Comorbidity Drug Risk Calculator
Assess Your Medication Risk
This tool estimates your risk of adverse drug reactions based on your health conditions and current medications. Results are for informational purposes only and should not replace professional medical advice.
Risk Assessment Results
When you take a medication, you expect it to help. But if you’re managing more than one health condition, the risk of something going wrong goes up-sometimes dramatically. It’s not just about the drug itself. It’s about how your body, already stressed by other illnesses, reacts to it. This is where comorbidities change everything.
What Exactly Are Comorbidities?
Comorbidities aren’t just having two or more health problems. They’re conditions that interact in ways that make treatment harder and riskier. Think of someone with diabetes and heart disease. Or someone with chronic pain who also has depression and kidney trouble. These aren’t separate issues-they’re connected. And when you add medications into the mix, the connections turn into dangers.Studies show that people with comorbidities are nearly three times more likely to have an adverse drug reaction than those with just one condition. In one large study, 19.6% of patients with multiple health problems had a bad reaction to a medication. For those without comorbidities? Just 7.6%. That’s more than double the risk.
Why Do Existing Conditions Make Drugs More Dangerous?
Your body processes drugs in predictable ways: it absorbs them, moves them around, breaks them down, and gets rid of them. But when you have diseases like liver failure, kidney disease, or heart failure, those processes get messed up.Take liver disease. The liver uses enzymes-especially the CYP450 system-to break down most medications. When the liver is damaged, those enzymes work at 30% to 50% less capacity. That means drugs stick around longer. A normal dose becomes too strong. A drug meant to last 8 hours might last 16. That’s how you get dizziness, confusion, or even falls.
Kidney problems do something similar. If your kidneys can’t filter properly, drugs that are cleared through urine build up. Blood pressure meds, antibiotics, and painkillers like ibuprofen can reach toxic levels without warning. Even if your doctor prescribed the right dose, your body can’t handle it like it used to.
It’s not just about how your body handles the drug. It’s also about how your disease changes your sensitivity to it. Someone with Parkinson’s might develop severe tremors from a low dose of an antipsychotic that’s fine for others. Someone with heart failure might crash into low blood pressure from a standard dose of a beta-blocker. These aren’t mistakes. They’re predictable outcomes of disease-drug interactions.
The Polypharmacy Trap
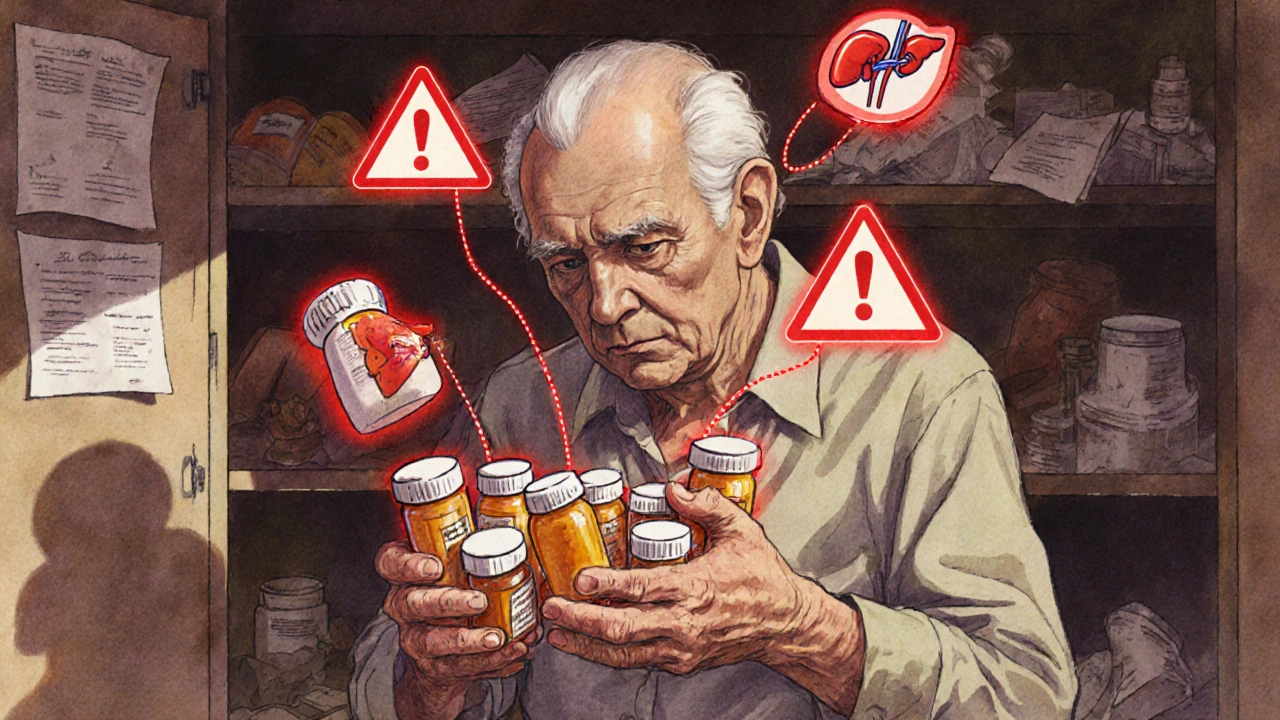
Most people with multiple conditions end up on multiple medications. In fact, 85% of adults over 65 have two or more chronic diseases-and nearly half of them take five or more drugs daily. That’s polypharmacy. And it’s where things get really dangerous.Each new drug adds a new chance for interaction. One drug might slow down how another is broken down. Another might make your kidneys work harder, which is bad if you already have kidney disease. Studies found that 47% of elderly patients on multiple drugs had at least one dangerous drug-drug interaction. Over a third of those were major-meaning they could cause permanent harm or death.
