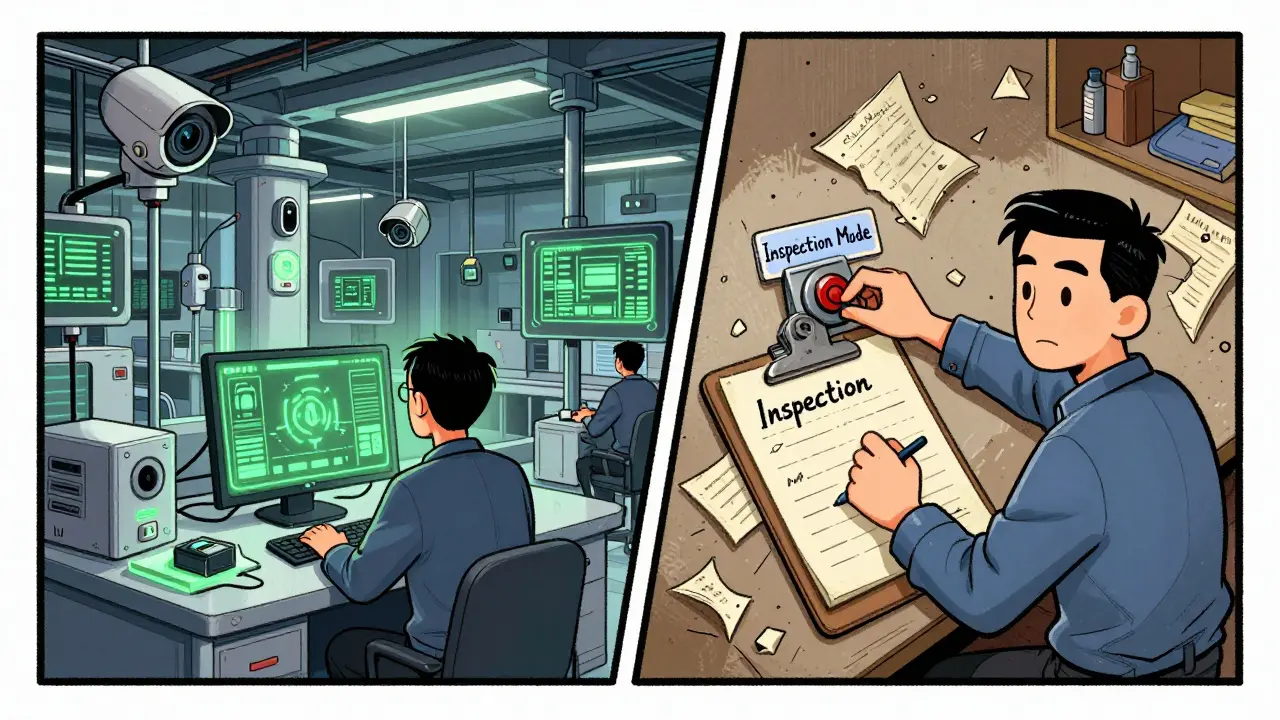
Where the Problems Are Worst
Not all countries are the same. China remains the largest source of foreign manufacturing, but its quality landscape is splitting in two. On one side, companies aligned with China’s “Made in China 2025” initiative are investing in AI-driven quality control, real-time monitoring, and certified staff. GQC.io reports that 73% of top-tier Chinese manufacturers now use advanced analytics. But on the other side, thousands of smaller, financially strained factories are cutting corners to survive. Some are even running “sophisticated bank-switch scams” - where they switch production lines overnight to avoid inspections, then switch back after the auditors leave. India is another major concern. Despite making up only 25% of foreign drug facilities, Indian suppliers accounted for 34% of FDA import alerts in 2024. The issue here isn’t lack of capability - it’s lack of enforcement. Quality assurance teams often report to production managers, not independent compliance officers. That means when a factory is under pressure to meet deadlines, quality gets sacrificed. Vietnam, meanwhile, is showing improvement. Gembah’s 2025 report found an 18% rise in quality metrics since 2022. That’s because many Vietnamese factories are being built from scratch with Western partners who demand transparency from day one. It’s not perfect - but it’s a model others could follow.How to Fix It
There’s no magic bullet. But companies that survive - and thrive - in overseas manufacturing do three things differently. First, they don’t rely on paper audits. They send their own quality managers to live on-site. One Minnesota medical device company reduced defects from 12.7% to just 0.8% by hiring a full-time Chinese quality lead, installing blockchain traceability, and using third-party verification labs. That’s not cheap - it cost them $18,500 per year per facility in training and salaries - but it saved them millions in recalls. Second, they demand unannounced inspections. The FDA is finally moving in this direction. In May 2025, Commissioner Marty Makary announced that by 2027, 75% of foreign inspections will be unannounced - matching U.S. standards. Companies that want to stay compliant need to build that into their contracts. No advance notice. No exceptions. Third, they write ironclad contracts. Vague language like “products must meet international standards” is useless. Contracts must specify exact tolerances, material grades, testing methods, and penalties for non-compliance. Harris Sliwoski found that 58% of recoverable losses came from contracts that didn’t define quality clearly enough.
