Antiemetic Risk Calculator
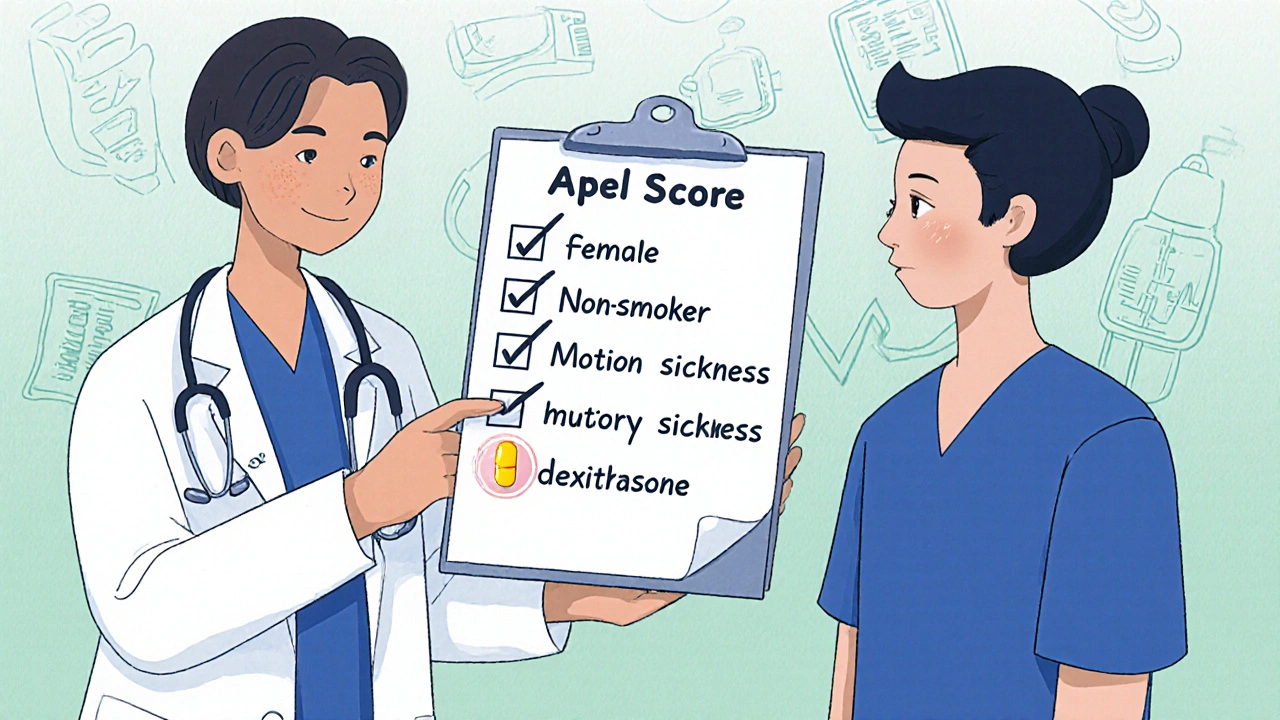
What is the Apfel Score?
The Apfel Score is a simple risk assessment tool that helps doctors determine which antiemetic to use after surgery. It's based on four risk factors:
- Female sex (2.2x higher risk)
- Non-smoker (1.9x higher risk)
- History of motion sickness or past PONV (3.1x higher risk)
- Will get opioids after surgery (1.5x higher risk)
When you're recovering from surgery, starting a new pain medication, or undergoing chemotherapy, nausea isn't just uncomfortable-it can delay healing, increase hospital stays, and even make you avoid necessary treatments. The good news? There are effective ways to stop it. But not all antiemetics are the same. Choosing the wrong one can mean wasted money, unnecessary side effects, or even serious risks. This isn't about guessing. It’s about matching the right drug to your situation.
What Exactly Are Antiemetics?
Antiemetics are drugs made to stop nausea and vomiting. They don’t just mask the feeling-they interrupt the signals in your brain and gut that trigger these reactions. There are seven main types, each with a different way of working. Some block serotonin. Others block dopamine. Some calm the inner ear. And a few even reduce inflammation. The key is knowing which one fits your cause of nausea.
For example, if you’re getting opioids after surgery, your nausea comes from how those drugs affect your brainstem. If you’re on chemo, it’s often serotonin flooding your gut. And if you’re prone to motion sickness, it’s your vestibular system. Each needs a different tool.
Top Antiemetics and How They Work
Let’s break down the most commonly used ones, based on real-world use and clinical data.
- Ondansetron (Zofran) - Blocks serotonin (5-HT3) receptors. It’s the go-to for chemo and surgery nausea. Works fast-often within 15 minutes. Standard dose: 4-8 mg IV or 8 mg oral. It’s effective in 65-75% of PONV cases. But it can cause headaches (reported by 32% of users) and, rarely, abnormal heart rhythms, especially in people with existing heart conditions.