In cancer patients, the numbers are even worse. In one study of 100 patients, 65 had drug interactions. More than a third were high-risk. And these weren’t theoretical. They led to hospital stays, treatment delays, and extra costs of $1,200 to $2,500 per incident.
It’s not just the number of pills. It’s the types. Anticoagulants, antidepressants, blood pressure drugs, and painkillers are the most common culprits. Combine them with conditions like diabetes, liver disease, or dementia, and the risk skyrockets.
What Symptoms Should You Watch For?
The side effects in people with comorbidities aren’t random. They follow patterns.The most common reactions? Weakness (36% of cases), dizziness (12%), headaches (7%), nausea (5%), vomiting (4%), and trouble sleeping (3%). These aren’t just annoying-they’re red flags. Dizziness can lead to falls. Weakness can make it hard to get up or walk. Nausea can lead to dehydration and malnutrition.
And here’s something important: the symptoms you see might not look like the drug’s usual side effects. A statin might normally cause muscle pain. But in someone with kidney disease, it might cause confusion or extreme fatigue instead. That’s because the disease changes how the drug affects your brain and muscles.
Who’s at the Highest Risk?
It’s not just older adults. But they’re the most affected. The Beers Criteria-a list of medications that are risky for seniors-shows that nearly half of older patients are prescribed at least one drug they shouldn’t be. Women over 75 are almost three times more likely to get these unsafe prescriptions than younger patients.People with substance use disorders are also at high risk. Over 75% of those in treatment for alcohol or opioid use also smoke. That means their liver is already under stress, and their heart is already damaged. Add medications for depression, pain, or heart disease, and the mix becomes volatile.
Chronic pain patients are another group at risk. About 10% misuse their opioid prescriptions. That’s not just addiction-it’s a dangerous feedback loop. The drug meant to treat pain ends up causing more health problems, which leads to more drugs, which leads to more side effects.
How Doctors Are Trying to Fix This
The system is catching on. Clinical pharmacists who review all your medications-every pill, every supplement-have cut adverse reactions by 22% in studies. Electronic health records now flag dangerous combinations when a doctor tries to prescribe. Some systems even adjust warnings based on your kidney or liver function.Tools like STOPP/START help doctors decide what to stop and what to start. Instead of just adding more pills, they ask: “Is this still helping? Is it worth the risk?” In one trial, using these guidelines reduced hospital stays due to bad reactions by 17%.
The NIH launched a new database in 2024 that tracks 12 million patient records. It’s already found 217 new dangerous drug-comorbidity pairs. Machine learning models now predict bad reactions with 89% accuracy-far better than older methods.
And the FDA now requires drug makers to test how their medications affect patients with common comorbidities. In 2018, only 42% of new drug applications included this. Now it’s 78%.