The Future Is Digital - But Not Everywhere
Technology is helping. AI-powered visual inspection systems now detect defects at 99.2% accuracy - far better than human eyes. IoT sensors track temperature, humidity, and vibration in real time. Blockchain logs every step of production, making fraud nearly impossible to hide. But here’s the truth: only 22% of Chinese manufacturers have fully adopted these tools as of Q2 2025. Most still rely on clipboards and handwritten logs. The companies that win in the next five years won’t be the ones with the lowest labor costs. They’ll be the ones who treat quality as a system - not an afterthought. That means investing in people, not just machines. It means trusting your own eyes more than a supplier’s report. And it means accepting that true safety isn’t cheap - it’s worth every penny.What You Should Do
If you’re a business buying from overseas:- Don’t sign contracts without a site visit - and make it unannounced.
- Require third-party lab testing on every shipment, not just samples.
- Build a China-specific quality triad: local QA manager, real-time data monitoring, and independent verification.
- Train your team on FDA 21 CFR Part 211 standards - not just generic ISO 9001.
- Set aside 8-12 weeks for supplier vetting. Rushing this step is how disasters start.
Why are FDA inspections in China often announced in advance?
Historically, Chinese manufacturers and local regulators have treated inspections as formalities rather than enforcement tools. Announcing inspections in advance allows factories to clean up, falsify records, or temporarily shut down non-compliant lines. Through 2024, 78% of FDA inspections in China were scheduled - compared to just 5% in the U.S. This double standard created blind spots that allowed dangerous products to slip through. Starting in 2025, the FDA is shifting to unannounced inspections, aiming for 75% coverage by 2027 to close this gap.
Can AI really fix quality issues in overseas manufacturing?
AI can detect defects with 99.2% accuracy - far better than human inspectors, who typically catch 85-90%. But AI alone can’t fix the root problem: intentional fraud and weak management systems. AI can spot a wrong label or a missing component, but it can’t tell if a factory is deliberately using substandard materials to save money. The most effective systems combine AI with human oversight, real-time data, and strict contractual accountability. AI is a tool - not a solution.
Is "Made in China 2025" actually improving quality?
It’s mixed. The initiative has pushed high-end manufacturers - especially in electronics, robotics, and medical devices - to adopt advanced quality systems. Dr. Li Wei of Tsinghua University says 73% of top-tier Chinese firms now use AI and analytics. But this only applies to a small fraction of factories. The majority of Chinese manufacturers, especially small and mid-sized ones, are under financial pressure and continue to cut corners. The initiative hasn’t fixed the system - it’s created a two-tiered quality landscape: one for elite exporters, and one for everyone else.
Why do so many recalls come from India?
India produces a large share of generic drugs - about 25% of U.S. imports - but accounts for 34% of FDA import alerts. The issue isn’t skill or infrastructure; it’s governance. Many Indian manufacturers have quality teams that report to production managers, not independent compliance officers. This creates a conflict: when deadlines are tight, quality gets sacrificed. Unlike the EU’s Qualified Person system - where a certified professional must personally sign off on every batch - India lacks equivalent accountability. That’s why the FDA keeps flagging them.
What’s the biggest mistake companies make when outsourcing manufacturing?
The biggest mistake is assuming that a supplier’s word is enough. Too many companies rely on certificates, photos, or third-party audits that are either outdated, biased, or faked. The real solution is direct, ongoing involvement: sending your own QA staff to live on-site, using blockchain or IoT to track production in real time, and testing every shipment independently. If you’re not physically involved, you’re not in control - and you’re gambling with safety.