- Droperidol (Inapsine) - Blocks dopamine receptors. Often overlooked because of old fears, but low-dose (0.625-1.25 mg IV) is safe and works better than ondansetron in some cases. One study showed only 14.5% of patients got nauseated with droperidol vs. 26.7% with tropisetron. It’s also cheaper-about $0.50 per dose. Requires ECG monitoring only if dose exceeds 1.25 mg.
- Dexamethasone - A steroid. Doesn’t work fast-it takes 4-5 hours. So it’s not for immediate relief. But when combined with ondansetron or droperidol, it boosts success rates by 20-30%. Used in 8 mg IV doses. Cost: $0.25 per dose. Ideal for high-risk patients.
- Metoclopramide (Reglan) - Blocks dopamine and speeds up stomach emptying. Great for nausea from slow digestion, like after abdominal surgery. But at 10 mg, it’s weak for pure medication-induced nausea. At 25-50 mg, it’s much stronger. Problem? It can cause involuntary muscle movements (extrapyramidal symptoms) in up to 8% of elderly patients. Many hospitals now avoid it in older adults.
- Promethazine (Phenergan) - An antihistamine with anticholinergic effects. Works for motion sickness, but not great for chemo or opioid nausea. Dose: 25 mg IV. Can cause low blood pressure and drowsiness. Not first-line anymore.
- Olanzapine - An antipsychotic repurposed for nausea. Works well for breakthrough nausea, especially in chemo patients. Dose: 2.5-5 mg oral. Fewer movement side effects than metoclopramide. Gaining popularity in elderly and opioid-tolerant patients.
Which One Should You Pick? The Risk-Based Approach
There’s no universal best drug. The right choice depends on your risk level. Doctors use the Apfel Score to figure this out. It looks at four things:
- Female sex (2.2x higher risk)
- Non-smoker (1.9x higher risk)
- History of motion sickness or past PONV (3.1x higher risk)
- Will get opioids after surgery (1.5x higher risk)
Count your points:
- 0-1 risk factors - No preventive meds needed. Just have ondansetron ready if nausea hits.
- 2 risk factors - Use one antiemetic. Droperidol 0.625 mg IV or ondansetron 4 mg IV. Both are equally effective here.
- 3-4 risk factors - Use two drugs. Combine droperidol (0.625-1.25 mg) + dexamethasone (8 mg). This combo cuts PONV risk by over 50% in high-risk patients.
Real-world data from Massachusetts General Hospital shows this approach reduces rescue meds by 32% compared to giving everyone ondansetron.
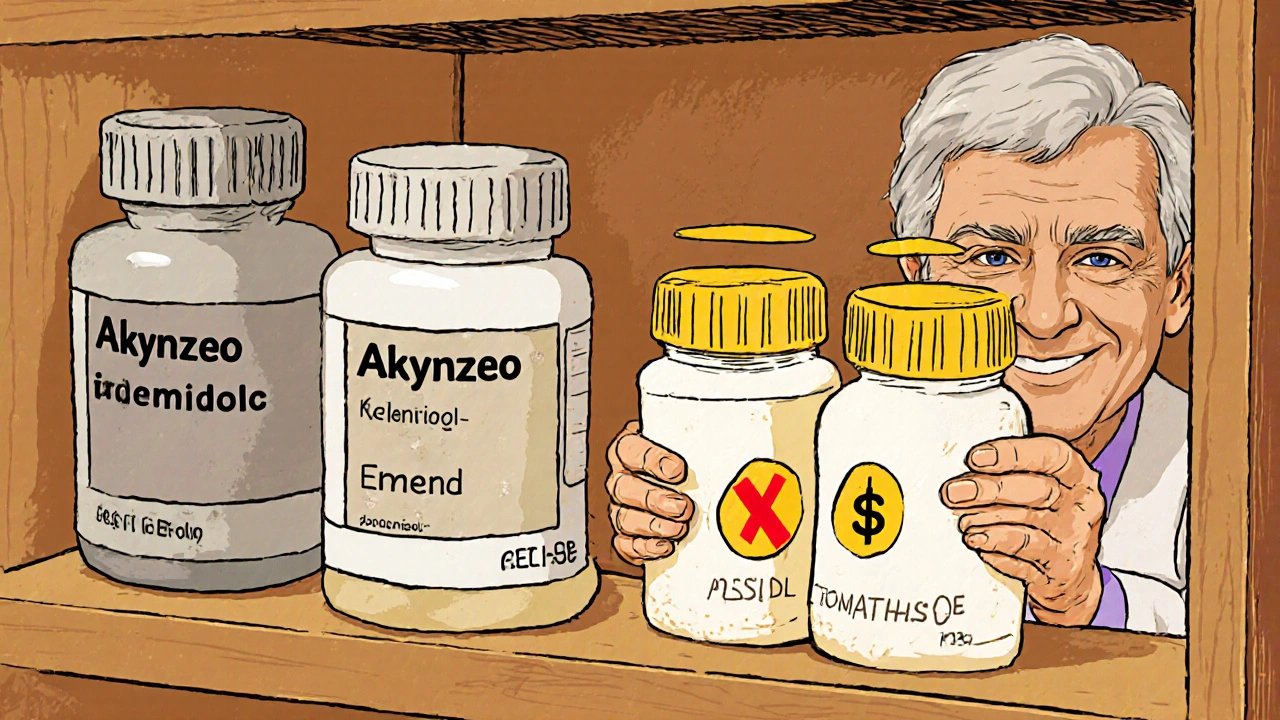
Cost vs. Effectiveness: What’s Actually Worth It?