What You Can Do
You don’t have to wait for the system to fix itself. Here’s what works:- Keep a full list of everything you take. Include prescriptions, over-the-counter meds, vitamins, and herbal supplements. Update it every time something changes.
- Ask your doctor or pharmacist: “Could this interact with my other conditions?” Don’t assume they know. Many doctors miss interactions because they’re focused on one disease at a time.
- Watch for new symptoms. If you start feeling dizzy, weak, or confused after starting a new drug, don’t brush it off. Call your provider.
- Request a medication review. Ask for a pharmacist-led review at least once a year-especially if you take five or more drugs.
- Bring all your meds to appointments. Don’t just describe them. Show them. A pill bottle tells more than a list.
The Big Picture
By 2030, 90% of adults over 65 will have two or more chronic conditions. That’s not a future problem-it’s happening now. Medications aren’t getting safer. They’re getting more complex. And the people who need them most are the ones most likely to be harmed by them.Comorbidities don’t just add up. They multiply risk. A single drug might be fine. Two might be okay. But five, ten, or more? That’s where the danger lives. The solution isn’t just better drugs. It’s smarter prescribing, better communication, and more awareness.
If you or someone you care about is managing multiple conditions, don’t accept side effects as normal. Ask questions. Push for reviews. Demand clarity. Because when it comes to drugs and comorbidities, the difference between safety and harm isn’t always obvious-but it’s always there.
Can a single health condition really make a drug unsafe?
Yes. Even one chronic condition like kidney disease, liver cirrhosis, or heart failure can change how your body absorbs, breaks down, or reacts to a drug. For example, a standard dose of a blood pressure medication might cause dangerous low blood pressure in someone with heart failure because their body can’t handle the extra stress. It’s not about the drug being bad-it’s about your body’s changed ability to manage it.
Why do older adults have more problems with medications?
Older adults are more likely to have multiple chronic conditions, reduced kidney and liver function, and take more medications. They’re also often excluded from clinical trials, so the safety data for their age group and health status is limited. As a result, doctors often prescribe based on data from younger, healthier people-which doesn’t reflect their reality.
Are over-the-counter drugs safe if I have comorbidities?
Not always. Many OTC meds like ibuprofen, antacids, sleep aids, or cold medicines can interact with prescription drugs or worsen conditions. For example, ibuprofen can damage kidneys in people with diabetes or high blood pressure. Antihistamines can cause confusion in those with dementia. Always check with your pharmacist before taking anything new.
How do I know if a side effect is from a drug or my condition?
Track when symptoms started. If weakness, dizziness, or nausea began shortly after starting a new medication, it’s likely related. But because comorbidities can cause similar symptoms, the best approach is to share your full list of meds and symptoms with your provider. They can compare timelines and rule out other causes.
Can I stop taking a medication if I think it’s causing side effects?
Never stop a prescribed medication without talking to your doctor. Some drugs, like blood pressure or antidepressant medications, can cause serious rebound effects if stopped suddenly. Instead, report the side effect and ask if the dose can be adjusted or if there’s a safer alternative.
Is there a tool to check for drug-comorbidity interactions?
Yes. Many electronic health records now flag risky combinations. You can also use free tools like the American Geriatrics Society’s Beers Criteria list or the NIH’s Comorbidity-Drug Interaction Knowledgebase. But the most reliable check is always a conversation with your pharmacist or provider who knows your full medical history.
Tim H
October 28, 2025 AT 19:42Matt Renner
October 29, 2025 AT 14:24Ifeoluwa James Falola
October 31, 2025 AT 00:48Julie Lamb
November 1, 2025 AT 04:40Ramesh Deepan
November 2, 2025 AT 22:59Wayne Rendall
November 4, 2025 AT 04:41april kakoske
November 4, 2025 AT 17:36Adam Phillips
November 4, 2025 AT 21:03Umesh Sukhwani
November 6, 2025 AT 00:55Dale Yu
November 7, 2025 AT 22:36Vishnupriya Srivastava
November 8, 2025 AT 17:04May Zone skelah
November 9, 2025 AT 11:20Rishabh Jaiswal
November 10, 2025 AT 11:23Pradeep Meena
November 11, 2025 AT 13:41