Brand-name drugs like Akynzeo (netupitant/palonosetron) cost $350 per dose. Generic ondansetron? $1.25. Droperidol? $0.50. Dexamethasone? $0.25.
Here’s the truth: for most people, the cheap ones work just as well. A 2023 study of 6,665 cesarean patients found that low-dose droperidol + dexamethasone performed as well as expensive 5-HT3 blockers. And it saved hospitals over $1,000 per avoided PONV case.
Why do 5-HT3 blockers dominate the market? Because they’re marketed heavily and perceived as “safer.” But safety isn’t just about side effects-it’s about using the right tool for the job. Droperidol has a black box warning for high doses (>1.25 mg), but at low doses, it’s among the safest and most effective options.
What to Avoid
Some antiemetics are outdated or risky for specific groups:
- Dolasetron - Has a FDA black box warning for dangerous heart rhythm changes. Avoid it entirely.
- High-dose metoclopramide (>300 mg/week) - Can cause permanent movement disorders. Stick to 25 mg max for PONV.
- Scopolamine patches - Great for motion sickness, but take 4 hours to work. Useless for sudden post-op nausea.
- Domperidone - Not approved in the U.S. due to cardiac risks. Avoid unless under strict supervision.
Also, don’t give ondansetron to someone with a known long QT syndrome. And never mix it with other drugs that prolong the QT interval without checking.
What’s New in 2025?
There are exciting updates:
- Intranasal ondansetron (Zuplenz) - Approved in 2024. Works for patients who can’t swallow pills or vomit after oral meds. Bioavailability is 89% of IV. Game-changer for ER and post-op settings.
- Rolapitant - An NK-1 receptor blocker. Best for delayed chemo nausea (24-120 hours after treatment). 78.4% success rate vs. 70.6% for placebo.
- Personalized dosing - New research shows people with certain CYP2D6 gene variants metabolize ondansetron slower. These patients need lower doses to avoid side effects. Genetic testing isn’t routine yet-but it’s coming.
Real Patient Experiences
On Reddit, anesthesiologists say: “Droperidol 0.625 mg is my secret weapon for opioid-tolerant patients. No sedation, no fuss.”
On Medscape, one doctor reported: “We switched from metoclopramide to olanzapine in elderly patients. Akathisia dropped from 8% to under 1%.”
Patients on Drugs.com praise ondansetron: “Stopped my nausea in 15 minutes.” But also warn: “Headache every time.”
Cost is a real barrier. One patient wrote: “My insurance won’t cover the new combo drug. I’m stuck with the $1.25 generic-and it works fine.”
Final Takeaway: Safety Isn’t About the Drug-It’s About the Fit
There’s no single best antiemetic. The safest choice is the one that matches your risk, your meds, and your body. Use the Apfel score. Start low with droperidol or ondansetron. Add dexamethasone if you’re high risk. Skip the expensive stuff unless you’ve tried the basics and failed. Watch for side effects-especially in older adults or those with heart issues. And remember: prevention beats rescue every time.
For most people, the answer isn’t more drugs. It’s smarter choices.
What’s the best antiemetic for post-surgery nausea?
For most patients, low-dose droperidol (0.625-1.25 mg IV) or ondansetron (4 mg IV) works best. For those with 3 or more risk factors (female, non-smoker, history of nausea, opioid use), combining droperidol with dexamethasone (8 mg) cuts nausea by over 50%. Ondansetron is preferred if heart rhythm concerns exist; droperidol is better for cost and opioid-tolerant patients.
Is ondansetron safe for everyone?
No. Ondansetron can prolong the QT interval, which increases risk of dangerous heart rhythms, especially in people with congenital long QT syndrome, low potassium, or on other QT-prolonging drugs. It’s also not ideal for elderly patients with kidney issues. Always check heart history before giving it. For high-risk patients, droperidol or olanzapine may be safer alternatives.
Why is droperidol underused despite being effective?
Droperidol was overhyped for safety risks in the early 2000s after a few cases of cardiac events at high doses. But low-dose use (≤1.25 mg) is now proven safe in multiple studies. The problem? Outdated guidelines and fear. Many hospitals still avoid it, even though it’s cheaper and often more effective than ondansetron for PONV. Education and updated protocols are slowly changing this.
Can I use antihistamines like promethazine for chemo nausea?
Not reliably. Antihistamines like promethazine work best for motion sickness and vertigo-related nausea. For chemotherapy-induced nausea, they’re far less effective than 5-HT3 blockers or steroids. Studies show they don’t significantly reduce vomiting in chemo patients. Stick to ondansetron, dexamethasone, or newer NK-1 blockers for cancer treatment.
How long does it take for dexamethasone to work?
Dexamethasone takes 4-5 hours to reach full effect. That’s why it’s not used alone for immediate nausea. It’s always paired with faster-acting drugs like ondansetron or droperidol. Give it at the start of surgery or chemo so it kicks in when nausea peaks-usually 6-24 hours later.
Are generic antiemetics as good as brand names?
Yes. Generic ondansetron, droperidol, and dexamethasone are bioequivalent to brand names in every major study. The only exception is newer combination drugs like Akynzeo or Emend, which have no generics yet. For standard PONV or chemo nausea, generics are the standard of care-effective, safe, and 100x cheaper.

Billy Tiger
October 31, 2025 AT 13:29Why are we still paying for Zofran when droperidol works better and costs less than a coffee
John Concepcion
November 2, 2025 AT 01:58Oh wow so now we're doing cost-benefit analysis on antiemetics like it's a Wall Street spreadsheet? Next you'll tell me we should use aspirin for chemotherapy nausea because it's cheaper
Oliver Myers
November 2, 2025 AT 08:21This is one of the most practical, well-researched posts I've seen in a long time. Seriously. The Apfel Score breakdown alone should be printed and hung in every recovery room. Thank you for cutting through the noise and giving us real, actionable info. I'm sharing this with my entire team tomorrow.
Caitlin Stewart
November 2, 2025 AT 23:28I work in oncology and we switched to olanzapine for elderly patients last year. The difference in akathisia rates was night and day. Also, they actually tolerate it better than metoclopramide. It’s not perfect, but it’s a huge step forward. I wish more hospitals were doing this.
Pritesh Mehta
November 4, 2025 AT 12:07Let us not forget the deeper metaphysical truth here: the pharmaceutical industry does not cure, it commodifies suffering. Ondansetron is not medicine-it is a corporate construct wrapped in clinical jargon to extract value from human vulnerability. Droperidol, on the other hand, is a quiet rebellion against the algorithmic absurdity of modern healthcare. It costs less, works faster, and refuses to be branded. In its simplicity lies a kind of Zen-like resistance to the capitalist medical machine. We are not treating nausea-we are resisting the ontological violence of overpriced pills. The Apfel Score is not a clinical tool; it is a mirror held up to the absurdity of risk stratification in a system that values profit over presence. And yet… we still use it. Because even rebellion must be measured. And quantified. And billed.
Alex Sherman
November 5, 2025 AT 14:28People still use promethazine? That's like using a horse and buggy to get to the airport. The FDA black box warnings are there for a reason and if you're still prescribing it for chemo nausea you're either lazy or didn't read the last 20 years of literature. Also why is this even a debate? The data is 100% clear
Katie Ring
November 7, 2025 AT 03:45It’s fascinating how we’ve reduced human suffering to a checklist of risk factors and drug algorithms. But behind every PONV score is someone trembling in a hospital bed, afraid to swallow water because they know what comes next. The real innovation isn’t in the drug-it’s in the way we stop seeing patients as data points and start seeing them as people who just want to stop feeling like they’re drowning. Droperidol may be cheap, but compassion? That’s priceless. And we’re running out of it.
Adarsha Foundation
November 8, 2025 AT 22:14Thank you for sharing this. I’m a nurse in Mumbai and we don’t always have access to the latest drugs, but we’ve been using low-dose droperidol and dexamethasone for years with great results. It’s reassuring to see our practice validated by U.S. data. Maybe we’re not so far behind after all.
Emmalee Amthor
November 10, 2025 AT 09:29Wait so olanzapine is actually good for nausea? I thought it was just for schizophrenia? I'm so used to hearing about side effects I didn't even consider it could help. This changes everything. I'm gonna ask my doc about it next time I'm in for chemo. Thank you for this
Leslie Schnack
November 11, 2025 AT 14:23Is there any data on how often droperidol is actually given at the correct low dose in real hospitals? I’m guessing a lot of providers avoid it because they’re scared of the black box warning and just give ondansetron by default, even when it’s not the best choice. We need better education-not just guidelines.